Abstract
Nebivolol is a third generation beta-blocker, which can be distinguished from other beta-blockers by its hemodynamic profile. It combines beta-adrenergic blocking activity with a vasodilating effect mediated by the endothelial L-arginine nitric oxide (NO) pathway. The effects of nebivolol have been compared with other beta-blockers and also with other classes of antihypertensive agents. In general, response rates to treatment are higher, and the frequency and severity of adverse events are either comparable or lower with nebivolol. Nebivolol is also effective in reducing cardiovascular morbidity and mortality in elderly patients with heart failure, regardless of the initial ejection fraction. Endothelium-derived NO is important in the regulation of large arterial stiffness, which in turn is a major risk factor for cardiovascular disease. Treatment with nebivolol increases the release of NO from the endothelium and improves endothelial function, leading to a reduction in arterial stiffness. Decreased arterial stiffness has beneficial hemodynamic effects including reductions in central aortic blood pressure. Unlike first generation beta-blockerrs, vasodilator beta-blockerrs such as nebivolol have favorable hemodynamic effects, which may translate into improved cardiovascular outcomes in patients with hypertension.
Introduction
Hypertension is a major risk factor for cardiovascular disease, and aggressive reduction of blood pressure can significantly improve cardiovascular outcomes (CitationStaessen et al 2003). However, there is still debate as to whether it is blood pressure reduction per se or the antihypertensive agent used that is most important in terms of improving cardiovascular outcome. The latest guidelines issued by the National Institute for Clinical Excellence (NICE) for England and Wales recommend an angiotensin-converting enzyme inhibitor (or an angiotensin receptor blocker if an ACE inhibitor is not tolerated) as first-line treatment for hypertension in patients less than 55 years old (CitationNICE 2006). In patients over 55 years and in black patients of any age, the recommended first-line therapy is either a calcium channel blocker or a thiazide-type diuretic.
The NICE guidelines no longer recommend beta-blockers for the first or second line treatment of hypertension. This recommendation was prompted by two recent meta-analyses which showed that despite reducing blood pressure, beta blockade was not effective in reducing cardiovascular events when compared with either placebo or other antihypertensive agents (CitationCarlberg et al 2004; CitationLindholm et al 2005). Beta-blockers have also recently been shown to increase the risk of type 2 diabetes, especially if treatment is in combination with a thiazide-type diuretic. However, atenolol was the beta-blocker used in most of these studies and, given the relative lack of clinical outcome data from trials of treating hypertension with beta-blockers other than atenolol, it is unclear whether this conclusion applies to all beta-blockers.
Isolated systolic hypertension is associated with increased large artery stiffness, a strong independent predictor of cardiovascular risk. Recently endothelium-derived nitric oxide (NO) has been shown to be involved in the regulation of large arterial stiffness, with a reduced bioavailability of NO production linked to increased arterial stiffness (CitationKinlay et al 2001; CitationWilkinson et al 2002; CitationSchmitt et al 2005). Arterial stiffening associated with age and disease has therefore become a new and important therapeutic target in terms of blood pressure reduction and cardiovascular disease prevention. Drugs such as nebivolol that reduce blood pressure and improve endothelial function may be especially useful in this regard and should be considered as an alternative first-line treatment for hypertension and in elderly patients with chronic heart failure.
Nebivolol
Nebivolol is a third generation beta-blocker, which can be distinguished from other beta-blockers by its hemodynamic profile. The hemodynamic effects of nebivolol are due to its vasodilator properties including a reduction in systemic vascular resistance and an increase in cardiac output (CitationRitter 2001). It is the most beta-1-selective adrenoceptor antagonist currently in clinical use and has no alpha-1-blocking action (CitationVan Bortel et al 1997). The enantiomers have different pharmacological properties. The d-isomer provides the beta-blocking component (CitationVan Nueten and De Cree 1998) and both the d- and l-isomers have an endothelial NO-dependent vasodilating effect. Thus racemic nebivolol is needed for the drug to be most effective. Such characteristics are in contrast to those of carvedilol which also has vasodilatory and anti-inflammatory properties, but in this case due to its ability to block alpha1 receptors. The effects of carvedilol on NO bioactivity also remain unclear.
Nebivolol is rapidly absorbed after oral administration of a standard 5-mg dose and reaches peak plasma levels between 30 minutes to 2 hours after intake. It is extensively metabolized and excretion is mainly in the feces and urine. The pharmacokinetics of nebivolol are not affected by age. However, the recommended starting dose for patients over 65 years is 2.5 mg a day. This is in line with many other antihypertensive treatments where dosage is lowered for elderly patients.
Nebivolol (5 mg) is indicated for the treatment of essential hypertension and, in elderly patients ≥70 years, for the treatment of stable mild and moderate chronic heart failure in addition to standard therapies. A starting dose of 2.5 mg is suggested in patients over 65 years or in patients with renal insufficiency.
