Abstract
Low-density lipoprotein (LDL) cholesterol concentration has been the prime index of cardiovascular disease risk and the main target for therapy. However, several lipoprotein ratios or “atherogenic indices” have been defined in an attempt to optimize the predictive capacity of the lipid profile. In this review, we summarize their pathophysiological aspects, and highlight the rationale for using these lipoprotein ratios as cardiovascular risk factors in clinical practice, specifying their cut-off risk levels and a target for lipid-lowering therapy. Total/high-density lipoprotein (HDL) cholesterol and LDL/HDL cholesterol ratios are risk indicators with greater predictive value than isolated parameters used independently, particularly LDL. Future recommendations regarding the diagnosis and treatment of dyslipidemia, including instruments for calculating cardiovascular risk or action guidelines, should include the lipoprotein ratios with greater predictive power which, in view of the evidence-based results, are none other than those which include HDL cholesterol.
Introduction
Estimation of cardiovascular risk has become the cornerstone of cardiovascular prevention. Although atherogenesis is a multifactorial process, abnormalities in lipoprotein metabolism are one of the key factors, representing around 50% of the population-attributable risk of developing cardiovascular disease.Citation1 Despite of the considerable progress made in cardiovascular disease management in recent decades, there is almost unanimous agreement among epidemiologists and clinicians that coronary risk assessment based exclusively on low-density lipoprotein (LDL) cholesterol is not optimal,Citation2 particularly in individuals at intermediate risk.Citation3 Efforts have been made in seeking emergent or new cardiovascular risk factors to improve cardiovascular disease prediction.Citation1 However, it must be emphasized that in an attempt to optimize the predictive capacity of the lipid profile, several lipoprotein ratios or “atherogenic indices” have been defined. These ratios can provide information on risk factors difficult to quantify by routine analyses and could be a better mirror of the metabolic and clinical interactions between lipid fractions. Since lipoprotein ratios are under-used in cardiovascular prevention, but can add to risk assessment, in this review, we briefly summarize their physiological and pathophysiological aspects. Furthermore, we highlight the rationale for using these lipoprotein ratios as cardiovascular risk factors in clinical practice, specifying their cut-off risk levels and a target for lipid-lowering therapy ().
Table 1 Risk categories and target levels for total cholesterol/HDL-C, LDL-C/HDL-C and apoB/apoA-I ratios, in primary and secondary prevention, stratified by genderCitation6,Citation7,Citation14
Total cholesterol/HDL cholesterol and LDL/HDL cholesterol ratios
The total/high-density lipoprotein (HDL) cholesterol ratio, known as the atherogenic or Castelli index and the LDL/HDL cholesterol ratio are two important components and indicators of vascular risk, the predictive value of which is greater than the isolated parameters. In this respect, an increase in total cholesterol concentration, and specifically LDL cholesterol, is an atherogenic lipid marker, whereas reduced HDL cholesterol concentration is correlated with numerous risk factors, including the components of the metabolic syndrome, and probably involves independent risk.Citation4 When total cholesterol, HDL cholesterol, and total/HDL cholesterol ratio are compared between an apparently healthy population and myocardial infarction survivors, the total/HDL cholesterol ratio is found to present less superposition of populations.Citation5 This illustrates the high discriminatory power for coronary heart disease presented by the total/HDL cholesterol ratio, as well as its great predictive capacity. The value of this parameter when the lipid profile is within desirable range should be emphasized. For example, total cholesterol of 231 mg/dL (5.89 mmol/L) and HDL cholesterol of 42 mg/dL (1.09 mmol/L) gives a total/HDL cholesterol ratio of 5.5, which indicates moderate atherogenic risk.Citation6 On the other hand, with the same level of total cholesterol, if HDL cholesterol were 60 mg/dL (1.55 mmol/L), the ratio would be 3.8. As total cholesterol/HDL ratio is considered a more sensitive and specific index of cardiovascular risk than total cholesterol, the Canadian working group has chosen this lipid ratio as a secondary goal of theraphy.Citation7
The LDL/HDL cholesterol ratio appears to be as useful as the total/HDL cholesterol ratio. Their similarity can be explained by the fact that approximately two thirds of plasma cholesterol are found in LDL and, consequently, total and LDL cholesterol are closely related. Like the total/HDL cholesterol ratio, LDL/HDL cholesterol may have more predictive power if triglyceridemia is taken into account.Citation8 Although, the increase in these ratios predicted a greater cardiovascular risk in a wide range of cholesterol or triglyceride concentrations, the risk is significantly higher when hypertriglyceridemia is present, as shown by the Helsinki Heart Study.Citation9
However, it is clear than when there is no reliable calculation of LDL cholesterol, as when triglyceridemia exceeds 300mg/dL (3.36 mmol/L), it is preferable to use the total/HDL cholesterol ratio; furthermore, the very-low-density lipoprotein (VLDL) fraction shows cholesterol enrichment in individuals with high triglyceride concentrations, and thus the LDL/HDL cholesterol ratio may underestimate the magnitude of the lipoprotein abnormality in these patients.
