Abstract
Atrial fibrillation (AF) is the most common form of cardiac arrhythmia and is associated with an increased risk of cardiovascular morbidity and mortality, especially due to ischemic stroke. The occurrence of AF leads to atrial electrical and structural remodeling. The renin-angiotensin system appears to play a role in the development of atrial arrhythmias by its involvement in both of these processes. Large-scale hypertension trials and heart failure trials have indicated the potential value of angiotensin II receptor blockers in the treatment of AF.
Introduction
Atrial fibrillation (AF) is the most common clinically significant cardiac arrhythmia. Overall, it affects >1% of the population and is common in the elderly, with a prevalence of almost 10% in individuals aged over 75 years.Citation1 Currently, approximately 2.3 million people in the United States are diagnosed with AF, and this number is expected to rise to 5.6 million by 2050.Citation2–Citation4
A 38-year follow-up review of data from the Framingham Study has indicated that men have a 1.5-fold greater risk of developing AF than women and that hypertension and diabetes are significant independent predictors of AF, after adjustment for age and other predisposing conditions. Hypertension was shown to be the most common, independent, and potentially modifiable risk factor for AF,Citation5,Citation6 primarily because of its high prevalence in the population.Citation5 The cardiac conditions that pose the greatest risk for development of AF include heart failure, myocardial infarction, and valvular heart disease (especially mitral valve disease). In addition, other cardiac conditions that have been associated with the occurrence of AF include myocarditis, hypertrophic cardiomyopathy, congenital heart disease, pericarditis, hypertensive cardiovascular disease, left ventricular hypertrophy, and coronary artery disease.Citation5,Citation7 Obesity was not associated with the incidence of AF in the review of Framingham data.Citation5 However, it has been proposed as a risk factor for the development of AF in relation to associated left atrial dilation.Citation8
The development of AF has been associated with a 1.5- to 1.9-fold greater mortality risk, after adjusting for preexisting cardiovascular conditions, in the original cohort of the Framingham Study.Citation9 Much of the morbidity and mortality associated with AF is due to thromboembolic complications resulting in ischemic stroke, especially in the elderly.Citation10 Ischemic stroke incidence among patients with nonvalvular AF averages 5% per year and is approximately 2 to 7 times greater than in individuals without AF.Citation11
The occurrence of AF leads to atrial electrical and structural remodeling, which both contribute to the maintenance and recurrence of the arrhythmia.Citation12–Citation18 Patients who initially present with paroxysmal AF often progress to longer, non–self-terminating bouts,Citation19 and enlarged atria are a major risk factor for its recurrence.Citation20,Citation21
Current treatment strategies for AF include the prevention of thromboembolism and either rate-control or rhythm-control strategies, with pharmacotherapy or left atrial ablation as first- or second-line therapy options, respectively.Citation8 These approaches may produce similar outcomes, but rate control may be preferable because agents used to maintain sinus rhythm can have proarrhythmic effects. However, both approaches have important limitations, including proarrhythmic and negative dromotropic effects, respectively.Citation8,Citation22,Citation23 In view of this, a preventive strategy may be a more attractive option.Citation7 The angiotensin-converting enzyme (ACE) inhibitors have been shown to reduce the incidence of AF postmyocardial infarction and in patients with left ventricular dysfunction.Citation24,Citation25 In addition, in recent years, large-scale hypertension trials (Losartan Intervention For Endpoint reduction in hypertension [LIFE] and Valsartan Antihypertensive Long-term Use Evaluation [VALUE]) and heart failure trials (Candesartan in Heart Failure – Assessment of Mortality and Morbidity [CHARM] and Valsartan Heart Failure Trial [Val-HeFT]) have indicated the potential value of angiotensin II receptor blockers (ARBs) in the treatment of AF.Citation26–Citation30 The aim of this review is to examine the mechanisms of action and clinical efficacy of ARBs in the prevention of AF.