Nebivolol combines beta-adrenergic blocking activity with a vasodilating effect via increased NO availability, mediated by the endothelial L-arginine NO pathway, leading to a reduction in peripheral vascular resistance. Treatment with nebivolol also leads to improvements in left ventricular function in patients with heart failure (CitationUhlir et al 1991; CitationErdogan et al 2007; CitationLombardo et al 2006), and arterial compliance (CitationVan Merode et al 1989). Left ventricular function is preserved and left ventricular mass is reduced in hypertensive patients with left ventricular hypertrophy (CitationStoleru et al 1993).
Hypertensive patients are at high risk of coronary artery disease and subsequent impaired cardiac function (CitationRobertson and Ball 1994) and congestive heart failure. Endothelial dysfunction, characterized by decreased bioavailability of NO, also occurs early in various forms of cardiovascular disease. NO has powerful antiatherogenic effects and a decrease in NO production is associated with a number of cardiovascular risk factors including hypertension, diabetes mellitus and hypercholesterolemia. Endothelial dysfunction may therefore contribute to the pathogenesis of atherosclerosis in hypertension (CitationMoncada 1994). Treatment with nebivolol may thus favorably impact on the vascular complications of hypertension either directly by reducing blood pressure or indirectly by increasing the bioavailability of NO. In healthy volunteers, nebivolol (5 mg) decreases systemic vascular resistance with no impairment of left ventricular function (CitationVan de Water et al 1988). In addition, chronic treatment with nebivolol maintains left ventricular function in healthy volunteers and in patients with hypertension (CitationDe Cree et al 1991), acute myocardial infarction and congestive heart failure (CitationStoleru et al 1993).
Central aortic pressure is a strong predictor of cardiovascular morbidity and mortality but classic beta-blockers such as atenolol have little effect on reducing central aortic pulse pressure in hypertensive patients. Studies comparing atenolol with other antihypertensive agents show that although decreases in peripheral blood pressure are similar, treatment with atenolol results in significantly less reduction of central aortic pressure compared with either fosinopril (CitationChen et al 1995) or eprosartan (CitationDhakam et al 2006). Improvements in arterial stiffness and arterial compliance are also greater with calcium channel blockers, angiotensin-converting enzyme inhibitors, and angiotensin II receptor blockers compared with atenolol (CitationResnick and Lester 2002).
The lack of efficacy of atenolol in reducing central pressure can have a direct effect on cardiovascular outcomes. In the CAFE study (CitationWilliams et al 2006) both brachial and aortic pressures were measured using pulse wave analysis in 2199 patients originally enrolled for the ASCOT trial. Patients treated with amlodipine/perindopril had greater reductions in central aortic systolic pressure and central aortic pulse pressure compared with patients given atenolol/bendrofluazide, even though reductions in brachial blood pressure were similar across the treatment groups. In addition, central aortic pulse pressure was an independent determinant of cardiovascular outcomes and may help to explain why, in the ASCOT trial, clinical outcomes were worse in patients treated with atenolol/bendrofluazide.
Atenolol may be less effective at reducing central aortic pressure because of its effects on reducing heart rate which may enhance the effect of wave reflections (CitationWilkinson et al 2006). The additional vasodilatory effects of nebivolol contribute to a lower reduction in heart rate, and the subsequent decrease in wave reflection together with improvements in arterial stiffness, and endothelial dysfunction may offset such deleterious hemodynamic effects and thus lower central pressure more than atenolol. This may translate clinically into greater reductions in cardiovascular morbidity and mortality than those seen with traditional beta-blockers (CitationKelly et al 1989; CitationPedersen and Cockcroft 2006), although this remains as yet unproven.
Clinical efficacy of nebivolol in hypertension
The efficacy of nebivolol monotherapy has been extensively studied in patients with mild to moderate hypertension. Early double-blind, placebo-controlled studies showed significant reductions of blood pressure with a daily dose of 5 mg nebivolol (CitationVan Bortel and Van Baak 1992; CitationVan Nueten et al 1997a). Nebivolol was equally effective in black patients, with a notable absence of typical side-effects usually associated with beta-blockade. Nebivolol did not impair Quality of life, measured with the Inventory of Subjective Health (ISH), and the frequency of adverse events was similar between nebivolol and placebo (CitationVan Bortel et al 1993).
A recent follow-up study was conducted in order to establish whether the reported efficacy and safety of nebivolol can be generalized in a large nationwide study (CitationCleophas et al 2006). A total of 6356 patients with mild hypertension were treated with nebivolol for 6 weeks. No serious adverse events occurred during the study, and the occurrence of minor adverse events was very limited. Blood pressure was significantly reduced and the efficacy of nebivolol monotherapy and add-on therapy was similar. Nebivolol was also highly effective in patients with isolated systolic hypertension.
CitationCleophas et al (2001) have assessed the long-term efficacy of nebivolol monotherapy. The study found a greater reduction in blood pressure and a higher percentage of responders after 6 months of nebivolol treatment. Nebivolol was well tolerated and patients reported a better feeling of general well being compared with any previous monotherapies. Although current guidelines recommend the adjustment of antihypertensive drug therapy after 6–8 weeks of treatment (CitationWHO-ISH 1999), such a strategy may not be appropriate for optimal nebivolol treatment.
