Abstract
The continued movement away from the treatment of individual cardiovascular (CV) risk factors to managing overall and lifetime CV risk is likely to have a significant impact on slowing the rate of increase in cardiovascular disease (CVD). However, the management of CVD is currently far from optimal even in parts of the world with well-developed and well-funded healthcare systems. Effective implementation of the knowledge, treatment guidelines, diagnostic tools, therapeutic interventions, and management programs that exist for CVD continues to evade us. A thorough understanding of the multifactorial nature of CVD is essential to its effective management. Improvements continue to be made to management guidelines, risk assessment tools, treatments, and care programs pertaining to CVD. Ultimately, however, preventing the epidemic of CVD will require a combination of both medical and public health approaches. In addition to improvements in the “high-risk” strategy, management, an increase in the utilization of population-based management strategies needs to be made to attempt to reduce the number of patients falling within the “at-risk” stratum for CVD. This review outlines how a comprehensive approach to CVD management might be achieved.
Introduction
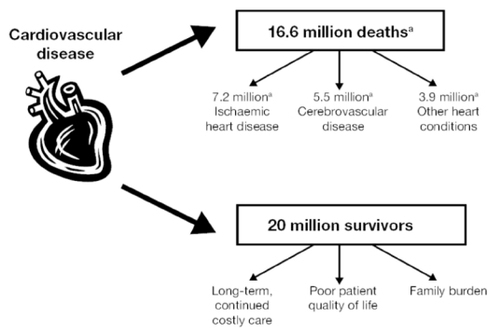
Cardiovascular disease (CVD) is one of the most prevalent and devastating health problems in the world and is responsible for approximately 30% of deaths worldwide (CitationWHO 2005) which equates to about 16.6 million deaths (). It is the leading cause of death in many developed countries and, by 2010, it is thought that CVD will be the leading cause of death in developing countries (CitationWHO 2005). Furthermore, the mortality, financial, and medical resource costs of CVD worldwide are huge and increasing.
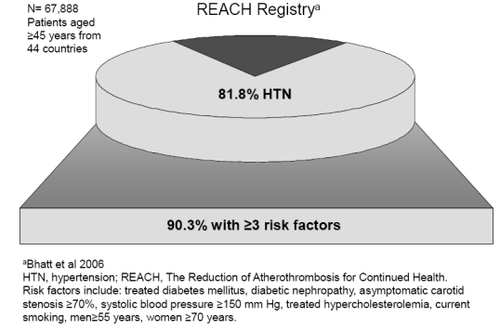
Figure 2 Most hypertensive patients have additional risk factors (CitationBhatt et al 2006).
Efforts are being extended to investigate ways to optimally manage risk factors for CVD and to improve medical interventions for the disease. In some countries these efforts have been rewarded with reductions in CVD mortality, as seen in most Northern, Southern, and Western European countries (CitationRayner 2000). An example of a successful community-based intervention strategy was started in the North Karelia province of Finland in 1972 (CitationPuska 1988; CitationVartiainen et al 1994; CitationPuska et al 1998). The interventions aimed to change target risk factors and health behaviors (serum cholesterol, blood pressure, smoking, diet) at the population level. In the early 1970s middle-aged Finnish men had the highest mortality from CVD in the world, but since this prevention program was started the mortality rate decreased dramatically; from 1969–1971 to 1995 the age-standardized coronary heart disease (CHD) mortality (per 100,000) decreased in North Karelia by 73% (CitationPuska et al 1998).
However, in many regions, reductions are not as impressive or conversely the prevalence of CVD is rising. Worldwide increases in CVD events are anticipated because the disease remains uncontrolled on a global scale. There is, therefore, a critical need to find ways to blunt the worldwide increase in CVD projected for forthcoming decades (CitationMurray and Lopez 1997).
What may be surprising is that we already possess the knowledge and the tools to significantly reduce the burden of CVD risk. However, effectively implementing the treatment guidelines, diagnostic tools, therapeutic interventions, and management programs that exist for CVD somehow still manages to evade us. Among the reasons for this include the increasing number of people adopting lifestyles that are at odds with maintaining an acceptable CVD risk (CitationWHO 2005; CitationChobanian et al 2003), elements of which may include poor diet, smoking, and physical inactivity. Furthermore, epidemics of conditions related to these unhealthy lifestyles (eg, diabetes and obesity) are escalating, which further increases the rise in CVD. For example, it has been estimated that there are more than 1 billion overweight adults and more than 300 million adults who are clinically obese (CitationAHA 2003). Obesity rates have dramatically increased (>3 fold) in parts of North America, Eastern Europe, the Middle East, the Pacific Islands, Australia, and China since 1980 (CitationAHA 2003).
The prevalence of diabetes (which is closely linked with obesity) is also increasing rapidly. For example, the worldwide prevalence of diabetes is expected to nearly double from 2.8% in 2000 to 4.4% in 2030, a rise from 171 million to 366 million people (CitationWild et al 2004). In the US, the prevalence of those diagnosed with diabetes has increased by 61% since 1990 (CitationRosamond et al 2007). It is estimated that 20.8 million Americans (7% of the population) now have diabetes (CitationRosamond et al 2007). Similarly, the prevalence of type 2 diabetes has now reached epidemic levels in Asia (CitationYoon et al 2006) with levels very similar to those in the US and Europe (approximately 7.8% in 2003). The highest rates in Europe are generally observed in countries of Central and Eastern Europe (International Diabetes Federation’s Diabetes Atlas). The ever increasing worldwide burden of diabetes will have a substantial impact on the occurrence of CVD. The recent INTERHEART study revealed that worldwide those with diabetes are 2.37 times more likely to experience a myocardial infarction (MI) in comparison with those without diabetes (CitationYusuf et al 2004). Moreover, previous studies have demonstrated that diabetes is associated with a CV risk similar to that post-MI (CitationHaffner et al 1998) and an equivalent risk to ageing 15 years (CitationBooth et al 2006) (). Of note is the fact that diabetes has a far greater adverse impact on women, although women develop CHD at a later age, usually lagging behind men by about 10 years (CitationLerner and Kannel 1986), women with diabetes are up to 50% more likely to die from CHD compared with men with diabetes (CitationNatarajan et al 2003; CitationHuxley et al 2006).
Table 1 Major risk factors and protective factors for CVD
The management of CVD is currently in a state of transformation. In the past, the management process has centered on the modification of single risk factors, such as hypertension. However, there have been repeated calls to move away from this siloed approach (CitationAnsell 2005; CitationGiles et al 2005; CitationJackson et al 2005; CitationMancia 2006) and many treatment guidelines now recommend simultaneously adopting lifestyle and therapeutic interventions targeted at multiple risk factors (CitationDe Backer et al 2003; CitationJoint British Societies 2005). This change of perception promises to have a positive impact on the success of treatment for the disease. This review aims to demonstrate how the consideration of the multifactorial nature of CVD needs to become the cornerstone of how CVD is viewed, assessed, and ultimately managed.
Key points
– CVD is responsible for approximately 30% of deaths worldwide.
– The multifactorial nature of CVD needs to underpin management strategies for the disease.
– To optimally manage CVD, therapeutic interventions need to target multiple risk factors.
Multifactorial nature of CVD
The numerous risk factors for CVD are usually categorized based on whether they are modifiable or are non-modifiable (). In addition, certain factors have been shown to be protective against the development of CVD, namely, daily consumption of fruit and vegetables, regular moderate alcohol consumption, and regular physical activity (CitationMcManus 2005). Evidence accumulated over the past 30 years has consistently demonstrated that these risk factors are linked epidemiologically, clinically, and metabolically (CitationNeaton and Wentworth 1992; CitationAsmar et al 2001; CitationThomas et al 2002; CitationFelmeden et al 2003; CitationGreenland et al 2003; CitationBhatt et al 2006).
