Abstract
Clevidipine is a new calcium channel blocker of the dihydropyridine class that is characterized by its ultra-short onset of action, vascular selectivity, small volume of distribution and extremely high clearance that coupled together result in an extremely short half-life of approximately 1 minute therefore permitting a rapid titration to the desired effect. Structurally similar to other dihydropyridines, clevidipine has an extra ester link that allows its rapid hydrolization to its inactive carboxylic acid metabolite in blood and extravascular tissues. Clevidipine’s metabolites are then primarily eliminated through urine and fecal pathways. Clevidipine does not affect cytochrome P450 (CYP) enzymes and no clinically significant drug interactions have been determined. In trials like the ESCAPE trials, ECLIPSE, and VELOCITY, clevidipine demonstrated a significant improvement in the management of acute hypertension when compared to placebo as shown in both ESCAPE trials. The ECLIPSE trial compared clevidipine to other drugs currently used in the management of acute hypertension, such as sodium nitroprusside, nitroglycerine and nicardipine; clevidipine was superior to all three agents; in providing blood pressure support, safety and tolerability clevidipine also showed a significant reduction in mortality rate (4.7% vs 1.7%, P =0.0445) when compared to sodium nitroprusside. In the VELOCITY trial clevidipine demonstrated a reduction in blood pressure of 6% at the 3 minute mark, 15% within 9.5 minutes and 27% at the 18 hour mark.
Introduction to the management of acute hypertension
Chronic hypertension is among the most common medical conditions, affecting approximately 72 million people, which accounts to almost 30% of the population older than 20 years in the United States alone.Citation1 Even though the chronic form of hypertension is by far the most common, it is the acute form of hypertension that presents a far greater challenge, with more and more frequent and severe complications and poorer short-term prognosis than chronic hypertension. Acute elevations in blood pressure (BP) may result in severe clinical conditions such as hypertensive encephalopathy, acute aortic dissection, acute myocardial infarction, acute renal failure, intracranial hemorrhage, acute heart failure, and eclampsia, among others.Citation2
Hypertensive crises are most commonly encountered by emergency department (ED) personnel in a clinical setting, occurring in up to 27.5% of all nonsurgical emergencies presenting to the ED and accounting to up to 3% of all emergency room visits.Citation3
Some of the most commonly used agents are intravenous short-acting vasodilators like sodium nitroprusside and nitroglycerin. Both are used in the management of acute hypertension due to high vascular resistance; however, both of these agents present multiple adverse effects that hinder their utility.Citation4–Citation7
Clevidipine is a relatively new, ultra-short acting, dihydropyridine, calcium channel blocker.Citation8 Clevidipine’s effectiveness is due, in part, to its selectivity for arteriolar dilatation without affecting myocardial contractility and its lack of effect on venous capacitance.Citation9 Characteristics like rapid onset of effect, high clearance, and small volume of distribution make it a promising agent for the management of acute severe hypertension.Citation10
The Seventh Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood PressureCitation11 defined a ‘hypertensive emergency’ as an acute elevation in systolic blood pressure (SBP) and diastolic blood pressure (DBP) associated with end-organ damage; while an acute elevation of SBP and/or DBP without end-organ damage can be defined as a ‘hypertensive urgency’.Citation11
The swift differentiation between a hypertensive emergency and hypertensive urgency is extremely important in the clinical settings, as the presence or lack of end-organ damage will dictate the urgency and aggressiveness of treatment. In a hypertensive emergency, the rapid reduction and control of BP is essential to avoid further end-organ damage,Citation11 while in a hypertensive urgency the BP control can be achieved within the first 24 to 48 hours after its presentation, with minimal or no change in outcome.Citation12,Citation13
It is estimated that approximately 1% of chronically hypertensive patients will experience a hypertensive crisis in their lifetime.Citation14 Risk factors for hypertensive crises are similar to chronic hypertension, including old age, male gender, African American race, tobacco use, obesity, and diabetes mellitus.Citation15,Citation16 The morbidity and mortality of hypertensive crises is directly dependent on the degree of target organ damage, adequate BP control, and adherence to treatment. In patients who do not receive medical treatment the mortality rate at 1 year can be as high as 79%Citation17 and among all patients who present a hypertensive crises, there is a 5-year survival rate of 74%.Citation18
Clinical assessment and initial management of acute hypertension
Patients who present to the ED with a hypertensive emergency will usually have a complaint that is directly related to the presence and degree of end-organ damage; most commonly chest pain, dyspnea and altered mental status.Citation3
Patients who present to the ED with a hypertensive emergency need an immediate reduction in BP to reduce the risk and/or progression of end-organ damage; a general goal is the reduction of mean arterial pressure (MAP) by 15% to 20% within the first 2 hours of initial evaluation. This is in contrast to hypertensive urgencies where there is no need for a rapid reduction in BP, and the target BP can be achieved over a period of 24 to 48 hours. Citation19 In fact, unnecessary rapid reduction is not without risk, and correction of severely elevated BP can markedly reduce perfusion, causing ischemia and infarction, and may be associated with significant morbidity in hypertensive urgency.Citation20–Citation24 Although BP must be reduced in these patients, it must be lowered in a slow and controlled fashion to prevent organ hypoperfusion.