In a 6-week observational study, nebivolol reduced both systolic and diastolic blood pressures and, unlike first generation beta-blockerrs, there were significant reductions in cholesterol, triglycerides, and blood sugar (CitationFallois and Faulhaber 2001). Results of studies comparing the efficacy and safety of nebivolol compared with other beta-blockers and other classes of antihypertensive agents generally find response rates to treatment are higher, and the frequency and severity of adverse events are either comparable or lower with nebivolol.
Nebivolol vs other beta-blockers
The antihypertensive effects of nebivolol are similar to those of the classic beta-blockers but the unique hemodynamic profile of nebivolol may contribute to its additional reported benefits. For example, in a double blind, randomized study in patients with untreated essential hypertension (CitationKamp et al 2003), both nebivolol (5 mg/day) and atenolol (100 mg/day) significantly reduced blood pressure to a similar extent. However, nebivolol also significantly reduced heart rate and peripheral resistance and increased stroke volume, leading to a small increase in cardiac output whereas cardiac output was significantly decreased and peripheral resistance increased with atenolol. The improvements in diastolic function with nebivolol highlight its potential use in the treatment of heart failure.
A separate double blind, randomized, parallel group trial compared patients treated for 4 weeks with nebivolol (5 mg/day), atenolol (50 mg/day), or placebo. Both nebivolol and atenolol significantly reduced blood pressure compared with placebo while nebivolol had no orthostatic effects and was better tolerated than atenolol (CitationVan Nueten et al 1998b). Similar results were found when nebivolol was compared with metoprolol (CitationUhlir et al 1991).
The unique hemodynamic profile of nebivolol may also contribute to the maintenance of exercise capacity compared with other beta-blockers. In a double blind, placebo-controlled, cross-over study of exercise tolerance in healthy volunteers given nebivolol (5 mg) or atenolol (100 mg) for 2 weeks, exercise capacity was lower and fatigue higher with atenolol compared with nebivolol (CitationVan Bortel and Van Baak 1992). Nebivolol also significantly decreased the total peripheral resistance during exercise compared with placebo.
Nebivolol vs other classes of antihypertensive agents
Nebivolol is an effective antihypertensive agent with a superior tolerability profile in comparison with other classes of antihypertensive agents. In a double-blind study comparing hypertensive patients treated with nebivolol (5 mg) or the angiotensin-converting enzyme inhibitor enalapril (10 mg) for 3 months, the decrease in blood pressure was significantly higher and response rates were higher with nebivolol (CitationVan Nueten et al 1997b). The incidence of cough was also higher with enalapril.
Although nebivolol (5 mg) and the calcium antagonist nifedipine (20 mg) were equally effective in lowering blood pressure, nebivolol also significantly reduced heart rate (CitationVan Nueten et al 1998a) and adverse events associated with nifedipine treatment caused a significantly higher number of patients to withdraw from the study compared with nebivolol-treated patients. Heart rate was also significantly reduced with nebivolol in a study comparing nebivolol (2.5–5 mg) with the calcium channel blocker amlodipine (5–10 mg) in elderly patients with mild to moderate hypertension (CitationMazza et al 2002). A high heart rate is linked to an increased risk of death in the elderly (CitationPalatini et al 1999) and so an antihypertensive such as nebivolol that effectively lowers blood pressure and also lowers heart rate has dual benefits in this population.
Effects of nebivolol and the angiotensin receptor blocker losartan on quality of life and antihypertensive effects were compared in a double-blind, randomized, parallel group study (CitationVan Bortel et al 2005). Patients with hypertension were treated for 12 weeks with 5 mg of nebivolol or 50 mg of losartan once daily. Quality of life parameters did not differ between the two treatments and although both drugs decreased systolic blood pressure similarly, the decrease in diastolic blood pressure was significantly greater with nebivolol.
Type 2 diabetes
Endothelial dysfunction, leading to decreased bioavailability of NO, is one of the major underlying mechanisms linking cardiovascular risk factors such as hypertension, diabetes mellitus, and dyslipidemia to overt cardiovascular disease (CitationMason 2006). In addition, tight control of blood pressure is more effective at reducing cardiovascular events than tight control of blood sugar in diabetic patients (CitationPalatini et al 1999). Unlike some beta-blockerrs, nebivolol had no effect on insulin sensitivity and glucose tolerance (CitationFogari et al 1997) and may therefore have potential therapeutic benefits in patients with type 2 diabetes, especially as many diabetic patients develop hypertension during the course of their disease (CitationKannel et al 1991).