Individuals with a high total/HDL cholesterol or LDL/HDL cholesterol ratio have greater cardiovascular risk owing to the imbalance between the cholesterol carried by atherogenic and protective lipoproteins. This may be due to an increase in the atherogenic component contained in the numerator, a decrease in the anti-atherosclerotic trait of the denominator, or both.Citation10
Some studies have calculated inverse ratios, ie, HDL/total cholesterol and HDL/LDL cholesterol. Although their predictive value is identical but in the opposite order, few authors suggest they more clearly express the proportion of HDL cholesterol (protective) compared with the rest.Citation8
ApoB/ApoA-I ratio
Apolipoprotein (apo) B represents most of the protein content in LDL and is also present in intermediate-density lipoproteins (IDL) and VLDL. ApoA-I is the principal apolipoprotein in HDL. Both apolipoproteins, therefore, separately provide information for detecting high-risk individuals. ApoA-I is also believed to be a more reliable parameter for measuring HDL than cholesterol content since it is not subject to variation. Therefore, the apoB/apoA-I ratio is also highly valuable for detecting atherogenic risk, and there is currently sufficient evidence to demonstrate that it is better for estimating vascular risk than the total/HDL cholesterol ratio.Citation11–Citation14 The apoB/apoA-I ratio was stronger than the total cholesterol/HDL holesterol and LDL/HDL cholesterol ratios in predicting risk.Citation11 Furthermore, Walldius and colleagues have reported that addition of lipids, lipoproteins or any cholesterol ratio to apoB/apoA-I in risk models did not further improve the strong predictive value of apoB/apoA-I.Citation13
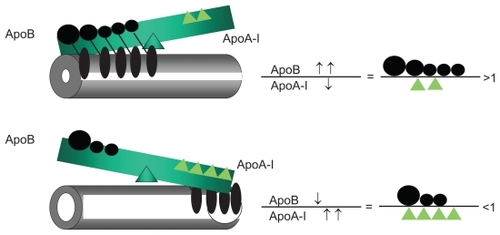
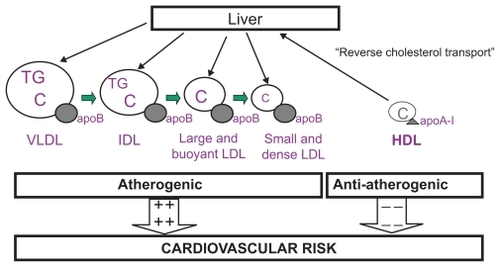
This ratio reflects the balance between two completely opposite processes (): transport of cholesterol to peripheral tissues, with its subsequent arterial internalization, and reverse transport to the liver.Citation15 shows that the greater the apoB/apoA-I ratio, the larger will be the amount of cholesterol from atherogenic lipoproteins circulating through the plasma compartment and likely to induce endothelial dysfunction and trigger the atherogenic process. On the other hand, a lower apoB/apoA-I ratio will lead to less vascular aggression by plasma cholesterol and increased and more effective reverse transport of cholesterol, as well as other beneficial effects, thereby reducing the risk of cardiovascular disease.
Figure 1 Atherogenic and anti-atherogenic lipoproteins. This diagram shows that there is one single apolipoprotein B (apoB) molecule in each large, buoyant or small, dense particle of very-low-density (VLDL), intermediate-density (IDL), and low-density lipoproteins (LDL). Therefore, apoB represents the total number of potentially atherogenic particles. Apolipoprotein A-I (apo A-I) is the principal protein component in high-density lipoproteins (HDL) and is responsible for starting reverse cholesterol transport. The balance between apoB and apoA-I is indicative of cardiovascular risk: the greater the ratio, the greater the risk.