One of the most revolutionary findings from epidemiological data is that hypertension usually occurs in conjunction with other major risk factors for CVD, namely, glucose intolerance, obesity, left ventricular hypertrophy, and dyslipidemia (CitationKannel 2000a, Citationb; CitationAsmar et al 2001; CitationGreenland et al 2003; CitationO’Meara et al 2004; CitationBhatt et al 2006).
This is thought to be because these factors are metabolically linked to hypertension, and could thus form a predisposition to development of the condition (CitationReaven et al 1996). Findings from various studies, including the Framingham Heart Study have shown that CVD risk factor “clustering” occurs frequently in individuals (CitationKannel 2000a, Citationb; CitationAsmar et al 2001; CitationGreenland et al 2003; CitationO’Meara et al 2004; CitationBhatt et al 2006). A cluster of 2 or more risk factors occurs in approximately half of hypertensive persons, a frequency twice that expected by chance (CitationKannel 2000a, Citationb). Clusters of 3 or more risk factors occur at 4 times the expected rate (CitationKannel 2000a, Citationb). In fact, only 10%–20% of cases of hypertension occur in the absence of other CVD risk factors (CitationKannel 2000a, Citationb; CitationBhatt et al 2006), for example, in the Reduction of Atherothrombosis for Continued Health (REACH) registry, 90.3% of patients with hypertension had ≥3 risk factors () (CitationBhatt et al 2006). Furthermore, obesity and weight gain appear to be among the most important determinants of the rate of development of hypertension and the tendency for other risk factors to cluster with elevated blood pressure (BP) (CitationKannel 2000a).
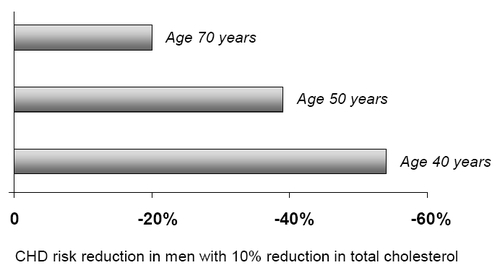
Although much emphasis is placed on modifiable risk factors, it is important to appreciate the impact of non-modifiable risk factors such as gender and age, which may influence the potency of modifiable risk factors. Increasing age plays an important role in the risk equation. With each additional year of life comes an increased risk of CVD complications, and the prevalence of other risk factors such as hypertension (CitationVasan et al 2002) and dyslipidemia (CitationPrimatesta and Poulter 2000) are seen to increase. A non-smoking male aged 35–44 with total cholesterol:high-density lipoprotein (HDL) ratio of 6, and a systolic BP of 150 mmHg, has a 15% risk of a coronary event over the next 10 years. At 45–64, bearing the same systolic BP and cholesterol levels (though in reality both may increase with age), his risk is between 15% and 30%. At 65 years, his risk is greater than 30%. Interestingly, the impact of the modifiable risk factors diminishes with age, for example, an analysis of 10 cohort studies found that lowering total cholesterol by 10% was associated with a 54% CHD risk reduction in men aged 40 years, but only a 20% reduction in men aged 70 years () (CitationLaw et al 1994). Taken together, these examples support the concept that risk factor management should be implemented early and aggressively to be most effective.
Figure 3 Influence of age on relationship between cholesterol and coronary heart disease (CHD) (CitationLaw et al 1994).
Epidemiological studies have demonstrated a continuum of risk for increasing levels of BP, total cholesterol (TC), low-density lipoprotein (LDL), and smoking (CitationWilson et al 1998). For BP beginning at 115/75 mmHg, the risk of CVD doubles with each increment of 20/10 mmHg (CitationChobanian et al 2003). Similarly, the risk of CHD and CVD increases in a similar manner with LDL cholesterol (LDL-C) concentration (CitationNeaton and Wentworth 1992; CitationStamler et al 1993; CitationThomas et al 2002). This has important implications for disease management. In an environment where some international guidelines still outline therapeutic cut-off points for BP and LDL-C, it is critical for physicians (and indeed patients) to understand that there is no threshold where CV risk ceases to exist. There is no level of risk that can be considered “safe”. In response to these findings, target levels for LDL-C and BP have moved progressively downwards. This trend is set to continue as a number of studies have provided evidence that intensive lipid-lowering therapy that reduces LDL-C beyond the levels currently recommended is associated with reduced progression of coronary atherosclerosis and greater protection against death or major CV events than more moderate therapy (CitationCannon et al 2004; CitationNissen et al 2004a).
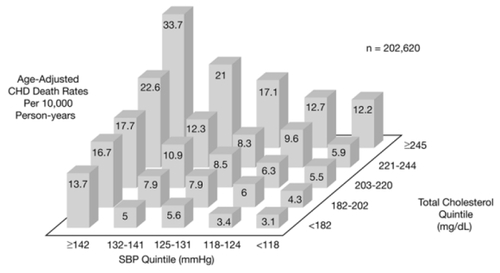
Another important finding is that the increased risk of CVD resulting from multiple risk factors is frequently greater than simply additive (CitationNeaton and Wentworth 1992; CitationThomas et al 2002). Using data from the Multiple Risk Factor Intervention Trial (MRFIT), Neaton and colleagues examined the interaction between TC levels, systolic BP, smoking, and CHD death rates (CitationNeaton and Wentworth 1992). illustrates the strong, graded relationship between increasing TC levels and CHD death across systolic BP levels, and the similarly strong relationship between increasing systolic BP and CHD death across TC levels. When risk factors were analyzed together, patients in both the highest TC and the highest systolic BP quintiles had an approximately 11-fold greater risk of CHD death than patients who were in both the lowest TC and lowest systolic BP quintiles (CitationNeaton and Wentworth 1992). Similarly, Liao et al studied a cohort of more than 15,800 Americans and found that the incidence rate of CVD events observed in patients with hypertension and elevated LDL-C was 51 per 10,000 person years (CitationLiao et al 2004). This was significantly larger than the sum of the incidence rates expected due to either condition alone (28 per 10,000 person years). The excess risk of 31% indicates synergism between these two risk factors. Pathophysiology studies have provided potential mechanisms by which hypertension and dyslipidemia might synergistically accelerate atherosclerosis, including increased endothelial permeability (CitationMeyer et al 1996), increased intimal retention of atherogenic lipoproteins (CitationRakugi et al 1996), exacerbation of inflammation (CitationBarter 2005; CitationBautista et al 2005), and increased free radical production (CitationRodriguez-Porcel et al 2003); all of which may contribute to endothelial dysfunction (CitationBonetti et al 2003).
Figure 4 The additive effect of cholesterol and systolic blood pressure on the risk of coronary heart disease death. Reproduced with permission from CitationNeaton JD, Wentworth D. 1992. Serum cholesterol, blood pressure, cigarette smoking, and death from coronary heart disease. Overall findings and differences by age for 316,099 white men. Multiple Risk Factor Intervention Trial Research Group. Arch Intern Med, 152:56–64. Copyright © 1992. American Medical Association. All rights reserved.
The significance of the relationships between CV risk factors and CVD events have been elegantly demonstrated in the results of recent clinical trials and meta-analyses which have assessed the effects of intensive interventions aimed at reducing modifiable risk factors for CVD (CitationGaede et al 2003; CitationJulius et al 2004; CitationBaigent et al 2005). Based on a meta-analysis of clinical trials enrolling 90,056 patients Baigent et al concluded that, regardless of baseline LDL-C levels, the 5-year risk of major coronary events, coronary revascularization, and stroke was lowered by approximately 20% per 1 mmol/L (38.8 mg/dL) reduction in LDL-C (CitationBaigent et al 2005). Similarly, Turnbull et al demonstrated in a meta-analysis of randomized trials of antihypertensives that the relative risks of stroke and major CV events were significantly reduced (by 28% and 22%, respectively) when systolic BP was lowered by an average of 5 mmHg using angiotensin-converting enzyme (ACE) inhibitor-based regimens versus placebo (CitationTurnbull 2003). The Steno-2 study demonstrated that in patients with type 2 diabetes and microalbuminuria, intensive interventions targeted at hyperglycemia, hypertension, dyslipidemia, and microalbuminuria, together with the secondary prevention of CVD using aspirin, could reduce the risk of CVD by 50% versus conventional treatment (CitationGaede et al 2003).