Arterial stiffness and cardiovascular risk
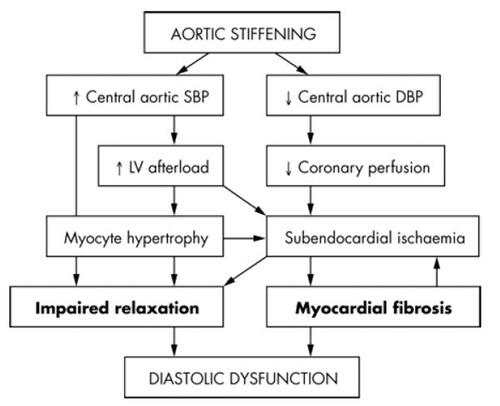
Arterial stiffness is a consequence of age (CitationKass 2002) and also of conditions such as diabetes and hypercholesterolemia, which cause premature vascular aging. Arterial stiffness is a major risk factor for cardiovascular disease and is an important predictor of mortality in hypertensive patients (CitationLaurent et al 2001). Increased aortic stiffness is also an independent predictor of diastolic dysfunction in patients with hypertensive heart disease (CitationYambe et al 2004; CitationMottram et al 2005) (see also ), and may also limit exercise tolerance in patients with dilated cardiomyopathy (CitationBonapace et al 2003). Patients who have heart failure with a preserved ejection fraction present with ventricular-systolic and arterial stiffening beyond that expected with age and/or hypertension (CitationKawaguchi et al 2003). Ventricular-vascular stiffening may also be greater in elderly women compared with elderly men (CitationRedfield et al 2005). Therefore, therapies aimed at reducing arterial stiffening may be of use in the treatment of diastolic dysfunction and heart failure.
Figure 1 Pathophysiological pathways through which aortic stiffness may contribute to the development of diastolic dysfunction. DBP, diastolic blood pressure; SBP, systolic blood pressure. Reproduced with permission from CitationMottram PM, Haluska BA, Leano R et al 2005. Relation of arterial stiffness to diastolic dysfunction in hypertensive heart disease. Heart, 91:1551–6. Copyright © 2005. BMJ Publishing Group Ltd.
Aortic pulse wave velocity (PWV) is a direct measure of arterial stiffness and may be a better predictor of future cardiovascular events compared with established risk factors such as age, hypertension, hypercholesterolemia, and diabetes. Studies using PWV find that increased arterial stiffness can predict cardiovascular risk in apparently healthy subjects (Citationvan Popele et al 2006), patients with hypertension (CitationBoutouyrie et al 2002), diabetes (CitationCruickshank et al 2002), end-stage renal failure (CitationBlacher et al 1999), and older individuals (CitationMeaume et al 2001). Arterial stiffness is also a possible risk factor for diastolic heart failure in hypertensive patients.
Pulse pressure, determined by large artery compliance and the pattern of left ventricular ejection, is a surrogate measure of arterial stiffness. In older patients, pulse pressure is a more important determinant of cardiovascular prognosis than mean arterial pressure in normotensive (CitationBenetos et al 1997), hypertensive (CitationBenetos et al 1998) and post-myocardial infarction populations (CitationMitchell et al 1997). These findings are confirmed by recent re-analysis (CitationMillar et al 1999) and meta-analysis (CitationBlacher et al 2000) of blood pressure lowering studies. Patients with congestive heart failure have an elevated central pulsatile load, which may help to explain why an increased pulse pressure is linked to an increase in clinical events in such patients (CitationMitchell et al 2001). Therapies that help to reduce such abnormal loading of the heart may be of use in the treatment of congestive heart failure.
An increased PWV and amplitude of the pressure wave reflected back to the aorta can cause increases in central aortic pressure, leading to increased left ventricular workload. Central aortic pressure is therefore an independent predictor of cardiovascular morbidity and mortality. Indeed, patients with high aortic pressure have a worse cardiovascular prognosis than patients with more effective control of central aortic pressure (CitationWilliams et al 2006).
Increased arterial stiffness is linked to endothelial dysfunction and reduced bioavailability of NO (CitationWilkinson et al 2004). Endothelial dysfunction, which is found in patients with most cardiovascular risk factors, may explain why these conditions are also associated with increased arterial stiffness at an early stage before the development of manifest atheroma (CitationCockcroft et al 1997). Therefore, drugs such as nebivolol that can increase NO production may help to reduce large artery stiffness which in turn may lead to a reduction of cardiovascular risk.
Antihypertensive agents differ in their effects on large arterial stiffness and pulse wave reflection (CitationChen et al 1995; CitationVan Bortel et al 1995; CitationBreithaupt-Grogler et al 1996; CitationDreary et al 2002). However, some of the beneficial effects observed may simply be due to the passive effect of lowering mean arterial pressure. The classical first generation beta-blockers such as atenolol have been shown to actually increase pulse wave reflection and central pressure acutely (CitationO’Rourke et al 1989). Nebivolol decreases arterial stiffness independently of any effect on blood pressure (CitationMcEniery et al 2004). Such vasodilating effects of nebivolol may help to reduce cardiovascular risk and improve outcomes, although such benefits need to be confirmed by the data from longer-term intervention trials.