Logarithmic transformation of the triglyceride/HDL cholesterol molar concentration ratio
The association between triglycerides and HDL cholesterol reflected by this ratio depicts the balance between atherogenic and protective lipoproteins. Known as the atherogenic plasma index, it shows a positive correlation with the HDL esterification rate (FERHDL) and an inverse correlation with LDL size.Citation16 Therefore, the phenotype of LDL and HDL particles is clearly synchronized with the FERHDL. Hypoalphalipoproteinemia and hypertriglyceridemia both induce an increase in the percentage of small HDL and small, dense LDL particles. Ultimately, the simultaneous use of triglycerides and HDL cholesterol in this ratio reflects the complex interactions of lipoprotein metabolism overall and can be useful for predicting plasma atherogenicity.Citation17 An atherogenic plasma index [log (triglycerides/HDL cholesterol)] over 0.5 has been proposed as the cut-off point indicating atherogenic risk.Citation16
LDL cholesterol/apoB ratio
Although apoB is not an apolipoprotein exclusive to LDL, since it is present in other atherogenic lipoprotein fractions such as IDL and VLDL, the LDL cholesterol/apoB concentration ratio provides approximate information on LDL particle size. In this respect, it has been suggested that a ratio of less than 1.3 would indicate the predominance of LDL particles with lower cholesterol content, consistent with small, dense LDL particles.Citation18 However, a study comparing LDL particle size determination by gradient-gel electrophoresis with the LDL cholesterol/apoB ratio in healthy and hyperlipidemic subjects failed to find a good correlation and did not recommend the use of this ratio as a surrogate LDL size marker.Citation19
Non-HDL cholesterol/HDL cholesterol ratio
Non-HDL cholesterol, which is total cholesterol minus HDL cholesterol, is a measure of the cholesterol in LDL, IDL and VLDL particles. Non-HDL cholesterol has therefore been recommended as a secondary therapeutic target in individuals with high triglyceride concentration, and it has been suggested that it could be a surrogate marker of serum apoB concentration in clinical practice. However, non-HDL cholesterol is not always strongly associated with apoB, particularly in the presence of hypertriglyceridemia.Citation20 The non-HDL cholesterol/HDL ratio is a lineal combination of total/HDL cholesterol. Although few studies have evaluated this lipoprotein ratio for predicting cardiovascular disease, and as it is a lineal combination of the results can be assumed to be similar to those of the total/HDL cholesterol or LDL/HDL cholesterol ratios.Citation21
Predictive power of lipoprotein ratios for cardiovascular risk
The evidence derived from large observational studies, including the Framingham Study,Citation22 the LRCPCitation23 and the PROCAM,Citation24,Citation25 suggests that the total/HDL cholesterol ratio is a more powerful coronary risk predictor than independently-used total cholesterol, LDL cholesterol and HDL cholesterol. The predictive value for the development of coronary events of the baseline total/HDL cholesterol and LDL/HDL cholesterol ratios in the placebo groups of WOSCOPS,Citation26 AFCAPS/TexCAPS,Citation27 and 4SCitation28 studies was higher than that of other lipid parameters in multivariate analyses. Indeed, the total/HDL cholesterol ratio was included in the Framingham equation to improve risk prediction.Citation29 The LRC-CPPT studyCitation5 analysed the ability of the total/HDL cholesterol ratio to predict coronary risk and compared it to other lipid metabolism variables in three large population-based cohorts: the men in the placebo group of the LRCP-CPPT study; a group of individuals of both sexes subject to follow-up in the Framingham Study; and a group of men and women without coronary disease included in the LRCP Mortality Follow-up Study. The groups of men and women from the Framingham Study and the men from the LRCP-CPPT control group were divided into deciles, using a primary lipid end-point, and the deciles were subsequently divided into terciles using a secondary lipid end-point. When total cholesterol and LDL cholesterol were used as primary end-points, the total/HDL cholesterol and LDL/HDL cholesterol ratios identified significantly high- and low-risk groups within the deciles. For example, when the LRCP-CPPT men were divided into deciles according to LDL cholesterol, the absolute difference in risk within each decile between individuals in the upper and lower terciles of the total/HDL cholesterol ratio was 13% (95% confidence intervals [CI]: 8.2%–17.7%). The results were similar when the LDL/HDL cholesterol ratio was used. When the LDL/HDL cholesterol and total/HDL cholesterol ratios were used as primary end-points, neither total nor LDL cholesterol identified high- or low-risk groups within the deciles. These results of the stratified analysis were confirmed in the logistic regression analysis and suggest that the total/HDL cholesterol ratio adds risk prediction power to total and LDL cholesterol values. However, no other lipid parameter adds predictive power to the total/HDL cholesterol ratio. On the other hand, no conclusive data were obtained in relation to the superiority of the total/HDL cholesterol ratio over the LDL/HDL ratio, or vice versa. Only in women was the total/HDL cholesterol ratio found to have greater predictive power, which could be explained by the fact that this ratio, and not LDL/HDL cholesterol, includes triglyceride-rich lipoproteins in the numerator (VLDL and IDL), and triglycerides are a more powerful coronary risk predictor in women than in men.Citation30 When there is no reliable calculation of LDL cholesterol, as occurs in individuals with serum triglycerides above 300 mg/dL (3.36 mmol/L), since in this scenario the Friedewald formula for estimating LDL cholesterol is not valid, the total/HDL cholesterol ratio will have to be used. The total/HDL cholesterol ratio was the best risk predictor in a subanalysis of the cohort of 14,916 men in the Physicians Health StudyCitation31 and, after adjusting for other factors, each unit increase in the ratio was found to be associated with a 53% increase in the risk of myocardial infarction. Similarly, in the cohort of 28,263 postmenopausal women undergoing a three-year follow-up in the Women’s Health Study,Citation32 among lipid variables, various inflammation markers and homocysteine, the only independent predictors of risk for a cardiovascular event were C-reactive protein and the total cholesterol/HDL cholesterol ratio. Other studiesCitation33,Citation34 have shown the total cholesterol/HDL cholesterol ratio to be the lipid parameter with the greatest predictive power with regard to the presence, severity and extension of coronary atherosclerosis in women.