The way in which the multiple risk factors for CVD cluster dictates that the disease should be approached in a way that takes all of these risk factors into account when evaluating risk and when choosing the most appropriate treatment. Addressing only a single risk factor will reduce an individual’s CVD risk but leave a substantial residual risk; such a strategy equates to “missing” those patients who are at long-term risk of disease and leads to chronic sub-optimal management of the disease. In contrast, a population-wide intervention to reduce both systolic BP and TC could reduce CVD events by 45% (CitationEmberson et al 2004).
Key points
– Risk factors for CVD frequently cluster in individuals and can act in a synergistic manner to increase the risk of CV events.
– Age is an important unmodifiable risk factor for CVD. With increasing age, the 10-year risk of CVD increases steeply.
– There is a continuum of risk for CVD with increasing levels of BP, TC, LDL-C, and smoking; and this risk is greater still in individuals with diabetes. There is no lower threshold level at which CVD risk ceases to exist.
Current approach to managing these factors
There are numerous guidelines for the treatment and management of individual risk factors such as hypertension (CitationChobanian et al 2003; CitationMancia et al 2007) and dyslipidemia (CitationNational Cholesterol Education Program 2001), as well as joint guidelines for the prevention of atherosclerosis and CVD (CitationDe Backer et al 2003; CitationJoint British Societies 2005). The mutual underlying principles of these guidelines include the following:
– CV risk assessment.
– Treatment of those at high risk for disease.
– Management adjusted to patient’s total risk of CHD or CVD; the higher the risk, the greater the intensity of management.
– Employment of a range of interventions to address risk factors for CVD, including treatment of hypertension, treatment of dyslipidemia, smoking cessation, increased physical activity, cardioprotective diet, treatment of hyperglycemia, weight management, antiplatelet/anticoagulant therapy, and psychosocial support.
Considering the body of scientific evidence that supports these guidelines, the management of CVD should include all of these elements, as a minimum. However, the success (in terms of lowering CV risk) in disseminating relevant new clinical data and implementing treatment guidelines has in general been disappointing (CitationErhardt et al 2004). Surveys and observational studies continue to demonstrate that the management/control of CV risk factors is poor – even in developed countries where more resources exist for implementing guidelines (CitationEUROASPIRE I and II Group 2001; CitationJohnson et al 2006; CitationWong et al 2006). The REACT survey, conducted with physicians from 5 European countries, showed that while 81% of practitioners agreed with therapeutic guidelines and reported using them, only 18% felt that the guidelines were being implemented to any great extent (CitationHobbs and Erhardt 2002). There are various issues that prevent guidelines from being implemented effectively and thus inhibit the successful reduction of CV risk (). A discussion paper regarding implementation of guidelines for CVD is provided by Erhardt et al (CitationErhardt et al 2004).
Table 2 Factors that influence the implementation of CVD guidelines
In recent years, the most relevant development in CVD guidelines has been the acknowledgement of the multifactorial nature of CVD. Too often, the treatment focus will be on a single risk factor that might lower the risk by up to 20%–30%, however, it must be remembered that the residual risk in this individual is still 70%–80%; more can be done. This has resulted in a positive shift from management based solely on single risk factors, towards managing a patient’s total CV risk, as demonstrated by the incorporation of tools for calculating CV risk into recent treatment guidelines (CitationNational Cholesterol Education Program 2001; CitationDe Backer et al 2003; CitationJoint British Societies 2005). However, the understanding of the importance of this approach has still not had far-reaching impact and has not been implemented in a uniform manner, as highlighted by the management conundrums outlined below, some of which have their foundations entrenched in the fact that CVD is a multifactorial disease.
Management conundrums
As management guidelines evolve, based on emerging clinical data, they will invariably include elements of scientific evidence, practicality, consensus, and compromise. There will always be the inevitable challenge of bridging the gap between theory and practice. Today, there are a number of conundrums regarding the management of CVD which continue to be debated and have yet to be effectively addressed within current guidelines.
Population versus high-risk approach?
Two approaches to primary prevention are generally recognized: the high-risk approach which involves the identification and treatment of only those individuals at high risk; and the population approach which involves population-wide changes in risk factors so that the entire population distribution of those with CVD is shifted, meaning that less individuals fall within the “at risk” level (). The high-risk approach is the most obvious choice for those concerned about the CV risk of the individual patient, limiting treatment to only those most likely to have a CV event in the short term. However, this is complicated by the fact that on a population basis, most CV events do not occur in the small number of high-risk individuals but rather in the much larger proportion of patients in the low-to-moderate risk stratum. For example, MacMahon and Rodgers found that 75% of strokes occur among those with “normal” BP levels (CitationMacMahon and Rodgers 1994).
Figure 5 Pictorial representation of the distribution of risk for cardiovascular disease, and high-risk and population-based management strategies.
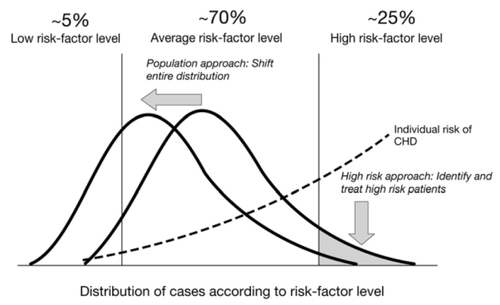
Consequently, if the primary focus of management is on treating the minority of individuals at high risk, while the individual patient may benefit, the impact on national mortality and morbidity figures will remain almost unchanged because intervention is only provided to a small number of individuals. To achieve a considerable impact on CVD requires an approach that serves the individual with overt disease as well as those with risk factors that predispose them to disease in later life. Long-term pharmaceutical drug use can only be justified in a limited number of people. Therefore, a strategy that reduces the level of risk in the entire population is required. Hence a combination of high-risk and population approaches is needed. A number of advantages and disadvantages of these two approaches are outlined in .
Table 3 Advantages and disadvantages of high-risk and population approaches to CVD management
Who should be considered as high risk?
We have already determined that because of the continuum of risk, there is no level of CVD risk which can be considered as “safe”. In addition, advancing age confers an increasing risk for CVD to the patient, so the individual’s 10-year risk is continually changing. Guidelines differ with respect to the definition of high risk, depending on health system and health policy environments. Many currently used guidelines define patients at high risk as those with a 30% absolute risk of developing a CV event within the next 10 years. More recent guidelines have changed the definition of high risk to encompass patients with ≥20% risk of CV events (CitationJoint British Societies 2005). The reason why these levels are chosen is based on a number of factors including scientific, financial, practical, as well as political issues. However, as we have also shown, the number of patients that fall within this 20%–30% of risk is small. Adoption of 20%–30% 10-year risk as an indication for therapy denies a huge proportion of individuals the opportunity to prevent or delay a first vascular event, and subjects the individual to years of potential atherogenic damage.