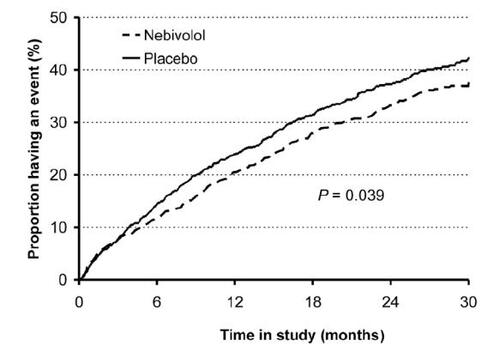
Clinical efficacy of nebivolol in chronic heart failure
A large, randomized, double-blind, placebo-controlled study (SENIORS study), has assessed the effects of nebivolol on mortality and morbidity in elderly patients ≥70 years with a history of heart failure (CitationFlather et al 2005). Patients were started on a dose of 1.25 mg nebivolol once daily and titrated to a target dose of 10 mg over a mean of seven weeks. Although nebivolol did not significantly reduce mortality, the composite risk of all cause mortality or cardiovascular hospital admission (time to first event) was significantly reduced by 15% with nebivolol compared with placebo (). This risk reduction was lower than that seen in previous trials with other beta-blockers (CitationShibata et al 2001). However, a sub-analysis of data from patients most similar to patients of these earlier trials showed the risk reduction to increase to 27%. Such results indicate that nebivolol has comparable benefits to those of other beta-blockers studied in heart failure. The benefits of treatment appeared after 6 months and the risk reduction increased if treatment was continued. The benefits of beta-blockade were independent of the initial ejection fraction and were observed even in patients with mild left ventricular dysfunction or preserved ventricular function. The vasodilating effects specific to nebivolol may help to improve tolerability in elderly patients with heart failure and support the use of this particular beta-blocker to treat heart failure in an elderly population.
Figure 2 Time to first occurrence of events (all cause death or hospital admission for a cardiovascular reason – primary endpoint). CitationFlather MD, Shibata MC, Coats AJ et al 2005. Randomized trial to determine the effect of nebivolol on mortality and cardiovascular hospital admission in elderly patients with heart failure (SENIORS). Eur Heart J, 26:215–25. Copyright © 2005. Oxford University Press.
Safety and tolerability
Nebivolol is well-tolerated in patients with hypertension. In clinical trials, reported adverse events are mostly mild to moderate in nature with an incidence similar to that observed with placebo (CitationTzemos et al 2001). Meta-analysis of the incidence of adverse events in double-blind, placebo-controlled trials finds the occurrence of adverse events to be no different with nebivolol compared with placebo (CitationLacourciere and Arnott 1994; CitationVan Nueten et al 1998a) and doses of up to 30 mg (6 times the recommended dose) have been well tolerated. Adverse events typical of classical beta-blockers are lower with nebivolol (CitationSteiner et al 1990). Classical beta-blockers may also alter plasma lipids in a potentially adverse manner (CitationCruickshank and Prichard 1987) whereas patients treated for 3 months with up to 10 mg daily nebivolol show no changes in plasma total cholesterol, triglycerides, lipoproteins, and apolipoproteins (CitationLacourciere et al 1992; CitationVan Nueten et al 1997b; CitationTzemos et al 2001). Quality of life, assessed using the Inventory of Subjective Health, is not impaired with nebivolol treatment (CitationVan Bortel et al 1993) and in general is similar to that reported with both atenolol and losartan (CitationVan Nueten et al 1998c; CitationVan Bortel et al 2005).
In the SENIORS study in elderly patients with chronic heart failure, the tolerability of nebivolol was similar to placebo (CitationFlather et al 2005). Drug-related adverse events were typical of those associated with beta-blockers and included hypotension, bradycardia and dizziness.
Endothelial function and the role of nitric oxide
The vascular endothelium modulates the tone and structure of the blood vessel smooth muscle by releasing various vasoactive and relaxing factors. One of the most important appears to be NO, a potent endogenous smooth muscle dilator, synthesized from the amino acid L-arginine, via the action of the constitutive enzyme nitric oxide synthase (CitationPalmer et al 1988). NO regulates basal vascular tone and blood pressure and also has powerful antiatherogenic properties. Endothelial dysfunction, manifested by reduced arterial vasodilation, is linked to abnormalities of the L-arginine/NO pathway resulting in decreased bioavailability of NO. Such dysfunction can therefore predispose to atherogenesis and may represent a link between conditions associated with increased cardiovascular risk (including diabetes, hypercholesterolemia and hypertension) and the development of overt cardiovascular disease (CitationMoncada 1994; CitationBrunner et al 2005).
Nebivolol can improve endothelial function directly via an effect on the endothelial L-arginine/NO pathway. Nebivolol relaxes precontracted canine coronary artery strips only if the endothelium is intact (CitationStoleru et al 1993) and this vasorelaxant effect is antagonized by nitro-L-arginine, an inhibitor of NO production, implying that the effect is mediated via release of endothelium-derived NO (CitationGao et al 1991).
Similar findings have been reported in vivo in a human vascular bed (CitationCockcroft et al 1995). Infusion of nebivolol into the brachial artery of healthy volunteers resulted in vasodilation and an increase in forearm blood flow by an average of 90% whereas atenolol had no effect. The vasodilator effect was significantly reduced with co-infusion of L-NMMA and this inhibition was abolished by L-arginine, the substrate for NO production, suggesting that the L-arginine/nitric oxide pathway was involved. Similar effects of nebivolol have also been demonstrated in experiments of nebivolol infusion into superficial hand veins (CitationBowman et al 1994) and in patients with hypertension (CitationDawes et al 1999). Oral nebivolol, but not atenolol, can also improve both basal and stimulated NO release relative to placebo in patients with essential hypertension (CitationTzemos et al 2001).