The total/HDL cholesterol ratio has also been shown to be a good predictor of carotid intima-media thickness; it has greater power than the isolated variables and similar power to that of the apoB/apoA-I ratio and non-HDL cholesterol.Citation35 More controversial is the role of the ratio between the principal protein fractions of LDL and HDL, apoB and A-I, which is the apoB/apoA-I ratio, as contradictory results regarding its use for predicting cardiovascular risk and its relative value compared with the LDL/HDL cholesterol and total/HDL cholesterol ratios have been obtained in the different observational studies.Citation36,Citation37 In the Interheart study, which included around 30,000 subjects from 52 countries, the apoB/apoA-I ratio was the variable which predicted a larger proportion of risk of myocardial infarction. Indeed, nearly 50% of the population-attributable risk corresponded to that ratio.Citation1 However, the Interheart study did not include any other lipid measurement, such as HDL or LDL cholesterol, and thus did not compare the relative usefulness of this ratio. In a recent study conducted in 3,322 Framingham inhabitants of both sexes with a 15-year follow-up, the apoB/apoA-I ratio was not superior to the total/HDL cholesterol ratio.Citation38 In the EPIC-Norfolk study conducted in apparently healthy men and women, the apoB/apoA-I ratio was associated with the risk of future coronary events independently of the traditional lipid variables, including the total/HDL cholesterol ratio and the Framingham equation. However, the apoB/apoA-I ratio was not a better discriminatory factor between cases and controls than the total/HDL cholesterol ratio, and added little predictive power to the Framingham equation.Citation39 Recently, the Cardiovascular Risk in Young Finns StudyCitation40 has demonstrated that the apoB/apoA-I ratio measured in adolescence was higher than LDL/HDL cholesterol ratio in predicting increased carotid intima-media thickness in adulthood.
Considering these observations and given that apolipoprotein measurement methods are not as widely used as lipoprotein methods and the absence of consensus on reference values and therapeutic objectives, it would appear that the use of apoB/apoA-I ratio is limited for the time being.
Although the total/HDL cholesterol and LDL/HDL cholesterol ratios predict greater cardiovascular risk with a wide range of cholesterol or triglyceride concentrations, the risk is considerably higher in the presence of hypertriglyceridemia. In the Helsinki study,Citation41 the LDL/HDL cholesterol ratio was a powerful predictor of cardiovascular risk, mainly in subjects with elevated triglycerides. The greatest risk was observed in subjects with an LDL/HDL ratio >5 and triglycerides >200 mg/dL (2.24 mmol/L), who represented around 10% of the population studied; it was precisely this group which most benefited from treatment with gemfibrozil, with a remarkable 71% reduction in the incidence of coronary events, more than double that of the overall active-treatment group. In the cohort of 4,559 adult men in the PROCAM observational study,Citation24,Citation25 it was found that subjects with an LDL/HDL cholesterol ratio >5 presented more than six times the rate of coronary events of those with an LDL/HDL ratio <5; however, when the LDL/HDL cholesterol ratio was >5 and associated with triglycerides ≥200 mg/dL (2.24mmol/L), the risk was double that of subjects with triglycerides <200 mg/dL (2.24 mmol/L). In the Physicians Health Study,Citation31 this synergic effect was also found between the increase in the atherogenic/protective cholesterol ratio and hypertriglyceridemia.
Predicting the magnitude of the preventive effect
The total/HDL cholesterol and LDL/HDL cholesterol ratios are also good predictors of the degree of clinical benefit to be derived from lipid-lowering intervention.Citation10 In the LRC-CPPT with cholestyramine, the drops in the total/HDL cholesterol ratio in the active treatment group were associated with clinical benefit. In the Helsinki study, multivariate analysis of the relationship between the lipid changes induced by gemfibrozil and the incidence of cardiovascular events in the treated group showed better predictive value for changes in HDL cholesterol and the total/HDL cholesterol ratio. In the placebo group of the AFCAPS/TexCAPS study,Citation27 baseline LDL cholesterol had no predictive value for the incidence of coronary events, whereas predictive value was found in HDL cholesterol and the total/HDL cholesterol and LDL/HDL cholesterol ratios, both with greater significance than HDL cholesterol by adjusted logistic regression; in the active treatment group, only changes in apoB and the apoB/apoA-I ratio, which is largely equivalent to the LDL/HDL cholesterol ratio, predicted risk reduction. The total/HDL cholesterol ratio also had more predictive value than other lipid parameters in the control group of the 4S study;Citation28 treatment-induced changes in this ratio were the best risk predictors in the group receiving simvastatin, with an estimated 17.6% risk difference for every one-unit reduction in the ratio.