Hypertensive crisis in the surgical setting is an extremely common occurrence, affecting up to 25% of all patients that undergo surgery;Citation25 it is particularly common during cardiac surgery, major vascular surgery (ie, carotid end-arterectomy, aortic surgery), neurosurgery, head and neck surgery, renal transplantation, and major trauma, eg, burns or head injury). Postoperative hypertension (BP ≥ 190 mmHg and/or diastolic BP 100 mmHg on two consecutive readings after surgery)Citation26,Citation27 could result in creating significant adverse sequelae in both cardiac and noncardiac patients. Depending on the population examined, the incidence of postoperative hypertensive crises varies from 4% to 35% of patients shortly after a surgical procedure.Citation28–Citation30 Greater attention should be given to precise perioperative BP control, as excursions outside a targeted BP range have correlated with increased risk of 30-day mortalityCitation31 and increased odds ratio for postoperative death to 3.8.Citation25
Among the numerous agents currently utilized for the treatment of acute hypertension none have the ideal combination of vascular selectivity, rapid onset and offset of action coupled with a low incidence of side effects. Nitroprusside has long been among the most utilized agents for rapid BP control. A short-acting intravenous vasodilator with well demonstrated efficacy, nitroprussides utility is limited due to several disadvantages that include low arteriolar selectivity, toxicity, and side effects such as tachyphylaxis, reflex tachycardia, and rebound hypertension.Citation32 An alternative vasodilator, nitroglycerin is not an ideal agent for first-line treatment due to lower efficacy than nitroprusside, fairly common occurrence of hypotension, tachyphylaxis, and reflex tachycardia.Citation1,Citation17,Citation19
Another group of medications currently available for acute BP control is calcium channel blockers, particularly those of the dihydropyridine class. These agents have a demonstrated efficacy and vascular selectivity.
Review of pharmacology of clevidipine
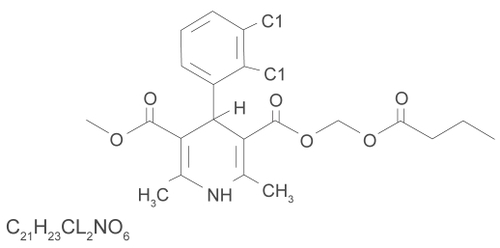
Clevidipine is the latest generation calcium channel blocker of the dihydropyridine family, with characteristics of arterial selectivity, extremely rapid onset of action and high rate of clearance (see and ).Citation9,Citation33–Citation35
Table 1 Pharmacology of clevidipine
Clevidipine comes in a lipid emulsion, and the FDA recommends tube changes every 4 hours. There has been speculation that the clevidipine lipid emulsion may result in increased triglyceride levels. However, there have been no complications reported from the lipids. In the ECLIPSE trials the investigators stated that changes in triglyceride levels were similar for clevidipine and comparator agents.Citation31 Moreover, in the VELOCITY trial, long-term infusion of clevidipine lipid emulsion did not alter the median percentage change in triglyceride levels, and a post-hoc analysis demonstrated that there was no relationship between clevidipine dose and change in triglyceride levels from baseline to 6 hours after clevidipine treatment.Citation36
Pharmacokinetics
Clevidipine is structurally similar to other dihydropyridines; however an extra ester link allows its rapid hydrolization to its inactive carboxylic acid metabolite in blood and extra-vascular tissues. Clevidipine’s metabolites are then primarily eliminated through urine and fecal pathways.Citation34 Clevidipine has a very short half-life of approximately 1 minute Citation10,Citation35 secondary to its high clearance (median blood clearance is 0.125L/min/kg]) Citation35 and a small volume of distribution of 0.51 to 0.58L/kg. These characteristics allow a more rapid titration to the desired effect, as the drug achieves steady blood concentrations rapidly after the initiation of an infusion,Citation37,Citation38 and a rapid decrease on BP effect after the infusion is suspended.Citation8 After discontinuation or reduction of the infusion, in most patients, full recovery of BP is obtained in under 15 minutes.Citation39
Clevidipine does not affect cytochrome P450 (CYP) enzymes and no clinically significant drug interactions have been determinedCitation39 increasing its margin of safety for drug interactions.