The improvements in endothelial function, secondary to release of NO, seen with nebivolol are of particular importance in black patients. This patient group has a reduced bioavailability of NO and alterations in endothelial function which may contribute to the greater susceptibility to cardiovascular disease observed in black patients. Pre-treatment with nebivolol of endothelial cells from black patients can increase NO bioavailability to levels similar to those in endothelial cells from white patients thereby helping to reverse endothelial dysfunction (CitationMason et al 2005).
Conclusion
Nebivolol is a third generation beta-blocker and is an effective antihypertensive with a good tolerability profile. Adverse events are generally mild with an incidence similar to placebo and there is a low incidence of many of the side effects usually associated with the use of classical beta-blockers. Nebivolol is also effective in reducing morbidity and mortality in elderly patients with heart failure, regardless of the initial ejection fraction. In addition to its effectiveness as an antihypertensive, nebivolol has a unique hemodynamic profile. Treatment with nebivolol increases NO bioavailability, improves endothelial function, leading to a reduction in arterial stiffness which in turn can help lower central aortic pressure. Such effects of nebivolol have the potential to reduce cardiovascular events. Additional studies are needed to determine the long term clinical relevance of these findings in the treatment of hypertension and cardiovascular disease.
References
- BenetosARudnichiASafarMPulse pressure and cardiovascular mortality in normotensive and hypertensive subjectsHypertension19983256049740626
- BenetosASafarMRudnichiAPulse pressure:a predictor of long-term cardiovascular mortality in a French male populationHypertension199730141059403561
- BlacherJGuerinAPPannierBImpact of aortic stiffness on survival in end-stage renal diseaseCirculation1999992434910318666
- BlacherJStaessenJGirerdXPulse pressure not mean pressure determines cardiovascular risk in older hypertensive patientsArch Int Med20001601085910789600
- BonapaceSRossiACicoiraMAortic distensibility independently affects exercise tolerance in patients with dilated cardiomyopathyCirculation20031071603812668493
- BoutouyriePTropeanoAIAsmarRAortic stiffness is an independent predictor of primary coronary events in hypertensive patientsHypertension20023910511799071
- BowmanAJChenCP-HFordGANitric oxide mediated venodilator effects of nebivololBr J Clin Pharmacol1994381992047826820
- Breithaupt-GroglerKLeschingerMBelzGGButzerRErbKde MeyCSinnWInfluence of antihypertensive therapy with cilazapril and hydrochlorothiazide on the stiffness of the aortaCardiovasc Drugs Ther19961049578723170
- BrunnerHCockcroftJRDeanfieldJEndothelial function and dysfunction. Part II: association with cardiovascular risk factors and diseases. A statement by the Working Group on Endothelins and Endothelial Factors of the European Society of HypertensionJ Hypertens2005232334615662207
- CarlbergBSamuelssonOLindholmLHAtenolol in hypertension: is it a wise choice?Lancet20043641684915530629
- ChenCP-HTingC-TLinS-JDifferent effects of fosinipril and atenolol on wave reflection in hypertensive patientsHypertension1995251034417737712
- CleophasTJAgrawalRLichtenthalANationwide efficacy-safety study of nebivolol in mildly hypertensive patientsAm J Ther200613192716772759
- CleophasTJGrabowskyINiemeyerMGLong-term efficacy of nebivolol monotherapy in patients with hypertensionCurr Ther Res20016245161
- CockcroftJRChowienczykPJBrettSENebivolol vasodilates human forearm vasculature: evidence for an L-arginine/NO-dependent mechanismJ Pharmacol Exp Ther19952741067717562470
- CockcroftJRWilkinsonIBWebbDJThe Trevor Howell Lecture: age, arterial stiffness and the endotheliumAgeing1997265360
- CruickshankJMPrichardBNCBeta-blockers in clinical practice1987EdinburghChurchill Livingstone
- CruickshankKRisteLAndersonSGAortic pulse-wave velocity and its relationship to mortality in diabetes and glucose intolerance. An integrated index of vascular function?Circulation200210620859012379578
- DawesMBrettSEChowienczykPJMantTGKThe vasodilator action of nebivolol in forearm vasculature of subjects with essential hypertensionJ Clin Pharmacol1999484603
- De CreeJGeukensHVerhaegenHNon-invasive cardiac haemodynamics of nebivololClin Drug Investig19913Suppl 12530
- DhakamZMcEnieryCMYasminAtenolol and eprosartan:differential effects on central blood pressure and aortic pulse wave velocityAm J Hypertens200619214916448896
- DrearyAJSchumannALMurfetHInfluence of drugs and gender on the arterial pulse wave and natiuretic peptide secretion in untreated patients with essential hypertensionClin Sci2002103493912401122