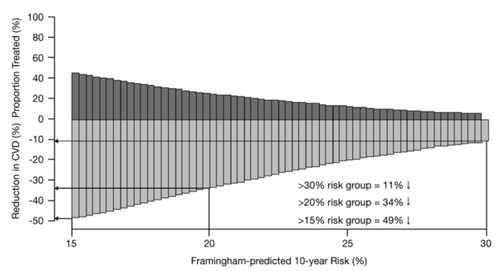
Emberson et al elegantly demonstrated that with high-risk strategies, the higher the level at which high risk is defined, the less effective the reduction in CVD levels is () (CitationEmberson et al 2004). Furthermore, they found that aggressive treatment in individuals with a 10-year Framingham risk of ≥30% would theoretically reduce the occurrence of major CVD by approximately 11%, this increased to 34% when a ≥20% high-risk threshold was employed. However, when modest (10%) downshifts to the population distribution of serum TC and systolic BP were applied, a reduction in major CVD by 45% was observed (CitationEmberson et al 2004).
Figure 6 The impact of different levels of Framingham-predicted 10-year risk of cardiovascular disease (CVD) on the percentage reduction of CVD and the proportion of patients treated. Reproduced with permission from Emberson J, Whincup P, Morris RW, et al 2004. Evaluating the impact of population and high-risk strategies for the primary prevention of cardiovascular disease. Eur Heart J, 25:484–91. Copyright © Oxford University Press.
This leads to the question of whether the definition of “high risk” used as an indicator for therapeutic intervention in guidelines is set too high. The answer is probably “yes”. Considering that CV risk factors may start to cluster early in life (CitationBao et al 1994), it is essential that the risk factor burden of people in their second and third decades is reduced. Essentially, a shift is needed in the perception of those who are at risk. Many guidelines still focus on absolute 5-, 7-, or 10-year projections of CHD or CVD risk (CitationNational Cholesterol Education Program 2001; CitationDe Backer et al 2003; CitationJoint British Societies 2005). This may be an inadequate approach in younger or middle-aged patients. For example, a 50-year-old man with high cholesterol and hypertension has a 10-year risk of heart attack or coronary death of only 7%, but a lifetime risk that is 10-times greater (CitationLloyd-Jones et al 2006).
Ideally, what is needed is a longer – preferably lifetime – risk assessment in order that interventions can be applied in time to prevent underlying vascular events. However, the level finally chosen to delineate high risk will ultimately be a decision based on cost, ie, what level of risk can affordably be managed on a large scale. Hence, while scientific knowledge will continue to promote reducing the level that constitutes high risk, lack of funding and political arguments will continue to promote maintaining the level at that which is affordable.
Relative or absolute risk?
Knowledge of the multifactorial nature of CVD has prompted the development of management systems based on “absolute risk” of developing CVD. Absolute risk – the actual odds that a patient (or population) will develop an event over a given period of time – reflects the sum of all the factors that contribute to the risk of CVD. Absolute risk always increases with advancing age, irrespective of the level of BP, cholesterol, or of smoking habits. This measurement is useful in that it allows identification of individuals who need to be advised immediately about risk factor reduction. However “relative risk” measurements can also be a useful tool for clinicians, particularly in younger patients with a low absolute risk, because they can provide information regarding who is at a high relative risk compared with their peers and who may benefit from aggressive risk factor reduction in the long term. The recently updated ESH-ESC guidelines recommend that treatment of younger patients should be based on their relative risk rather than their absolute risk (CitationMancia et al 2007). These updated preventive guidelines also contain relative risk scores for younger individuals to facilitate the understanding of risk in these individuals who have a low absolute 10-year risk of CVD events.
Conversely, when formulating public health policy absolute risk reductions should be used as these provide a far more meaningful measure of what can be achieved at the population level. For example, reducing the daily salt intake from 9.5 g to 6 g will lead to a 13% reduction in stroke and a 10% reduction in heart disease (CitationMedical Research Council 2006).
Cardiovascular risk calculators are available that measure either absolute or relative risk, so it will be interesting to observe whether the useful information that can be derived from both of these measurements will be used to its fullest in the future.
Key points
– CVD guidelines have evolved to take account of the multifactorial nature of CVD, resulting in management strategies centered on lowering a patient’s total CV risk.
– Implementation of CVD guidelines is poor.
– To achieve a considerable impact on CVD requires a management approach that serves the individual with risk factors that predispose them to disease in later life as well as those with overt disease.
Recommended optimal approach
Based on the issues discussed above, the following represents our attempt at outlining what the optimal approach to CVD management might involve. While we accept that practicalities may always lie in the way of achieving what is essentially an idealistic approach, an appreciation of appropriate goals is an important step in improving management practices.
Step 1: Identifying patients at risk/estimating level of total lifetime risk
Recognizing patients who are at risk of a CV event is the first step to achieving effective prevention. Patients with existing CVD are usually at high risk for recurrent CVD events, but healthy patients with multiple CV risk factors may be as likely to suffer a CVD event as those with clinically manifest disease. It is a particularly important step for those with existing CV risk factors, as other CV risk factors likely coexist. When one CV risk factor has been identified, especially hypertension, regular screening for other CV risk factors is desirable.
Indeed, it can be argued that the concepts of primary and secondary prevention are now obsolete (CitationPlummer 2006). Firstly, as mentioned above, apparently healthy individuals with no previous CV events, may have asymptomatic indications of CVD, such as carotid artery stenosis and left ventricular hypertrophy, and thus may be at higher risk than those who have had CV events. Secondly, a patient may be unaware that they have had a CV event and thus if treatment recommendations are based on the occurrence of a CV event rather than their risk of a future event such patients would be managed inappropriately. For example, approximately 20% of MIs were unrecognized in the Atherosclerosis Risk in Communities (ARIC) study (CitationBoland et al 2002).
Considering the many variables that need to be considered in calculating an individual’s risk for CVD, it is essential that a properly validated risk assessment tool be used to help the physician derive an accurate picture of the individual’s risk. Effective risk assessment tools estimating absolute CV risk are available and should be used to identify people at high risk for CVD. They should be considered an aid to making clinical decisions about how intensively to intervene on lifestyle and how to proceed with the use of antihypertensive, lipid-lowering, and other modifiable risk factor medications. There are many variables that confer risk which are not included in the common risk algorithms – dietary and exercise habits, and psychosocial factors – and therefore any risk assessment must be individualized and include these factors. Furthermore, a positive family history and diabetes mellitus, not included in most risk algorithms, increases the risk of CVD significantly. Consequently, risk assessment tools are never exact and should be used in combination with clinical judgment.
In recent years web-based systems, score card methods, and tools such as the “Grimm Meter” have become available and have simplified the risk assessment procedure (CitationThomsen et al 2001; CitationConroy et al 2003; CitationGohlke et al 2005; CitationGrimm and Svendsen 2006). Many risk assessment tools are available that are of benefit in particular patient populations. A detailed review of these methods is outside the scope of this review (see CitationGrover et al 2006 for a recent review).
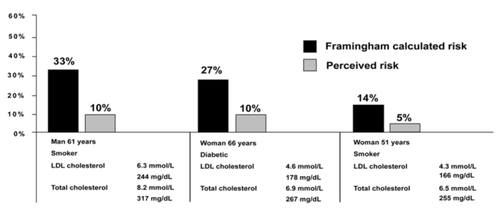
The decision over which risk assessment tool to employ is somewhat less important than the choice to actually use a risk assessment tool. As most tools generally arrive at a similar estimation of risk, the actual tool chosen is probably not critical. However, it is essential that some form of risk assessment is used as this leads to improved estimation of patient risk and hence better management. A study by Backlund et al demonstrated that physicians often underestimate their patients CV risk () (CitationBacklund et al 2004), and other studies show that physicians rarely or never use tools when calculating a patient’s CVD risk (CitationHobbs and Erhardt 2002; CitationDe Muylder et al 2004). Hobbs and Erhardt showed that 43% of physicians reported that they never use risk calculator charts that may accompany guidelines, a further 43% said they sometimes referred to them, but only 13% said that this was always the case (CitationHobbs and Erhardt 2002).