Pharmacodynamics
Clevidipine has an extremely rapid onset of effect in 2 to 3 minutes.Citation35 It exerts its effect by inhibiting transmembrane influx of calcium ions through the voltage-dependent L-type calcium channels.Citation40 Like similar drugs of the dihydropyridine family, such as nicardipine and nifedipine, a key characteristic of clevidipine is its arterial dilation selectivity. Vascular selectivity allows the decrease of BP by reducing vascular resistance but not causing venous dilation and therefore not affecting cardiac preload; thus it has minimal effect on stroke volume, cardiac output, or heart rate.Citation41
A study of the pharmacokinetics and arteriovenous differences in clevidipine concentration after a short- and a long-term intravenous infusion in healthy volunteers was performed by Ericsson et alCitation42 In this study. The MAP and heart rate were monitored and recorded before (ie, baseline), during, and after short and 24-hour infusions of clevidipine. The MAP measurements after cessation of the 24-hour infusion did not differ from those obtained at baseline, before starting of infusion. After short 20-minute infusion clevidipine reduced MAP from approximately 90 to 75 mmHg, and increased heart rate from approximately 53 to 75 beats/min, at steady-state conditions. After cessation of the infusion, MAP and heart rate returned to predose measurements within 10 minutes for all subjects.
Clevidipine trials
ESCAPE-1
The Efficacy Study of Clevidipine Assessing Its Preoperative Antihypertensive Effect in Cardiac Surgery (ESCAPE-1) trial of 105 patients scheduled for cardiac surgery that were either diagnosed with hypertension or recently had hypertension, who were randomized into 2 groups. An intervention cohort received a 0.4 to 0.8 μg/kg/min infusion of clevidipine while the control group received an infusion of 20% lipid placebo emulsion. The clevidipine cohort had a significantly lower rate of treatment failure, defined as failure to reduce SBP by more than 15% from the baseline BP or the termination of infusion, when compared to placebo (7.5% vs 82.7%; P <0.0001). Of the patients who received clevidipine, 90% reached the target BP at a median time of 6 minutes, while in the placebo group the median time was unable to be established because so few patients actually reached the target BP.Citation33,Citation43 The authors of ESCAPE-1 concluded that clevidipine was effective in quickly decreasing preoperative BP to targeted BP levels and was well tolerated in most patients.
In ESCAPE-1, clevidipine was shown to be well tolerated with an adverse event (AE) profile similar to that of placebo and consistent with outcomes expected in cardiac surgery.Citation44,Citation45 A modest increase in heart rate was observed during clevidipine administration, as has been reported with other intravenous dihydropyridinesCitation46,Citation47 and in studies of clevidipine in essential hypertension and postcardiac surgery.Citation10,Citation32
A limitation of ESCAPE-1 was that it could not be designed to evaluate clevidipine during surgery for ethical reasons (ie, not treating hypertension), and therefore involved a somewhat artificial preoperative treatment strategy. Moreover, another potential study limitation was the influence of premedication on arterial BP. Because ESCAPE-1 was designed as an acute assessment of antihypertensive treatment over 30 minutes, and included comparison of active treatment to placebo, it was unlikely that any effects of pre-medication on study results would have gone unnoticed.
ESCAPE-2
The Efficacy Study of Clevidipine Assessing Its Postoperative Antihypertensive Effect in Cardiac Surgery-2 (ESCAPE-2) is a double-placebo controlled trial that examined the safety and efficacy of clevidipine in post cardiac surgery patients with hypertension. The trial randomized 110 patients meeting the criteria for a diagnosis of postoperative hypertension into two groups; one received an infusion of clevidipine at 0.4 to 0.8 μg/kg/min, while the second group received a 20% lipid emulsion for a maximum of 1 hour. The clevidipine group had a better success rate (91.8%; P <0.0001), defined as the absence of treatment failure, compared to placebo which had a success rate of 20.4%. Patients treated with clevidipine also showed a considerably greater reduction in mean arterial pressure than the placebo group 2 minutes after the infusion of either clevidipine or placebo (P =0.0004). In the clevidipine group there was a 5.7 mmHg reduction, compared to 0.1 mmHg with placebo. The efficacy of clevidipine was most evident when comparing the greatest mean change. The greatest mean change was 28.1 mmHg with clevidipine, compared to 8.9 mmHg for placebo (P <0.0001). Citation48 AE rates were similar for both treatment groups with no clinically significant increases in heart rate or acute adverse hemodynamic events. In the ESCAPE-2 trial, clevidipine was effective and safe in the rapid management of acute hypertension related to cardiac surgery.