- ErdoganDGulluHCaliskanMNebivolol improves coronary flow reserve in patients with idiopathic dilated CardiomyopathyHeart2007933192417065184
- FalloisJVFaulhaberH-DNebivolol, a third generation beta-blocker:the current treatment of arterial hypertensionPraxis2001904354111293936
- FlatherMDShibataMCCoatsAJRandomized trial to determine the effect of nebivolol on mortality and cardiovascular hospital admission in elderly patients with heart failure (SENIORS)Eur Heart J2005262152515642700
- FogariRZoppiALazzariPComparative effects of nebivolol and atenolol on blood pressure and insulin sensitivity in hypertensive patients with type II diabetesJ Hum Hypertens19971175379416986
- GaoYNagaoTBondRANebivolol induces endothelium-dependent relaxations of canine coronary arteriesJ Cardiovasc Pharmacol19911796491714022
- KampOSieswerdaGTVisserCAComparison of effects on systolic and diastolic left ventricular function of nebivolol versus atenolol in patients with uncomplicated essential hypertensionAm J Cardiol200392344812888152
- KannelWBWilsonPWZhangTJThe epidemiology of impaired glucose tolerance and hypertensionAm Heart J19911211268732008855
- KassDAAge-related changes in venticular-arterial coupling: pathophysiologic implicationsHeart Fail Rev20027516211790922
- KawaguchiMHayIFeticsBCombined ventricular systolic and arterial stiffening in patients with heart failure and preserved ejection fraction: implications for systolic and diastolic reserve limitationsCirculation200310771472012578874
- KellyRDaleyJAvolioAArterial dilation and reduced wave reflection. Benefit of dilevalol in hypertensionHypertension19891414212737733
- KinlaySCreagerMAFukumotoMEndothelium-derived nitric oxide regulates arterial elasticity in human arteries in vivoHypertension20013810495311711496
- LacourciereYArnottWPlacebo-controlled comparison of the effects of nebivolol and low-dose hydrochlorothiazide as monotherapies and in combination on blood pressure and lipid profile in hypertensive patientsJ Hum Hypertens1994828388021909
- LacourciereYPoirierLLefebvreJComparative effects of a new cardioselective beta-blocker nebivolol and nifedipine sustained-release on 24-hour ambulatory blood pressure and plasma lipoproteinsJ Clin Pharmacol19923266061353507
- LaurentSBoutouyriePAsmarRAortic stiffness is an independent predictor of all-cause and cardiovascular mortality in hypertensive patientsHypertension20013712364111358934
- LindholmLHCarlbergBSamuelssonOShould beta-blockers remain first choice in the treatment of primary hypertension? A meta-analysisLancet200536615455316257341
- LombardoRMReinaCAbrignaniMGEffects of nebivolol versus carvedilol on left ventricular function in patients with chronic heart failure and reduced left ventricular systolic functionAm J CardiovascDrugs2006625963
- MasonRPNitric oxide mechanisms in the pathogenesis of global riskJ Clin Hypertens (Greenwich)2006831816894246
- MasonRPKalinowskiLJacobRFNebivolol reduces nitroxidative stress and restores nitric oxide bioavailability in endothelium of black AmericansCirculation2005112379580116330685
- MazzaAGil-ExtremeraBMaldonatoANebivolol vs amlodipine as first-line treatment of essential arterial hypertension in the elderlyBlood Press200211182812126265
- McEnieryCMSchmittMQasemANebivolol increases arterial distensibility in vivoHypertension2004443051015262912
- MeaumeSBenetosAHenryOFAortic pulse wave velocity predicts cardiovascular mortality in subjects. >70 years of ageArterioscler Thromb Vasc Biol20012120465011742883
- MillarJALeverAFBurkeVPulse pressure as a risk factor for cardiovascular events in the MRC Mild Hypertension TrialJ Hypertens19991710657210466460
- MitchellGFMoyeLABraunwaldESphygomanometrically determined pulse pressure is a powerful independent predictor of recurrent events after myocardial infarction in patients with impaired left ventricular functionCirculation1997964254609416890
- MitchellGFTardifJCArnoldJMPulsatile hemodynamics in congestive heart failureHypertension2001381433911751731
- MoncadaSNitric oxideJ Hypertens Suppl199412S35S97539493
- MottramPMHaluskaBALeanoRRelation of arterial stiffness to diastolic dysfunction in hypertensive heart diseaseHeart2005911551616287739
- NICEHypertension: Management of Hypertension in Adults in Primamry care – Partial update.NICE2006
- O’RourkeMFKellyRPAvolioAPEffects of arterial dilator agents on central systolic pressure and on left ventricular hydraulic loadAm J Cardiol198963381441
- PalatiniPCasigliaEJuliusSHigh heart rate: a risk factor for cardiovascular death in elderly menArch Int Med19991595859210090115
- PalmerRMAshtonDSMoncadaSVascular endothelial cells synthesize nitric oxide from L-arginineNature198833366463131684