Figure 7 Physicians underestimation of their patients’ cardiovascular risk (CitationBacklund et al 2004)
There are some important caveats to using risk assessment tools. First, it is important for clinicians to appreciate that such tools provide only an estimate of risk. Biologic variability might mean that someone with a very low risk score could experience a CV event and someone with a very high chance of experiencing an event may not. Second, the outcome of the risk scoring exercise may not be the only reason why a physician may choose to offer an intervention; clinical judgment and thorough individual assessment (including exercise habits, food habits, and psychosocial factors) also need to play a role. Third, risk evaluation alone does not provide adequate information to help the patient understand their own risk and begin to make steps towards improving their own modifiable risk factor status. There are many physician- and patient-related barriers to communications regarding risk, an understanding of which is important for fully utilizing information arising from risk evaluation measures. Fourth, without improving therapeutic intervention, risk scoring is of little use. As Zimmerman and Horton-La Forge noted in 1996, “little evidence exists to suggest that risk assessment alone, without more intensive intervention, can have a lasting impact on health behaviors or health risks” (CitationZimmerman and Horton-La Forge 1996).
Step 2: Helping the patient to understand their personal risk
Providing patients with their CVD risk score is a useful means of motivating patients towards healthy behaviors (CitationSullivan et al 2004; CitationAlm-Roijer et al 2006). An understanding of both the fatal consequences and also the potential debilitating effects of nonfatal CV events, such as MI or stroke, may encourage patients to adhere to CV medications and life-style changes. However, this may be a little simplistic because uninformed patients may have difficulty in understanding the concepts of risk (CitationKnapp et al 2004). Knapp et al found that the use of verbal descriptors to improve the level of information about side-effect risk leads to overestimation of the level of harm and may lead patients to make inappropriate decisions about whether or not they take the medicine (CitationKnapp et al 2004). It is difficult, then, for the physician to decide what information to provide about CV risk. As a guide, physicians might wish to consider the following areas for communication with their patients:
Probability
Focus on the relative risk faced by that particular patient. Patients with CHD benefit from having specific individualized knowledge about their condition and their own risk factor status for promoting adherence to lifestyle changes and medical treatment (CitationAlm-Roijer et al 2006);
Exposure
Communicate that everyone faces the risk of CVD;
Hazard
Emphasize the modifiable risk factors the patient can control;
Consequences
Create a mental picture of CVD events, without creating fear, because this can influence whether a patient takes prescribed medications (CitationKnapp et al 2004). Within this concept, it is important to reiterate the need for adherence to both lifestyle changes and medications. Previous studies have clearly demonstrated that the percentage of patients who are adherent to both antihypertensive and lipid-lowering therapies declines sharply within the first year of therapy initiation (CitationChapman et al 2005). Furthermore, a link between low adherence to CV medications and poor clinical outcome has been demonstrated in a variety of settings (CitationWei et al 2002; CitationHo et al 2006a, Citationb).
Considering the challenges associated with establishing and maintaining effective communication with the CVD patient, and the consequences faced when this is not effectively achieved, it is likely that utilizing other healthcare professionals in the provision of in-depth counseling could be an advantage. With this in mind, the Risk Evaluation and Communication Health Outcomes and Utilization Trial (REACH OUT) has recently been completed. The study will assess the ability of a physician-delivered CHD risk evaluation and communication program to lower a patient’s predicted 10-year risk of MI or death due to CHD by 10% within 6 months, compared with usual care. Results from this trial are anticipated towards the later part of 2007. The results of this study promise to be of great interest to all of those involved in managing patients with CVD.
Step 3: Developing a comprehensive management strategy for the individual patient
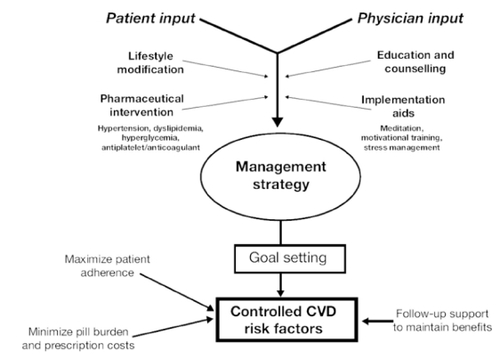
An effective management strategy for CVD should contain some element of lifestyle modification as well as pharmaceutical intervention, where appropriate (). As a first step in the management of their overall CVD risk, patients should be encouraged to adhere to healthy lifestyle habits. Patients should be informed of the benefits of smoking cessation, exercise, diet modification, and weight loss. A recent study supports this concept and has indicated that as many as 62% of CV events in men are preventable through adopting a low-risk lifestyle (CitationChiuve et al 2006). Compared with men who did not make lifestyle changes during follow-up in this study, those who adopted ≥2 additional low-risk lifestyle factors had a 27% lower risk of CHD (CitationChiuve et al 2006).
Where lifestyle changes are insufficient, therapy is advised. This should include a range of interventions such as treatment of hypertension, dyslipidemia, hyperglycemia, and antiplatelet/anticoagulant therapy.
It is important that the physician and patient closely collaborate to develop a management strategy that will suit the individual patient. One study showed that a multidimensional integrative approach, which identified specific health behaviors important for each patient to modify, was able to significantly reduce the risk of CVD. The patient, together with a health coach and a medical provider, devised a personal health plan which was driven not only by CV risk reduction but also the interests of the patient. Techniques used to help implement the health plan included meditation, relaxation training, stress management, motivational techniques, and health education and coaching (CitationEdelman et al 2006). It has been suggested that by working together, a goal-setting effort between patient and physician/medical team – if employed and adhered to – can help reduce CV risk (CitationMacGregor et al 2006).
Given the multifactorial nature of CVD it is not surprising that clinical trials have consistently demonstrated that multiple CV risk factors should be managed simultaneously to maximize reductions in CV events (CitationSamuelsson et al 1987; CitationSever et al 2003). The downside to this approach is that increasing pill burden and prescription costs can decrease adherence to treatment (CitationChapman et al 2005; CitationSafran et al 2005; CitationLynch 2006; CitationSoumerai et al 2006). Consequently, the development of multi-modal drugs, which in a single pill can target a number of risk factors, is a promising approach. In 2003, Wald and Law introduced the concept of combining medicines for effective risk factor reduction by use of the Polypill™. They proposed that a single, daily pill containing half doses (to minimize toxicity) of a beta-blocker, a thiazide diuretic, an ACE inhibitor, a statin, folic acid, and aspirin, taken by everyone aged >55 could reduce the incidence of CVD by more than 80% (CitationWald and Law 2003).
Step 4: Providing continued follow-up support
The aims of patient follow-up support should be to assess and communicate to the patient the success of intervention strategies in order to i) maintain patient motivation, ii) identify problems in adherence to the disease management strategy (there is a very real difference between obtaining a prescription for a medication and actually taking it), iii) provide further disease/therapy information.
Follow-up studies have observed that educational programs and counseling on CV risk and events have a significant effect for up to 12 months (CitationBarth et al 2006) and demonstrate the need for continued counseling and follow-up support. However, more information needs to be made available to the physician/medical team to help them provide such follow-up support effectively. Support should also be provided to those who have had a debilitating CV event such as an MI or stroke, who frequently live for many years after such an event.
Key points
– Recognizing patients who are at risk of a CV event is the first step to achieving effective CVD prevention.
– The concepts of primary and secondary prevention are in many ways now obsolete and should be substituted by proper risk calculation and risk stratification.
– Properly validated risk assessment tools should be used to help derive an accurate picture of the patient’s total CV risk, but should be used in conjunction with clinical judgment.
– Advising patients of their CVD risk is a useful means of motivating patients towards healthy behaviors, but needs to be done sensitively because the concept of risk can be misunderstood.
– Management for CVD should entail a close collaboration between the physician, other healthcare professionals, and the patient to develop a strategy that will suit the individual patient. It should include elements of lifestyle modification as well as pharmaceutical intervention, where appropriate, to address the multiple CV risk factors likely to be present. Follow-up support should be provided to ensure patient adherence and provide additional support where necessary.