VELOCITY
The Prolonged Infusion of Clevidipine Results in Safe and Predictable Blood Pressure Control in Patients with Acute Severe Hypertension (VELOCITY) trial consisted of an open-label, single arm, multicenter study that enrolled 126 patients that presented either to the emergency department or intensive care unit with acute hypertension. The goal of VELOCITY was to ascertain the percentage of patients whose SBP decreased below a preset intended target after an initial dose of 2 mg/hour within a period of 3 minutes (safety endpoint, ie, overshoot rate), as well as the percentage of patients that reached an individualized target range within 30 minutes (efficacy endpoint). In this trial, clevidipine showed a rapid and effective reduction in BP, with a decrease on average of 6%, corresponding to 12 mmHg within the 3-minute time period, and a total reduction of 15% within 9.5 minutes. The trial not only demonstrated clevidipine’s efficacy in the short term, but it also showed the efficacy of clevidipine with a longer-term infusion, as there was a 27% reduction in BP 18 hours after the initiation of the infusion (a reduction equivalent to 55 mmHg).Citation36
In the VELOCITY safety population, 39.7% of patients experienced at least 1 AE after clevidipine initiation, and 8.7% of patients experienced at least 1 serious AE. Headache was the most frequently reported AE, with an overall incidence of 6.3% (8/126), followed by nausea (4.8%; 6/126), chest discomfort (3.2%; 4/126), and vomiting (3.2%; 4/126).
Patients in the safety population most often had AEs categorized by the investigator as mild (13.5%) or moderate (17.5%) in severity, as opposed to severe (8.7%). Safety patients most often had AEs assessed by the investigator as unrelated to clevidipine (30.2%) vs related (9.5%). Two of 126 patients complained of pruritus at the infusion site. The frequency of AEs, severity, and possible relationship to clevidipine were similar in the long-term cohort. The VELOCITY trial also ascertained that clevidipine is both safe and effective in patients with underlying severe hypertension, heart failure, or renal dysfunction. These data are compatible with data obtained from both ESCAPE trials. The authors concluded that clevidipine is a safe and effective drug in the rapid management of severe hypertension at a nonweight-based dose of 2 mg/hour followed by simple infusion titration to desired BP during 18 hours of more.
Limitations of the VELOCITY trial are that the trial was performed as an open-label uncontrolled study. However, it was designed to permit the use of concomitant intravenous antihypertensive therapy at any time if needed; thus, each patient effectively served as his or her own control. The definition for severe hypertension used in this study (SBP >180 mmHg and/or DBP >115 mmHg) was developed according to clinical experience. No universally accepted definition exists for severe hypertension.Citation17,Citation49 The patient population studied represented a mixture of hypertensive urgencies and emergencies. It is possible, therefore, that the patients without acute end-organ injury would not all have received intravenous antihypertensive therapy in routine clinical practice but would have been treated with oral antihypertensive agents.