- PedersenMECockcroftJRThe latest generation of beta-blockers:new pharmacologic propertiesCurr Hypertens Rep200682798616884657
- RedfieldMMJacobsenSJBorlaugBAAge- and gender-related ventricular-vascular stiffening: a community-based studyCirculation200511222546216203909
- ResnickLMLesterMHDifferential effects of antihypertensive drug therapy on arterial complianceAm J Hypertens200215109610012460707
- RitterJMNebivolol: endothelium-mediated vasodilating effectJ Cardiovasc Pharmacol200138Suppl 3S13S1611811387
- RobertsonJISBallSGHypertension for the clinician1994LondonW.B. Saunders
- SchmittMAvolioAQasemABasal NO locally modulates human iliac artery function in vivoHypertension2005462273115867142
- ShibataMFlatherMWangWSystematic review of the impact of beta blockers on mortality and hospital admissions in heart failureEur J Heart Failure200133517
- StaessenJWangJ-GThijsLCardiovascular prevention and blood pressure reduction: a quantitative overview updated until March 2003Hypertension200321105576
- SteinerSSFriedhoffAJWilsonBLAntihypertensive therapy and quality of life: comparison of atenolol, enalapril and propanololJ Hum Hypertens19904217252194029
- StoleruLWijnsWvan EyllCEffects of d-nebivolol and l-nebivolol on left ventricular systolic and diastolic function: comparison with dl-nebivolol and atenololJ Cardiovasc Pharmacol199322183907692155
- TzemosNLimPOMacDonaldTMNebivolol reverses endothelial dysfunction in essential hypertensionCirculation20011045111411479245
- UhlirOFejifusaMHavranekKNebivolol versus metoprolol in the treatment of hypertensionClin Drug Investig19913Suppl 110710
- Van BortelLMBulpittCJFiciFQuality of life and antihypertensive effect with nebivolol and losartanAm J Hypertens2005181060616296572
- Van BortelLMABBreedJGSJoostenJNebivolol in hypertension: a double-blind placebo-controlled multicenter study assessing its antihypertensive efficacy and impact on quality of lifeJ Cardiovasc Pharmacol199321856627687708
- Van BortelLMABde HoonJNJMKoolMJPharmacological properties of nebivolol in manEur J Clin Pharmacol199751379849049578
- Van BortelLMABKoolMJBoudierHAEffects of antihypertensive agents on local arterial distensibility and complianceHypertension19952653147649594
- Van BortelLMABVan BaakMAExercise tolerance with nebivolol and atenololCardiovasc Drugs Ther19926239471353367
- Van de WaterAJanssensWJVan NuetenLPharmacological and hemodynamic profile of nebivolol, a chemically novel, potent and selective beta1-adrenergic antagonistJ Cardiovasc Pharmacol198811552632455841
- Van MerodeTVan BortelLMABSmeetsFAVerapamil and nebivolol improve carotid artery distensibility in hypertensive patientsJ Hypertens1989Suppl 7S262S3
- Van NuetenLDe CreeJNebivolol: a comparison of the effects of dl-nebivolol, d-nebivolol, l-nebivolol, atenolol, and placebo on exercise-induced increases in heart rate and systolic blood pressureCardiovasc Drugs Therap199812339449825177
- Van NuetenLDupontAGVertommenCA dose-response trial of nebivolol in essential hypertensionJ Hum Hypertens1997a11139449140802
- Van NuetenLLacourciereYVyssoulisGNebivolol versus nifedipine in the treatment of essential hypertension: a double-blind randomised comparative trialAm J Therap1998a52374310099065
- Van NuetenLSchellingAVertommenCNebivolol versus enalapril in the treatment of essential hypertension:a double-blind randomised trialJ Hum Hypertens1997b11813199468009
- Van NuetenLTaylorFRRobertsonJINebivolol vs atenolol and placebo in essential hypertension: a double-blind randomised trialJ Hum Hypertens1998b12135409504355
- Van NuetenLTaylorFRRobertsonJISNebivolol versus atenolol and placebo in essential hypertension: a double-blind randomised trialJ Hum Hypertens1998c12135409504355
- van PopeleNMMattace-RasoFUVliegenthartRAortic stiffness is associated with atherosclerosis of the coronary arteries in older adults: the Rotterdam StudyJ Hypertens2006242371617082718
- WHO-ISHHypertension guidelinesJ Hypertens1999171518310067786
- WilkinsonIBFranklinSSCockcroftJRNitric oxide and the regulation of large artery stiffness: from physiology to pharmacologyHypertension200444112615262901
- WilkinsonIBMcEnieryCMCockcroftJRAtenolol and cardiovascular risk: an issue close to the heartLancet2006367627916503444
- WilkinsonIBQasemAMcEnieryCMNitric oxide regulates local arterial distensibility in vivoCirculation2002105213711790703
- WilliamsBLacyPSThomSMDifferential impact of blood pressure-lowering drugs on central aortic pressure and clinical outcomes: principal results of the Conduit Artery Function Evaluation (CAFE) studyCirculation200611312132516476843
- YambeMTomiyamaHHirayamaYArterial stiffening as a possible risk factor for both atherosclerosis and diastolic heart failureHypertens Res2004276253115750255