In two angiographic studies in which cholestyramine was used as a hypolipidemiant agent,Citation42,Citation43 changes in the total/HDL cholesterol or LDL/HDL cholesterol ratios were the only independent predictors of the benefit observed in coronary stenosis. The predictive capacity of the ratios in this study is also supported by data indicating that an increase in HDL cholesterol is associated with an independent effect on regression,Citation44 and that combined treatment with lipid-lowering agents which reduce LDL cholesterol or increase HDL cholesterol more than monotherapy would be associated with a net regression, in comparison with monotherapy, which would only slow down progression. In a meta-analysis of coronary atherosclerosis follow-up studies with intravascular ultrasound scans in patients treated with statins, the apoB/apoA-I and HDL/LDL cholesterol ratios were powerful predictors of changes in atheroma burden.Citation45 This analysis clearly shows that an increase in HDL cholesterol and apoA-I is fundamental, as is a reduction in LDL cholesterol and apoB, for halting progression of coronary atherosclerosis.
At least in secondary prevention, the predictive power of the ratios in relation to the benefit of intervention can be extended to countries with a lower prevalence of coronary disease such as Spain. In a cohort of 882 coronary patients included in the Hospital de Bellvitge Secondary Prevention Programme who were followed up for a mean of 34 months, those who reached the established therapeutic target, an LDL/HDL cholesterol ratio <3.7, or reduced ratio by ≥15%, reduced their risk of hospitalization for cardiovascular disease and death to less than half, compared with those who did not reach the target. Of the different lipid and nonlipid risk factors, reaching the LDL/HDL ratio objective had the greatest power to predict a favorable outcome in the multiple regression analysis adjusted for possible confounding factors.Citation46
What do lipoprotein ratios provide that other conventional risk variables do not?
Classic cardiovascular risk factors such as age, sex, smoking, diabetes, hypertension, high LDL and low HDL cholesterol levels have been widely analyzed and established as independent cardiovascular risk factors. Many other predictors, such as triglycerides, apoB, lipoprotein(a), homocysteine, C-reactive protein and others have also been studied. Furthermore, the total/HDL cholesterol and LDL/HDL cholesterol ratios are of great interest as major predictors of cardiovascular disease.
Guidelines for lipid management are based on LDL cholesterol concentrations, although other parameters including the total/HDL cholesterol index are better cardiovascular risk predictors than LDL cholesterol and have not been included.Citation47 The beneficial use of these indices as important cardiovascular risk predictors is based on multiple epidemiological studies which have shown that these ratios (total/HDL cholesterol and LDL/HDL cholesterol) have a greater correlation with cardiovascular disease and are therefore better predictors of cardiovascular disease than simple lipid parameters.Citation5,Citation31,Citation48
A study in 32,826 menopausal womenCitation49 with an eight-year follow-up, after adjusting for age, smoking, C-reactive protein levels, homocysteine, body mass index, family history, diabetes, hypertension, physical activity, and alcohol consumption, found a relative risk of cardiovascular disease (95% CI) of 0.6 (0.5–0.8) for HDL cholesterol; 1.3 (1.0–1.5) for triglyceride levels; 1.4 (1.1–1.7) for LDL cholesterol; 1.7 (1.4–2.1) for apoB concentration; 1.6 (1.3–1.9) for non-HDL cholesterol; 1.5 (1.3–1.9) for the LDL/HDL cholesterol index; and 1.6 (1.3–1.9) for the total/HDL cholesterol index. The total/HDL cholesterol index is therefore a good predictor of cardiovascular risk irrespective of other factors.
In a retrospective study with a 20-year follow-up of 1,439 men and 2,812 women with cardiovascular disease,Citation50 cardiovascular risk increased in relation to total/HDL cholesterol levels, regardless of total or LDL cholesterol. In men, the relative risk for quintile 5 over 1 of LDL cholesterol was 1.85, whereas the upper over the lower quintile of the total/HDL cholesterol ratio was 2.9. This cardiovascular risk difference between LDL cholesterol and total/HDL cholesterol was not found in women. The authors therefore conclude that men with elevated LDL cholesterol do not have to be treated aggressively if their total/HDL cholesterol index is low, and vice versa, with mild elevations of LDL cholesterol requiring more aggressive treatment if the total/HDL cholesterol ratio is high. This reveals that the total/HDL cholesterol ratio is an excellent cardiovascular risk predictor and a good parameter for deciding on the intensity and need for therapeutic intervention in each different situation.