VELOCITY subset analyses
VELOCITY trial subset analyses have been performed in patients with renal dysfunction and acute heart failure. In subset of the Velocity trial, a safety and efficacy analysis of clevidipine used in 24 patients with moderate to severe renal dysfunction (>50% on dialysis)Citation50 found clevidipine rapidly and effectively lowered BP, was not associated with excessive or precipitous drops in BP, and had similar results in patients with or without renal dysfunction. Targeted BP control was rapidly achieved in 8.5 minutes and was maintained for the specified 18 hours duration after which most patients (88%) effectively transitioned to oral therapy within 6 hours of clevidipine termination. In this high risk subpopulation most AEs were assessed as unrelated to clevidipine treatment. This supports the relative safety of this product. The safety results of this subgroup analysis in patients with renal dysfunction are also consistent with the results of the overall VELOCITY trial.Citation36
The safety and efficacy of clevidipine was also assessed in a VELOCITY subset analysis of patients with acute heart failure. In this group of 19 patients presenting with acute heart failure, the median time or treatment with clevidipine to a patient-specific prespecified initial target range (ITR) of SBP to be achieved within 30 minutes was 11.3 minutes. Most patients (94%) reached ITR within 30 minutes. No patient had hypotension below the ITR and heart rate remained stable. At 18 hours, 16/19 patients had received continuous clevidipine infusion and their SBP was reduced by mean of 50 mmHg (25%) from baseline. There were no treatment-related AEs, or AEs that led to clevidipine discontinuation. Likewise, the results of this subgroup analysis in patients with acute heart failure are also consistent with the results of the overall VELOCITY trial.Citation36
ECLIPSE
Lastly, the Evaluation of Clevidipine in the Perioperative Treatment of Hypertension Assessing Safety Events (ECLIPSE) trial examined 1964 patients scheduled to undergo cardiac surgery that were randomized into 3 groups that would receive either clevidipine vs nicardipine, clevidipine vs nitroglycerin, or clevidipine vs nitroprusside. Prior to surgical intervention, the patient’s BP was constantly monitored and study drug was administered as needed. ‘Blood pressure excursions’ were defined as how long and how much the systolic BP was above or below individualized predetermined BP ranges.Citation43 In all three analyses, clevidipine was superior to the comparator drugs in properly controlling BP, with almost half of the BP excursions in relation to the other agents (3.8 vs 7.8 mmHg × min/hour). Clevidipine also had the narrowest SBP range in pre- and postoperatively (105 to 145), and during surgery (93 to 135).
For specific comparisons, clevidipine had almost half the BP excursions vs nitroglycerin (4.14 vs 8.87 mmHg × min/hour) and nitroprusside (4.37 vs 10.5 mmHg × min/hour). However, when clevidipine was compared to nicardipine, there was no significant difference in the pre/postoperative period in BP excursions (1.76 mmHg × min/hour vs 1.79 mmHg × min/hour). Citation43
Overall, clevidipine reduced BP to target in more than 90% of patients with perioperative HTN.Citation33,Citation43 The ECLIPSE trial demonstrated that clevidipine not only has superior BP control than other drugs, but also showed a significant reduction in 30-day mortality rate compared to nitroprusside (4.7% vs 1.7%, P =0.0445). There were no significant differences in incidence of cerebrovascular accident, heart attack, or kidney damage.Citation43 The ECLIPSE trial is consistent with the ESCAPE 1 and 2 and VELOCITY trials showing that clevidipine is a safe and effective drug for the treatment of acute hypertension, but also demonstrated that clevidipine offers a more precise and titratable BP control than nitroprusside and nitroglycerin.
The incidence of the most commonly reported AEs, including atrial fibrillation and sinus tachycardia, were similar for clevidipine and the comparator drugs. Atrial fibrillation was reported as an AE at an incidence of 33.6% vs 32.0% (clevidipine vs nitroglycerin); 36.1% vs 32.2% (clevidipine vs sodium nitroprusside); and 35.6% vs 35.2% (clevidipine vs nicardipine), all P = NS. The incidences of serious AEs were similar among all groups. Clinical laboratory data including change in triglyceride levels were similar between clevidipine and the comparator drugs. In this trial, clevidipine administration did not cause an increase in triglyceride levels.
Limitations of the study include the open-label design. Moreover, clevidipine was dosed in a standard fashion at all study sites, while comparator drugs were administered according to institutional practice.
Clevidipine dosing and titrating
Clevidipine is easy to use and is initiated with a nonweight-based starting dose followed by titration to a target BP. It may be administered as loading dose of 1 to 2 mg, followed by repeated incremental doubling of the dose at 90-second intervals until the desired BP is achieved. As the BP approaches goal, the dose should be increased by less than double and the time between dose adjustments lengthened to every 5 to 10 minutes. An increase of approximately 1 to 2 mg/hour will generally produce an additional 2 to 4 mmHg decrease in SBP. The desired therapeutic response for most patients occurs at doses of 4 to 6 mg/hour. Patients with severe hypertension may require doses up to 32 mg/hour. Citation39 Clevidipine is safe to administer by either central or peripheral line, providing convenience and flexibility. When treatment with clevidipine is no longer required, patients can be easily and successfully transitioned to oral therapy (see ).