Providing optimal care in a resource-scarce environment
Although the recommended optimal approach discussed above would bring about a substantial reduction in the prevalence of CVD, we need to be realistic considering the strong financial constraints under which many healthcare systems are operating. Indeed, 80% of the total global burden of CVD is carried by countries of low/moderate income (CitationWHO 2005). Disease prevention with statins and antihypertensive therapy has been shown to be cost-effective as the morbidity and mortality reductions and increases in life expectancy can be considerable (CitationMcMurray 1999; CitationPilote et al 2005). Nonetheless, further research is needed to acquire knowledge of the long-term cost consequences of various treatments and interventions. Cost-effective interventions to reduce the burden of CVD can only be implemented if health services policy environments and financial resources allow. For many (if not most) countries, the individual management of large numbers of patients, outside the high-risk sphere for CVD, will simply not be affordable. So what can be done to maximize any management efforts that are made in such countries?
Other healthcare providers
Implementation of a medical team approach in dealing with the patient’s needs is likely to be a more effective strategy than heavy reliance on the physician. Nurse-led care-share programs have been shown to be successful in providing the additional support and health promotion needed for effective management of CVD. Also, nurse evaluation of CV risk and medication adherence prior to and/or following the physician visit may help reinforce messages surrounding the importance of the illness and the need to adhere to prescribed therapies and lifestyle changes; and often patients find it easier to discuss such issues with a nurse. One UK study compared intensive management by nurses with routine follow-up in general practice for patients with CHD. Patients who received intensive nurse-led care reported improvements in their health, functional status, and in the likelihood of hospitalization within the first year of care (CitationCampbell et al 1998). In the USA, nurse case managers help in the care of patients in the out-patient setting. Their role includes securing long-term patient adherence and follow-up; developing clinic policy and computerized patient databases, and implementing management according to established CHD guidelines (CitationThomas et al 1997).
Care programs such as those described above are likely to be critical in improving care within any environment, but particularly those with limited resources. The most effective way of optimizing the outlay spent on managing CVD is to ensure that treatment applied is appropriate, that the patient adheres to the treatment and that, ultimately, risk factors for the disease are controlled.
Key points
– Providing optimal care for CVD is challenging considering the strong financial constraints under which many healthcare systems are operating.
– The most effective way of optimizing the outlay spent on managing CVD is to ensure that the treatment applied is appropriate, that the patient adheres to the prescribed treatment and that, ultimately, risk factors for CVD are controlled.
– The implementation of an effective nurse-patient interaction may improve the CV management.
What can we hope for in the future?
Guidelines relevant to CVD continue to evolve and improve. Significant advances were made in recent Canadian guidelines, on a number of levels, ie, by including global estimates of patient’s risk, by providing guidance on improving patient treatment adherence, and by improving the way in which the guidelines are disseminated and implemented (CitationDrouin et al 2006; CitationKhan et al 2006). The Canadian Hypertension Education Program (CHEP) recognizes that annually-updated, evidence-based guidelines for hypertension alone are not sufficient to improve the management of hypertension in Canada and have thus included an Implementation Task Force whose role it is to enhance dissemination and implementation of hypertension guidelines. Considering the impact that CHEP may have had on improvements in the management of hypertension in Canada, it is possible that it may serve as a model for disease management recommendations (CitationDrouin et al 2006).
The recently updated ESH-ESC guidelines (CitationMancia et al 2007) will also help to reinforce key messages; the guidelines emphasize the importance of assessing total CV risk, implementation of life-style changes, and blood pressure reduction per se rather than the antihypertensive class selected. In addition, the new guidelines recommend that combination therapy should be considered from the start (the choice of drug should be based on patient comorbidities), the threshold for initiating treatment should be more flexible (>140/90 mm Hg), and that all high-risk hypertensive patients (those with diabetes, multiple risk factors, or organ damage) should aim for a BP goal of <130/80 mm Hg. Moreover, it is noted that absolute risk should be used to guide treatment in the elderly whereas relative risk should be used in younger patients.
In future years, we might also expect to see improvements in risk assessment models and algorithms which measure global lifetime risk for CVD and improve existing models by adding novel risk factors. However, while the search for novel risk factors continues, any discoveries in this area are likely to be less important than the more thorough implementation of existing risk tools that are based on established risk factors. This is because 80% of CVD risk is conveyed by the 3 major risk factors: smoking, elevated BP, and high serum TC (CitationEmberson et al 2003). With optimal control of these risk factors, significant reduction in CV events may be obtained.
As explained earlier, the concept of a compound that can target multiple risk factors is likely to be an important tool for CVD management. While considerable challenges are likely to be faced in developing a therapy with the optimistic number of components proposed by CitationWald and Law (2003), inroads are being made with the development of combination therapies for CVD (CitationBlank et al 2005).
Ultimately, preventing an epidemic of CVD will likely require a combination of both medical and public health approaches. Public health strategies that target whole populations may offer a great prospect for reducing CVD.
Key points
– In future years, we might expect guidelines for CVD to evolve further by including elements to further help the patient adhere to prescribed treatment regimens and by including estimates of a patient’s global CV risk. Improving the dissemination and implementation of guidelines is likely to be vital in improving the control of CV risk factors.
– Compounds that target multiple risk factors for CVD may improve patient adherence.
– Ultimately, preventing an epidemic of CVD will likely require a combination of both medical and public health approaches.
Conclusion
The management of CVD is currently far from optimal, even in parts of the world with well-developed and well-funded healthcare systems. This is particularly concerning when considering the huge increase in CVD in low-middle income countries where healthcare systems are not funded to manage the growing CV epidemic.
The continued movement away from the treatment of individual CV risk factors to managing overall and lifetime CV risk is likely to have a significant impact on blunting the projected increase in CVD. However, for this to become effective, the importance of this approach needs to be appreciated on an even greater scale and ingrained into every aspect of CVD management.
A broad range of extremely effective lifestyle, counseling, and therapeutic interventions can be used in conjunction with CV risk assessment tools to markedly reduce an individual’s risk of CVD. Ultimately, however, quelling the CVD epidemic is likely to require a combination of effectively managing those at high risk of disease, and optimizing widespread population interventions which aim to reduce the number of individuals at risk. Considering the huge consequences of falling short in these aims, the success (or otherwise) in implementing these elements will be scrutinized.
Acknowledgements
Editorial assistance was provided by Jon Edwards of Envision Pharma and funded by Pfizer Inc.