Other authorsCitation51 studying subjects with peripheral arterial disease demonstrated the importance of the total/HDL cholesterol index in predicting atherosclerosis in this setting. Studying a cohort of 2,265 subjects with a five-year follow-up, they found disease progression to be significantly related to smoking, the total/HDL cholesterol index and plasma levels of lipoprotein(a) and C-reactive protein.
In an analysis of the Framingham Heart Study and the Coronary Primary Prevention Trial data,Citation52 LDL cholesterol and the total/HDL cholesterol and LDL/HDL cholesterol ratios were found to be good cardiovascular disease predictors. However, when vascular changes and cardiovascular risk after intervention were studied, both ratios were better cardiovascular risk reduction predictors than total cholesterol or LDL cholesterol. These ratios should therefore be used when assessing vascular risk and in the reduction of such risk after therapeutic intervention.
There is reason to believe that these lipoprotein ratios, mainly total/HDL cholesterol, based on two values directly measured in a clinical laboratory and which indicate the relationship or proportion between the atherogenic and antiatherogenic lipid fraction, have predictive power for cardiovascular disease and cardiovascular risk reduction after intervention superior to that of classic lipid parameters and should be used in regular clinical practice.
With regard to identifying the “best” lipoprotein ratio, there is an interesting contrast between the use of cut-off pointsCitation46 and quantiles.Citation50 Thus it must be taken into account that while cut-off points can provide clinical relevant information, with regard to comparing ratios it would seem more logical to use quantiles within the cohort/population.
Conclusions and recommendations
LDL cholesterol concentration has been the prime index of cardiovascular disease risk and the main target for therapy. However, data now suggest that total/HDL cholesterol and LDL/HDL cholesterol ratios are risk indicators with greater predictive value than isolated parameters used independently, particularly the former. These two indices can be regarded as similar; since two thirds of plasma cholesterol are found in LDL, total and LDL cholesterol are closely correlated. The predictive capacity of these ratios is supported by data suggesting that an increase in HDL cholesterol is more prevalently associated with plaque regression, while a decrease in LDL cholesterol would slow down progression. Both predict greater cardiovascular risk for a wide range of cholesterol concentrations. However, when there is no reliable determination of LDL cholesterol, as in cases of hypertriglyceridemia, it is preferable to use the total/HDL cholesterol ratio. This may be particularly interesting in patients with features of the metabolic syndrome.
ApoB constitutes most of the protein content of LDL, as does apoA-I for HDL, even as parameters subject to less variation. Therefore, the apoB/apoAI ratio is also of great value for detecting atherogenic risk and often better than the total/HDL and LDL/HDL cholesterol ratios.
We suggest that future recommendations regarding the diagnosis and treatment of dyslipidemia, including instruments for calculating cardiovascular risk or action guidelines, should include the lipoprotein ratios with greater predictive power which, in view of the results, are none other than those which include HDL cholesterol. Meanwhile, we propose that lipoprotein ratios should be routinely determined to assess the atherogeneity lipids disorders, mainly those characterized by an elevation in plasma triglycerides.
Disclosures
The authors report no conflicts of interest in this work.