Table 2 Frequency of adverse effects
Safety and tolerability
The ESCAPE, ECLIPSE and VELOCITY trials demonstrated that clevidipine is a safe and tolerable drug with few adverse effects. The ESCAPE-1 and -2 trials showed that the most common and severe adverse effect was a slight increase in heart rate without clinical significance. Likewise, the VELOCITY trial reported no serious AEs attributable to clevidipine, including rebound hypertension. Finally, in the ECLIPSE trial there were no differences in death or adverse outcomes at the time of hospital discharge to day 7 among any of the treatment groups. Across all pivotal studies, it has been determined that clevidipine is a safe and effective treatment for patients with severe hypertension, those scheduled for cardiac surgery, those with acute hypertension undergoing cardiac surgery, and in the rapid treatment of acute postoperative hypertension after cardiac surgery.Citation33,Citation36,Citation43,Citation48
Patient-focused perspectives
The use of clevidipine is complicated by remarkably few side effects compared to other medications commonly used to treat these conditions. Despite its arterial selective vasodilation effects, clevidipine use has relatively little association with cephalgia. While nitroglycerin use in the ED commonly requires the coadministration of intravenous narcotics for intractable headache, this is much less common with clevidipine.
Clevidipine use has occasionally been reported to be associated with thrombophlebitis; however as reported in the package insert, this occurs at a rate approximating 1%, and as such may be considered a relatively rare side effect.Citation39
An important consideration of the use of clevidipine is the potential for interaction with other agents. Because of its very short half-life, and its unique metabolic pathway that does not require hepatic or renal function, interactions are generally limited, and if occur can be terminated rapidly. Consideration for the potential of beta blocker withdrawal should be evaluated in patients on long-term beta blockers, who have them withheld while on clevidipine and develop unexplained tachycardia.
Because clevidipine is formulated within a 20% fat emulsion (0.2 g/mL) some attention to total lipid administration during a 24-hour period should be given. In conditions where there is significantly impaired lipid metabolism (eg, severe hyperlipidemia) or pathology that may potentially be worsened by the increase in lipid load (eg, acute pancreatitis), clevidipine use should be monitored.
Limitations
The paper reviews the use parenteral clevidipine for the acute control of BP in the critically ill patient, and in particular, reviews the results of pivotal clevidipine trials. Therefore, the paper is limited to reviewing the data originally presented in the published manuscripts of each trial and the approved prescribing information. No additional or new data are provided.
Conclusion
With its extremely fast onset and offset of action and arteriolar selectivity, as well as its high effectiveness, ease of use, and dosing, clevidipine is a very promising new agent in the management of acute hypertension. Clevidipine is structurally similar to other dihydropyridines; however it contains an extra ester link that allows the rapid hydrolization in blood and extravascular tissues. Since clevidipine is a pure after-load reducer, it does not affect central venous pressure and therefore does not affect preload and cardiac output. Trials like ESCAPE, ECLIPSE, and VELOCITY have shown that clevidipine is a very safe, tolerable, and effective in patients with severe hypertension, heart failure, or renal dysfunction. In addition, clevidipine is easy to use and monitor via BP cuff, reducing the need for more invasive monitoring. These characteristics, coupled with its small volume of distribution, result in the rapid and easy titration to the desired effect.
Acknowledgments
Acknowldgments
The authors would like to thank Richard Pistolese for his assistance in the preparation and review of this manuscript.
Disclosures
The authors have not received any support in the form of equipment, drugs, or grants related to this manuscript. Drs Angeles, Soto, and Lumb have no conflicts of interest to disclose. Drs Peacock and Varon have served as consultants for The Medicines Company. Dr Peacock has received honoraria for lectures from Abbott, Biosite, Otsuka Pharmaceuticals, Ortho Clinical Diagnostics, PDL Pharmaceuticals, Scios, Inc., and The Medicines Company. He has served as a consultant for Abbott, Beckman-Coulter, Inc., Biosite, Inovise Medical, Inc., Inverness Medical Innovations, Inc., Otsuka Pharmaceuticals, Ortho Clinical Diagnostics and The Medicines Company, Heartscape Technologies, Inc.; and he has received support in the form of research grants from Abbott, BAS, Biosite, Brahms, PCT, CHF Solutions, Heartscape Technologies, Inc., Inovise Medical, Inverness Medical Innovations, Inc., PDL Pharmaceuticals, and The Medicines Company. Dr Varon has received honoraria for lectures from PDL Pharmaceuticals, Eli Lilly and Company, and The Medicines Company, and has served as a consultant for EKR Pharmaceuticals and The Medicines Company.