References
- Alm-RoijerCFridlundBStagmoMKnowing your risk factors for coronary heart disease improves adherence to advice on lifestyle changes and medicationJ Cardiovasc Nursing200621E24E31
- [AHA] American Heart AssociationInternational cardiovascular disease statistics2003Dallas, TexasAmerican Heart Association
- AnsellBJEvidence for a combined approach to the management of hypertension and dyslipidemiaAm J Hypertens20051812495716245413
- AsmarRVolSPannierBHigh blood pressure and associated cardiovascular risk factors in FranceJ Hypertens20011917273211593091
- AvornJMonetteJLacourAPersistence of use of lipid-lowering medications:a cross-national studyJAMA19982791458629600480
- BacklundLBringJStrenderJ-EHow accurately do general practitioners and students estimate coronary risk in hypercholesterolaemic patientsPrimary Health Care Research and Development2004514552
- BaigentCKeechAKearneyPMEfficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statinsLancet200536612677816214597
- BaoWSrinivasanSRWattigneyWAPersistence of multiple cardiovascular risk clustering related to syndrome X from childhood to young adulthood. The Bogalusa Heart StudyArch Intern Med1994154184278053753
- BarterPThe inflammation: lipoprotein cycleAtheroscler Suppl20056152015823492
- BarthJCritchleyJBengelJEfficacy of psychosocial interventions for smoking cessation in patients with coronary heart disease:a systematic review and meta-analysisAnn Behav Med200632102016827625
- BautistaLEVeraLMArenasIAIndependent association between inflammatory markers (C-reactive protein, interleukin-6, and TNF-alpha) and essential hypertensionJ Hum Hypertens2005191495415361891
- BhattDLStegPGOhmanEMInternational prevalence, recognition, and treatment of cardiovascular risk factors in outpatients with atherothrombosisJAMA2006295180916403930
- BlankRLaSalleJReevesRSingle-pill therapy in the treatment of concomitant hypertension and dyslipidemia (The Amlodipine/Atorvastatin Gemini Study)J Clin Hypertens2005726473
- BolandLLFolsomARSorliePDOccurrence of unrecognized myocardial infarction in subjects aged 45 to 65 years (the ARIC study)Am J Cardiol2002909273112398956
- BonettiPOLermanLOLermanAEndothelial dysfunction: a marker of atherosclerotic riskArterioscler Thromb Vasc Biol2003231687512588755
- BoothGLKapralMKFungKRelation between age and cardiovascular disease in men and women with diabetes compared with non-diabetic people: a population-based retrospective cohort studyLancet2006368293616815377
- CabanaMDRandCSPoweNRWhy don’t physicians follow clinical practice guidelines? A framework for improvementJAMA199928214586510535437
- CampbellNCThainJDeansHGSecondary prevention clinics for coronary heart disease: randomized trial of effect on healthBMJ1998316143479572758
- CannonCPBraunwaldMDMcCabeCHIntensive and moderate lipid lowering with statins after acute coronary symptomsN Engl J Med2004350149550415007110
- ChapmanRHBennerJSPetrillaAAPredictors of adherence with antihypertensive and lipid-lowering therapyArch Intern Med200516511475215911728
- ChiuveSEMcCulloughMLSacksFMHealthy lifestyle factors in the primary prevention of coronary heart disease among menCirculation2006114160716818808
- ChobanianAVBakrisGLBlackHRThe seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: The JNC 7 ReportJAMA200328925607212748199
- ConroyRMPyoralaKFitzgeraldAPEstimation of ten-year risk of fatal cardiovascular disease in Europe: the SCORE projectEur Heart J200324987100312788299
- De BackerGAmbrosioniEBorch-JohnsenKEuropean guidelines on cardiovascular disease prevention in clinical practice. Third Joint Task Force of European and Other Societies on Cardiovascular Disease Prevention in Clinical PracticeEur Heart J20032416011012964575
- De MuylderRLorantVPaulusDObstacles to cardiovascular prevention in general practiceActa Cardiol2004591192515139651
- DrouinDCampbellNRKaczorowskiJImplementation of recommendations on hypertension: the Canadian Hypertension Education ProgramCan J Cardiol200622595816755314
- EdelmanDOddoneEZLiebowitzRSA multidimensional integrative medicine intervention to improve cardiovascular riskJ Gen Intern Med2006217283416808774
- EgedeLEImplementing behavioral counseling interventions in primary care to modify cardiovascular risk in adults with diabetesCardiovasc Rev Rep20032430612
- EmbersonJRWhincupPHMorrisRWReassessing the contribution of serum total cholesterol, blood pressure and cigarette smoking to the aetiology of coronary heart disease: impact of regression dilution biasEur Heart J20032417192614522566
- EmbersonJWhincupPMorrisRWEvaluating the impact of population and high-risk strategies for The primary prevention of cardiovascular diseaseEur Heart J2004254849115039128
- ErhardtLRPearsonTABruckertEGuidelines and their implementation: a discussion document focused on the best appraches to drive improvementVascular Disease Prevention20041166774
- EUROASPIRE I and II GroupClinical reality of coronary prevention guidelines:a comparison of EUROASPIRE I and II in nine countries. EUROASPIRE I and II Group. European Action on Secondary Prevention by Intervention to Reduce EventsLancet2001357995100111293642
- FaergemanOChallenges to best practice: Why are guidelines not implementedEur Heart J Suppl19991Suppl JJ12J17
- FelmedenDCSpencerCGBlannADLow-density lipoprotein subfractions and cardiovascular risk in hypertension: relationship to endothelial dysfunction and effects of treatmentHypertension2003415283312623954
- GaedePVedelPLarsenNMultifactorial intervention and cardiovascular disease in patients with type 2 diabetesN Engl J Med20033483839312556541
- GilesTDBerkBCBlackHRExpanding the definition and classification of hypertensionJ Clin Hypertens2005750512
- GohlkeHKWinterMKaroffMCARRISMA: a new tool to optimize cardiovascular risk management in primary prevention [abstract]Circulation2005123794 Abstract
- GreenlandPKnollMDStamlerJMajor risk factors as antecedents of fatal and nonfatal coronary heart disease eventsJAMA2003290891712928465
- GrimmRJnrSvendsenKCardiovascular risk meter: A device for rapid estimation of cardiovascular disease mortality in clinical settingsJ Clin Hypertens20068Suppl A 5A236P-577MP-55 abstract
- GroverSAHemmelgarnBJosephLThe role of global risk assessment in hypertension therapyCan J Cardiol2006226061316755316
- HaffnerSMLehtoSRonnemaaTMortality from coronary heart disease in subjects with type 2 diabetes and in nondiabetic subjects with and without prior myocardial infarctionN Engl J Med1998339229349673301
- HoPMRumsfeldJSMasoudiFAEffect of medication nonadherence on hospitalization and mortality among patients with diabetes mellitusArch Intern Med2006a16618364117000939
- HoPMSpertusJAMasoudiFAImpact of medication therapy discontinuation on mortality after myocardial infarctionArch Intern Med2006b1661842717000940
- HobbsFDErhardtLAcceptance of guideline recommendations and perceived implementation of coronary heart disease prevention among primary care physicians in five European countries: the Reassessing European Attitudes about Cardiovascular Treatment (REACT) surveyFam Pract20021959660412429661
- HuxleyRBarziFWoodwardMExcess of fatal coronary heart disease associated with diabetes in men and women: meta-analysis of 37 prospective cohort studiesBMJ200633273816371403
- International Diabetes FederationDiabetes Atlas3 [online]. URL: http://www.eatlas.idf.org/media/
- JacksonRLawesCMBennettDATreatment with drugs to lower blood pressure and blood cholesterol based on an individual’s absolute cardiovascular riskLancet20053654344115680460
- JohnsonMLPietzKBattlemanDSTherapeutic goal attainment in patients with hypertension and dyslipidemiaMed Care200644394616365611
- Joint British SocietiesJBS 2: Joint British Societies’ guidelines on prevention of cardiovascular disease in clinical practiceHeart200591Suppl 5v1v5216365341
- JuliusSKjeldsenSEWeberMOutcomes in hypertensive patients at high cardiovascular risk treated with regimens based on valsartan or amlodipine: the VALUE randomised trialLancet200436320223115207952
- KannelWBFifty years of Framingham Study contributions to understanding hypertensionJ Hum Hypertens2000a14839010723112
- KannelWBRisk stratification in hypertension: new insights from the Framingham StudyAm J Hypertens2000b133S10S10678282