Preventive mechanisms of ARBs in AF
The occurrence of uncomplicated AF leads mainly to electrical remodeling due to the high atrial rate (indicated by shortening of refractoriness), whereas structural remodeling develops when AF leads to a hemodynamic burden on the atria.Citation31 Cellular electrophysiological studies have indicated that marked reductions occur in the densities of the L-type voltage-gated calcium (Ca2+) current, I(Ca, L), the transient outward potassium (K+) current, I(TO), and the ultra-rapid delayed rectifier K+ current, I(Kur) in atrial myocytes from patients with chronic AF. Similar changes in currents have been noted in myocytes from a canine model of AF.Citation32 In both human and canine AF, the reduction in I (Ca, L) may explain the observed decrease in action potential duration and effective refractory period that are characteristic electro-physiological features of the remodeled atria.Citation32 Thus, it has been suggested that calcium overload and perturbations in calcium handling play prominent roles in AF-induced atrial remodeling in humans.Citation32
In addition, angiotensin II exerts its physiologic effects by activating AT1 and AT2 receptor subtypes. Goette et al noted that the occurrence of AF was associated with down regulation of AT1 and upregulation of AT2.Citation33 However, recently von Lewinski et al reported data that suggests that the major arrhythmic effects occur secondary to stimulation of the AT1 receptor and thus blockade of the AT1 receptor may be antiarrhythmic.Citation34
In contrast, structural remodeling is associated with fibrosis: this is characterized by increased deposition of connective tissue in the atria. The histological substrate of atrial biopsies in patients with lone AF has suggested that the probability of AF increases as the degree of fibrosis increases, and further electrophysiologic modification ultimately leads to self-perpetuation of AF.Citation31,Citation35–Citation39
The renin-angiotensin-aldosterone system (RAAS) appears to play a role in the development of arrhythmias by its involvement in both forms of remodeling. For example, angiotensin II has been shown to play a critical role in cardiac remodeling via the promotion of cardiac myocyte hypertrophy and cardiac fibroblast interstitial fibrotic changes associated with left ventricular hypertrophy, postmyocardial infarction remodeling, and congestive heart failure (CHF).Citation40 In particular, angiotensin II has been shown to mediate cardiac myocyte hypertrophy directly via induction of immediate early genes through a mitogen-activated protein kinase (MAPK)-dependent pathway. In addition, it has also been shown to mediate cardiac hypertrophy indirectly via stimulation of norepinephrine release from cardiac nerve endings and endothelin from endothelial cells and through multiple effects on cardiac fibroblasts.Citation40–Citation45
Electrical remodeling is brought about by the shortening of the atrial effective refractory period (AERP) and of the action potential duration.Citation46–Citation49 The inhibitory effects of an ARB (candesartan) and an ACE inhibitor (captopril) on atrial electrical remodeling induced by rapid pacing have been examined in a canine model of AF.Citation50 The AERP was measured before, during, and after rapid atrial pacing; infusions of saline, ARB, ACE inhibitor, or angiotensin II were initiated 30 minutes before rapid pacing and continued throughout the study. In the saline and angiotensin II groups, the AERP was significantly shortened during rapid atrial pacing and the rate adaptation of the AERP was lost. In contrast, in the ARB and ACE inhibitor groups, shortening of the AERP after rapid pacing was completely inhibited and the rate adaptation of the AERP was preserved, which indicated that endogenous angiotensin II may be involved in the mechanism of atrial electrical remodeling.Citation50
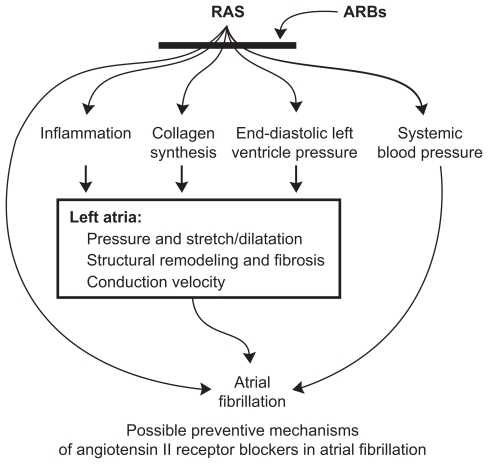
In addition to the reduction of blood pressure per se, there are a range of other potential mechanisms by which inhibition of the RAAS may reduce AF ().Citation51 For example, blockade of the RAAS may prevent left atrial dilatation, atrial fibrosis, dysfunction, and slowing of conduction velocityCitation44,Citation50,Citation52,Citation53 and, thus, may be particularly effective in patients with left ventricular dysfunction/heart failure.Citation54 Inhibition of the RAAS has also been shown to reduce inflammation and oxidative stress, and to modulate sympathetic nerve activity.Citation55 The use of agents that block the RAAS has been shown to increase the efficacy of electrical cardioversion of AF,Citation56–Citation59 and some studies have also indicated that blockade of the RAAS by ARBs may have direct antiarrhythmic properties.Citation60,Citation61 Thus, inhibition of the RAAS may lead to improvements in the management of AF.