References
- VaronJTreatment of acute severe hypertension: current and newer agentsDrugs200868328329718257607
- MarikPEVaronJHypertensive crises: challenges and managementChest200713161949196217565029
- ZampaglioneBPascaleCMarchisioMCavallo-PerinPHypertensive urgencies and emergencies. Prevalence and clinical presentationHypertension19962711441478591878
- KaplanJAFinlaysonDCWoodwardSVasodilator therapy after cardiac surgery: a review of the efficacy and toxicity of nitroglycerin and nitroprussideCan Anaesth Soc J19802732542596769567
- AmaranathLKellermeyerWFJrTachyphylaxis to sodium nitroprussideAnesthesiology19764443453481259195
- KhambattaHJStoneJGKhanEHypertension during anesthesia on discontinuation of sodium nitroprusside-induced hypotensionAnesthesiology1979512127130453612
- BenumofJLHypoxic pulmonary vasoconstriction and infusion of sodium nitroprussideAnesthesiology1979506481483453572
- VuylstekeAMilnerQEricssonHMurDDunningJJolin-MellgardAPharmacokinetics and pulmonary extraction of clevidipine, a new vasodilating ultrashort-acting dihydropyridine, during cardiopulmonary bypassBr J Anaesth200085568368911094580
- Kieler-JensenNJolin-MellgårdANordlanderMRickstenSECoronary and sustemic hemodynamic effects of clevidipine, an ultra-short-acting calcium antagonist, for treatment of hypertension after cardiac surgeryActa Anaesth Scand200044218619310695913
- BaileyJMLuWLevyJHRamsayJGShore-LessersonLPrielippRCClevidipine in adult cardiac surgical patients: a dose-finding studyAnesthesiology20029651086109411981147
- ChobanianAVBakrisGLBlackHRCushmanWCGreenLAIzzoJLJrSeventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood PressureHypertension20034261206125214656957
- FergusonRKVlassesPHHypertensive emergencies and urgenciesJAMA198625512160716133005672
- KaplanNMTreatment of hypertensive emergencies and urgenciesHeart Dis Stroke1992163733781344134
- Kincaid-SmithPMcMJMurphyEAThe clinical course and pathology of hypertension with papilloedema (malignant hypertension)Q J Med19582710511715313506014
- BennettNMSheaSHypertensive emergency: case criteria, sociodemographic profile, and previous care of 100 casesAm J Public Health19887866366403369591
- LipGYBeeversMPotterJFBeeversDGMalignant hypertension in the elderlyQJM19958896416477583078
- VaronJMarikPEClinical review: the management of hypertensive crisesCrit Care200375374378412974970
- LipGYBeeversMBeeversDGComplications and survival of 315 patients with malignant-phase hypertensionJ Hypertens19951389159248557970
- HaasARMarikPECurrent diagnosis and management of hypertensive emergencySemin Dial200619650251217150051
- PrisantLMCarrAAHawkinsDWTreating hypertensive emergencies. Controlled reduction of blood pressure and protection of target organsPostgrad Med199393292968433961
- BannanLTBeeversDGWrightNABC of blood pressure reductionBr Med J198028162459219237427510
- BertelOMarxBEConenDEffects of antihypertensive treatment on cerebral perfusionAm J Med1987823B29362882675
- ReedWGAndersonRJEffects of rapid blood pressure reduction on cerebral blood flowAm Heart J198611112262283946155
- StrandgaardSOlesenJSkinhojELassenNAAutoregulation of brain circulation in severe arterial hypertensionBr Med J1973158525075104692673
- VaronJMarikPEPerioperative hypertension managementVasc Health Risk Manag20084361562718827911
- ChobanianAVBakrisGLBlackHRCushmanWCGreenLAIzzoJLJrThe Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 reportJAMA200321;289192560257212748199
- PletsCArterial hypertension in neurosurgical emergenciesAm J Cardiol198963640C42C2562817
- HalpernNAAliceaMKrakoffLRGreensteinRPostoperative hypertension: a prospective, placebo-controlled, randomized, double-blind trial, with intravenous nicardipine hydrochlorideAngiology19904111 Pt 299210042248428
- Prys-RrobertsCAnaesthesia and hypertensionBr J Anaesth19845677117246145438
- GalTJCoopermanLHHypertension in the immediate postoperative periodBr J Anaesth19754717074238547
- AronsonSDykeCMStiererKALevyJHCheungATLumbPDThe ECLIPSE trials: comparative studies of clevidipine to nitroglycerin, sodium nitroprusside, and nicardipine for acute hypertension treatment in cardiac surgery patientsAnesth Analg200810741110112118806012