- KhanNAMcAlisterFARabkinSWThe 2006 Canadian hypertension education program recommendations for the management of hypertension: Part II – TherapyCan J Cardiol2006225839316755313
- KnappPRaynorDKBerryDCComparison of two methods of presenting risk information to patients about the side effects of medicinesQual Saf Health Care2004131768015175486
- LawMRWaldNJThompsonSGBy how much and how quickly does reduction in serum cholesterol concentration lower risk of ischaemic heart diseaseBMJ1994308367728043072
- LernerDJKannelWBPatterns of coronary heart disease morbidity and mortality in the sexes: a 26-year follow-up of the Framingham populationAm Heart J1986111383903946178
- LiaoDMoJDuanYThe joint effect of hypertension and elevated LDL-cholesterol on CHD is beyond additiveEur Heart J200425abstract suppl235 abstract #1377
- Lloyd-JonesDMLeipEPLarsonMGPrediction of lifetime risk for cardiovascular disease by risk factor burden at 50 years of ageCirculation2006113791816461820
- LynchTMedication costs as a primary cause of nonadherence in the elderlyConsult Pharm200621143616524358
- MacGregorKHandleyMWongSBehavior-change action plans in primary care: a feasibility study of cliniciansJ Am Board Fam Med2006192152316672674
- MacMahonSRodgersABlood pressure, antihypertensive treatment and stroke riskJ Hypertens Suppl199412S5S147769492
- McManusBINTERHEART: nine factors that could save your lifeHealthc Q200582815715328
- McMurrayJThe health economics of the treatment of hyperlipidemia and hypertensionAm J Hypertens19991299S104S10555609
- ManciaGTotal cardiovascular risk:a new treatment conceptJ Hypertens Suppl200624S17S2416601556
- ManciaGDe BackerGDominiczakA2007 Guidelines for the Management of Arterial Hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC)J Hypertens20072511058717563527
- Medical Research CouncilWhy 6g? A summary of the scientific evidence for the salt intake target2006CambridgeMedical Research Council
- MeyerGMervalRTedguiAEffects of pressure-induced stretch and convection on low-density lipoprotein and albumin uptake in the rabbit aortic wallCirc Res199679532408781486
- MurrayCJLopezADAlternative projections of mortality and disability by cause 1990–2020: Global Burden of Disease StudyLancet199734914985049167458
- NatarajanSLiaoYCaoGSex differences in risk for coronary heart disease mortality associated with diabetes and established coronary heart diseaseArch Intern Med200316317354012885690
- National Cholesterol Education ProgramExecutive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III)JAMA200128524869711368702
- NeatonJDWentworthDSerum cholesterol, blood pressure, cigarette smoking, and death from coronary heart disease. Overall findings and differences by age for 316,099 white men. Multiple Risk Factor Intervention Trial Research GroupArch Intern Med199215256641728930
- NissenSETuzcuEMSchoenhagenPEffect of intensive compared with moderate lipid-lowering therapy on progression of coronary atherosclerosis:a randomized controlled trialJAMA200429110718014996776
- O’MearaJGKardiaSLArmonJJEthnic and sex differences in the prevalence, treatment, and control of dyslipidemia among hypertensive adults in the GENOA studyArch Intern Med200416413131815226165
- PiloteLHoVLavoieFCost-effectiveness of lipid-lowering treatment according to lipid levelCan J Cardiol200521681716003451
- PlummerCJWhat’s in the CARDSDiab Med20062371114
- PrimatestaPPoulterNRLipid concentrations and the use of lipid lowering drugs:evidence from a national cross sectional surveyBMJ20003211322511090516
- PuskaPComprehensive cardiovascular community control programmes in Europe1988CopenhagenWHO Regional Office for Europe EURO Reports and Studies 106
- PuskaPVartiainenETuomilehtoJChanges in premature deaths in Finland:successful long-term prevention of cardiovascular diseasesBull World Health Organ199876419259803593
- RakugiHYuHKamitaniALinks between hypertension and myocardial infarctionAm Heart J1996132213218677859
- RaynerMEuropean Cardiovascular Disease Statistics2000
- ReavenGMLithellHLandsbergLHypertension and associated metabolic abnormalities – the role of insulin resistance and the sympathoadrenal systemN Engl J Med1996334374818538710
- Rodriguez-PorcelMLermanLOHerrmannJHypercholesterolemia and hypertension have synergistic deleterious effects on coronary endothelial functionArterioscler Thromb Vasc Biol2003238859112663373
- RosamondWFlegalKFridayGHeart disease and stroke statistics–2007 update:a report from the American Heart Association Statistics Committee and Stroke Statistics SubcommitteeCirculation2007115e69e17117194875
- SafranGNeumanPSchoenCPrescription drug coverage and seniors: findings from a 2003 national surveyHealth Aff2005Jan-JunSuppl Web ExclusivesW5-152W5-166
- SamuelssonOWilhelmsenLAnderssonOKCardiovascular morbidity in relation to change in blood pressure and serum cholesterol levels in treated hypertension. Results from the primary prevention trial in Goteborg, SwedenJAMA19872581768763625987
- SeverPSDahlöfBPoulterNRPrevention of coronary and stroke events with atorvastatin in hypertensive patients who have average or lower-than-average cholesterol concentrations, in the Anglo-Scandinavian Cardiac Outcomes Trial–Lipid Lowering Arm (ASCOT-LLA): a multicentre randomised controlled trialLancet200336111495812686036
- SimpsonEBeckCRichardHDrug prescriptions after acute myocardial infarction:dosage, compliance, and persistenceAm Heart J20031454384412660666
- SoumeraiSBPierre-JacquesMZhangFCost-related medication nonadherence among elderly and disabled Medicare beneficiaries:a national survey 1 year before the medicare drug benefitArch Intern Med200616618293517000938
- StamlerJVaccaroONeatonJDDiabetes, other risk factors, and 12-yr cardiovascular mortality for men screened in the Multiple Risk Factor Intervention TrialDiabetes Care199316434448432214
- SullivanLMMassaroJMD’AgostinoRBSrPresentation of multivariate data for clinical use:The Framingham Study risk score functionsStat Med20042316316015122742
- ThomasFBeanKGuizeLCombined effects of systolic blood pressure and serum cholesterol on cardiovascular mortality in young (<55 years) men and womenEur Heart J2002235283511922642
- ThomasTSImproving care with nurse case managers:practical aspects of designing lipid clinicsAm J Cardiol19978062H65H
- ThomsenTFDavidsenMIbsenHA new method for CHD prediction and prevention based on regional risk scores and randomized clinical trials; PRECARD and the Copenhagen Risk ScoreJ Cardiovasc Risk20018291711702035
- TurnbullFEffects of different blood-pressure-lowering regimens on major cardiovascular events:results of prospectively-designed overviews of randomised trialsLancet200336215273514615107
- VartiainenEPuskaPPekkanenJChanges in risk factor explain changes in mortality from ischaemic heart disease in FinlandBMJ19943092378044063
- VasanRSBeiserASeshadriSResidual lifetime risk for developing hypertension in middle-aged women and men: The Framingham Heart StudyJAMA200228710031011866648
- WaldNJLawMRA strategy to reduce cardiovascular disease by more than 80%BMJ2003326141912829553
- WeiLWangJThompsonPAdherence to statin treatment and readmission of patients after myocardial infarction:a six year follow up studyHeart2002882293312181210
- WildSRoglicGGreenAGlobal prevalence of diabetes:estimates for the year 2000 and projections for 2030Diabetes Care20042710475315111519
- WilsonPWD’AgostinoRBLevyDPrediction of coronary heart disease using risk factor categoriesCirculation1998971837479603539
- WongNDLopezVTangSPrevalence, treatment, and control of combined hypertension and hypercholesterolemia in the United StatesAm J Cardiol200698204816828593
- [WHO] World Health OrganizationCardiovascular disease:prevention and control2005GenevaWorld Health Organization
- YoonKHLeeJHKimJWEpidemic obesity and type 2 diabetes in AsiaLancet20063681681817098087
- YusufSHawkenSOunpuuSEffect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study):case-control studyLancet20043649375215364185
- ZimmermanEMHorton-La ForgeBDetection and prevention of cardiac risk factors:health risk assessment and targeted follow-up in a managed care populationJ Cardiovasc Nurs19961127389069029