References
- YusufSHawkenSÖunpuuSEffect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control studyLancet200436493795215364185
- SuperkoHRKingSIIILipid management to reduce cardiovascular risk: a new strategy is requiredCirculation200811756056818227396
- AradYGoodmanKJRothMNewsteinDGuerciADCoronary calcification, coronary disease risk factors, C-reactive protein, and atherosclerotic cardiovascular disease events: the St. Francis Heart StudyJ Am Coll Cardiol20054615816515992651
- AscasoJGonzález SantosPHernández MijaresAManagement of dyslipidemia in the metabolic syndrome. Recommendations of the Spanish HDL ForumAm J Cardiovasc Drugs20077395817355165
- KinosianBGlickHGarlandGCholesterol and coronary heart disease: predicting risks by levels and ratiosAnn Intern Med19941216416477944071
- GottoAMAssmannGCarmenaRThe ILIB lipid handbook for clinical practice: blood lipids and coronary heart disease2nd edNew York, NYInternational Lipid Information Bureau20005253201
- GenestJFrohlichJFodorGMcPhersonRthe Working Group on Hypercholesterolemia and Other DyslipidemiasRecommendations for the management of dyslipidemia and the prevention of cardiovascular disease: 2003 updateCMAJ200316992192414581310
- PintóXRosELípidos séricos y predicción del riesgo cardiovascular: importancia de los cocientes colesterol total/colesterol HDL y colesterol LDL/colesterol HDLClin Invest Arterioscl200012267284
- ManninenVTenkanenLKoskinenPJoint effects of serum triglyceride and LDL cholesterol and HDL cholesterol concentrations on coronary heart disease risk in the Helsinki Heart Study. Implications for treatmentCirculation19928537451728471
- CriquiMHGolomBAEpidemiologic aspects of lipid abnormalitiesAm J Med1998105Suppl 1A48S57S9707268
- WalldiusGJungerIAastveitAHolmeIFurbergCDSnidermanADThe apoB-apoA-I ratio is better than the cholesterol ratios to estimate the balance between the plasma proatherogenic and antiatherogenic lipoproteins and to predict coronary riskClin Chem Lab Med2004421355136315576296
- SnidermanADJungerIHolmeIAastveitAWalldiusGErrors that result from using the apoB/apoA-I ratio to identify the lipoprotein-related risk of vascular diseaseJ Intern Med200625945546116629851
- WalldiusGJungerIThe apoB/apoA-I ratio: a strong, new risk factor for cardiovascular disease and a target for lipid-lowering therapy – a review of evidenceJ Intern Med200625949351916629855
- HolmeIAastveitAHJungerIWalldiusGRelationships between lipoprotein components and risk of myocardial infarction: age, gender and short versus longer follow-up periods in the Apolipoprotein MOrtality RISk study (AMORIS)J Intern Med2008264303818298486
- ThompsonADaneshJAssociations between apolipoprotein B, apolipoprotein AI, the apolipoprotein B/AI ratio and coronary heart disease: a literature-based meta-analysis of prospective studiesJ Intern Med200625948149216629854
- DobiásováMFrohlichJThe plasma parameter log (TG/HDL-C) as an atherogenic index: correlation with lipoprotein particle size and esterification rate in apoB-lipoprotein-depleted plasma (FERHDL)Clin Biochem20013458358811738396
- DobiásováMAtherogenic index of plasma [Log (triglycerides/HDL-cholesterol)]: theoretical and practical implicationsClin Chem2004501113111515229146
- VegaGLBeltzWFGrundySMLow density lipoprotein metabolism in hypertriglyceridemic and normolipidemic patients with coronary heart diseaseJ Lipid Res1985261151263973508
- FuruyaDYagihashiANasuSLDL particle size by gradient-gel electrophoresis cannot be estimated by LDL-cholesterol/apolipoprotein B ratiosClin Chem2000461202120310926909
- SnidermanADSt-PierreACCantinBDagenaisGRDespresJPLamarcheBConcordance/discordance between plasma apolipoprotein B levels and the cholesterol indexes of atherosclerotic riskAm J Cardiol2003911173117712745098
- RaderDJDavidsonMHCaplanRJPearsJSLipid and apolipoprotein ratios: association with coronary artery disease and effects of rosuvastatin compared with atorvastatin, pravastatin, and simvastatinAm J Cardiol200391Suppl20C24C
- CastelliWJGarrisonRJWilsonPWFAbbotRDKalousdianSKannelWBIncidence of coronary heart disease and lipoprotein cholesterol levels. The Framingham StudyJAMA1986256283528383773200
- GroverSAPalmerCSCoupallLSerum lipid screening to identify high risk individuals for coronary death. The results of the Lipid Research Clinics prevalence cohortArch Intern Med19941546796848129502
- AssmannGSchulteHFunkeHvon EckardsteinASeedorfUMillerNEThe Prospective Cardiovascular Münster (PROCAM) StudyIdentification of high-risk individuals for myocardial infarction and the role of HDLHigh Density Lipoproteins and Atherosclerosis IIAmsterdam, The NetherlandsElsevier19895165
- AssmannGCullenPSchulteHThe Munster Heart Study (PROCAM). Results of follow-up at 8 yearsEur Heart J199819Suppl AA2A119519336
- The West of Scotland Coronary Prevention Study GroupBaseline risk factors and their association with outcome in the West of Scotland Coronary Prevention StudyAm J Cardiol1997797567629070554