- PowroznykAVVuylstekeANaughtonCMissoSLHollowayJJolin-MellgardAComparison of clevidipine with sodium nitroprusside in the control of blood pressure after coronary artery surgeryEur J Anaesthesiol200320969770312974590
- LevyJHMancaoMYGitterRKereiakesDJGrigoreAMAronsonSClevidipine effectively and rapidly controls blood pressure pre-operatively in cardiac surgery patients: the results of the randomized, placebo-controlled efficacy study of clevidipine assessing its preoperative antihypertensive effect in cardiac surgery-1Anesth Analg2007105491892517898366
- Rodriguez GabrielaVJClevidipine: A unique agent fot the criticalCritical Care and Shock2006924
- EricssonHFaktCJolin-MellgardANordlanderMSohtellLSunzelMClinical and pharmacokinetic results with a new ultrashort-acting calcium antagonist, clevidipine, following gradually increasing intravenous doses to healthy volunteersBr J Clin Pharmacol199947553153810336577
- PollackCVVaronJGarrisonNAEbrahimiRDunbarLPeacockWFtClevidipine, an intravenous dihydropyridine calcium channel blocker, is safe and effective for the treatment of patients with acute severe hypertensionAnn Emerg Med200953332933818534716
- LevyJHHurauxCNordlanderMEpsteinMTreatment of perioperative hypertensionCalcium Antagonists in Clinical MedicinePhiladelphiaHanely and Belfus1997
- FriederichJAButterworthJFtSodium nitroprusside: twenty years and countingAnesth Analg19958111521627598246
- The Medicines Company ICleviprex™ (clevidipine butyrate) prescribing information [online] [updated 2008 August; cited 25 August 2008]. http://www.cleviprex.com/media/ClevidipinePI.pdfAccessed July 15, 2009
- NordlanderMSjoquistPOEricssonHRydenLPharmacodynamic, pharmacokinetic and clinical effects of clevidipine, an ultrashort-acting calcium antagonist for rapid blood pressure controlCardiovasc Drug Rev200422322725015492770
- Kieler-JensenNJolin-MellgardANordlanderMRickstenSECoronary and systemic hemodynamic effects of clevidipine, an ultra-short-acting calcium antagonist, for treatment of hypertension after coronary artery surgeryActa Anaesthesiol Scand200044218619310695913
- EricssonHBredbergUErikssonUJolin-MellgardANordlanderMRegardhCGPharmacokinetics and arteriovenous differences in clevidipine concentration following a short- and a long-term intravenous infusion in healthy volunteersAnesthesiology2000924993100110754618
- AronsonSDykeCStiererKLevyJCheungALumbPThe ECLIPSE Trials: Comparative studies of clevidipine to nitroglycerin, sodium nitroprusside, and nicardipine for acute hypertension treatment in cardiac surgery patientsAnesth Analg200810741110112118806012
- EagleKAGuytonRADavidoffREdwardsFHEwyGAGardnerTJACC/AHA 2004 guideline update for coronary artery bypass graft surgery: summary article: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1999 Guidelines for Coronary Artery Bypass Graft Surgery)Circulation200411091168117615339866
- MackMJBrownPPKugelmassADBattagliaSLTarkingtonLGSimonAWCurrent status and outcomes of coronary revascularization 1999 to 2002: 148, 396 surgical and percutaneous proceduresAnn Thorac Surg2004773761766 discussion 6–814992867
- LambertCRHillJANicholsWWFeldmanRLPepineCJCoronary and systemic hemodynamic effects of nicardipineAm J Cardiol19855566526563976506
- LeslieJBristerNLevyJHYaredJPMartyAMartinHTreatment of postoperative hypertension after coronary artery bypass surgery. Double-blind comparison of intravenous isradipine and sodium nitroprussideCirculation1994905 Pt 2II2562617955262
- SinglaNWarltierDCGandhiSDLumbPDSladenRNAronsonSTreatment of acute postoperative hypertension in cardiac surgery patients: an efficacy study of clevidipine assessing its postoperative antihypertensive effect in cardiac surgery-2 (ESCAPE-2), a randomized, double-blind, placebo-controlled trialAnesth Analg20081071596718635468
- GilmoreRMMillerSJSteadLGSevere hypertension in the emergency department patientEmerg Med Clin North Am20052341141115816199342
- PeacockWFVaronJEbrahimiRDunbarLPollackCVJrClevidipine for severe hypertension in patients with renal dysfunction: a VELOCITY trial analysisBlood Press2009In press