- GottoAWhitneyESteinEARelation between baseline and on-treatment lipid parameters and first acute major coronary event in the Air Force/Texas Coronary Atherosclerosis Prevention Study (AFCAPS/TexCAPS)Circulation200010147748410662743
- PedersenTROlssonAGFaergemanOLipoprotein changes and reduction in the incidence of major coronary heart disease events in the Scandinavian Simvastatin Survival Study (4S)Circulation199897145314609576425
- AndersonKMWilsonPWOdellPMKannelWBAn updated coronary risk profile. A statement for health professionalsCirculation1991833563621984895
- HokansonJEAustinMAPlasma triglyceride level is a risk factor for cardiovascular disease independent of high-density lipoprotein cholesterol level: a meta-analysis of population-based prospective studiesJ Cardiovasc Risk199632132198836866
- StampferMJKraussRMMaJA prospective study of triglyceride level, low-density lipoprotein particle diameter, and risk of myocardial infarctionJAMA19962768828888782637
- RidkerPMHennekensCHBuringJERifaiNC-reactive protein and other markers of inflammation in the prediction of cardiovascular disease in womenN Engl J Med200034283684310733371
- HongMKRommPAReaganKGreenCERackleyCEUsefulness of the total cholesterol to high-density lipoprotein cholesterol ratio in predicting angiographic coronary artery disease in womenAm J Cardiol199168164616501746467
- NielsenNEOlssonAGSwahnEPlasma lipoprotein particle concentrations in postmenopausal women with unstable coronary artery disease. Analysis of diagnostic accuracy using receiver operating characteristicsJ Intern Med2000247435210672130
- FrontiniMGSrinivasanSRXuJHTangRBondMGBerensonGUtility of non-high-density lipoprotein cholesterol versus other lipoprotein measures in detecting subclinical atherosclerosis in young adults (The Bogalusa Heart Study)Am J Cardiol2007100646817599442
- SnidermanADFurbergCDKeechAApolipoproteins versus lipids as indices of coronary risk and as targets for statin treatmentLancet200336177778012620753
- BarterPJBallantyneCMCarmenaRApo B versus cholesterol in estimating cardiovascular risk and in guiding therapy: report of the thirty-person/ten-country panelJ Intern Med200625924725816476102
- IngelssonESchaeferEJContoisJHClinical utility of different lipid measures for prediction of coronary heart disease in men and womenJAMA200729877678517699011
- van der SteegWABoekholdtSMSteinEARole of the apolipoprotein B-apolipoprotein A-I ratio in cardiovascular risk assessment: a case-control analysis in EPIC-NorfolkAnn Intern Med200714664064817470832
- JuonalaMViikariJSKähönenMChildhood levels of serum apolipoproteins B and A-I predict carotid intima-media thickness and brachial endothelial function in adulthood: the Cardiovascular Risk in Young Finns StudyJ Am Coll Cardiol20085229329918634985
- ManninenVTenkanenLKoskinenPJoint effects of serum triglycerides and LDL cholesterol and HDL cholesterol concentration on coronary heart disease risk in the Helsinki Heart Study: implications for treatmentCirculation19928537461728471
- BrensikeJELevyRIKelseySFEffects of therapy with cholestyramine on progression of coronary arteriosclerosis: results of the NHLBI type II coronary intervention studyCirculation1984693133246360414
- WattsGFLewisBBruntJNHEffects on coronary artery disease of lipid-lowering diet, or diet plus cholestyramine, in the St. Thomas’ Atherosclerosis Regression Study (STARS)Lancet19923395635691347091
- BrownBGFusterVFusterVRossRTopolEJImpact of management in stabilization of coronary diseaseAtherosclerosis and Coronary Artery DiseasePhiladelphia, PALippincott-Raven1996191205
- NicholsSjTuzcuEMSipahiIStatins, high-density lipoprotein cholesterol, and regression of coronary atheroscleorsisJAMA200729749950817284700
- PintóXMecoJFCorbellaEPrograma de prevención secundaria de la arteriosclerosis de un hospital universitario. Resultados y factores predictivos del curso clínicoMed Clin (Barc)200312076877212797928
- HsiaSHPanDBerookimPLeeMLA population-based, cross-sectional comparison of lipid-related indexes for symptoms of atherosclerotic diseaseAm J Cardiol2006981047105217027569
- RidkerPMStampferMJRifaiNNovel risk factors for systemic atherosclerosis: a comparison of C-reactive protein, fibrinogen, homocysteine, lipoprotein(a), and standard cholesterol screening as predictors of peripheral arterial diseaseJAMA20012852481248511368701
- ShaiIRimmEBHankinsonSEMultivariate assessment of lipids parameters as predictors of coronary heart disease among postmenopausal women: potential implications for clinical guidelinesCirculation20041102824283015492318
- NamBHKannelWBD’AgostinoRBSearch for an optimal atherogenic lipid risk profile: from the Framingham StudyAm J Cardiol20069737237516442398
- Mounier-VehierCStephanDAboyansVGroupe vasculaire (SFC-Societe francaise de medecine vasculaires. The best of vascular medicine in 2006Arch Mal Coeur Vaiss2007100475517405565
- NatarajanSGlickHCriquiMHorowitzDLipsitzSRKinosianBCholesterol measures to identify and treat individuals at risk for coronary heart diseaseAm J Prev Med200325505712818310