Figure 1 Possible preventive mechanisms of ARBs in atrial fibrillation. Reproduced with permission from Aksnes T, Flaa A, Strand A, et al. Prevention of new-onset atrial fibrillation and its predictors with angiotensin II receptor blockers in the treatment of hypertension and heart failure. J Hypertens. 2007;25:15–23.Citation51 Copyright © wolters Kluwer Health.
Clinical trials with ARBs in AF
A range of clinical and experimental studies have shown that the use of ACE inhibitors or ARBs in CHF reduces the occurrence of AF and AF vulnerability via the reduction of atrial structural remodeling and fibrosis.Citation44,Citation53,Citation54,Citation62–Citation66
ARBs in patients with heart failure
A secondary analysis of the results of the CHARM program, which included 7601 patients with symptomatic CHF, has demonstrated that, in addition to significant reductions in cardiovascular deaths and hospital admissions for heart failure with reduced ejection fraction, the ARB candesartan significantly reduced the development of new AF compared with placebo. Moreover, the benefits of treatment with an ARB were accrued regardless of treatment at baseline (which included treatment with ACE inhibitors) and in a wide spectrum of patients with CHF, including those with preserved as well as reduced left ventricular systolic function ().Citation67,Citation68 In Val-HeFT, the occurrence of AF was associated with worse outcomes and was evaluated on the basis of adverse event reports in patients with heart failure treated with valsartan vs placebo on top of optimal heart failure therapy, which included ACE inhibitors and beta-blockers.Citation69,Citation70 Treatment with valsartan significantly reduced the combined endpoint of mortality and morbidity and improved clinical signs and symptoms in patients with heart failure, and also significantly reduced new-onset AF and reduced the relative risk of developing AF by 37% compared with placebo, when added to prescribed therapy. However, when ECG recordings from patients with sinus rhythm at enrolment were evaluated at 4, 12, and 24 months and at study end, the presence of at least 1 episode of AF showed no statistically significant difference between valsartan-treated patients and the placebo group (3.9% and 4.5%, respectively; P =0.15) (). Citation69,Citation70
Table 1 The effects of ARBs on AF and outcomes in clinical trials in patients with left ventricular dysfunction/congestive heart failure
ARBs in the treatment of AF after cardioversion
The efficacy of treatment with irbesartan in maintaining sinus rhythm after cardioversion has been evaluated in patients with persistent AF.Citation56 Patients were divided into 2 groups: group 1 was treated with amiodarone, group 2 with amiodarone plus irbesartan, and both groups underwent electrical cardioversion after 3 weeks of amiodarone administration. All patients started amiodarone after at least 3 weeks of anticoagulation to achieve an international normalized ratio greater than 2, and the primary endpoint of the study was the length of time to the first recurrence of AF. After 2 months of follow-up, the amiodarone plus irbesartan group had significantly fewer recurrences of AF (63.2%) than the amiodarone-only group (84.8%, P = 0.008), and had a greater probability of maintaining sinus rhythm (79.5% vs 55.9%, P = 0.007).Citation56 There was also a trend toward a lower number of shocks and lower electrical threshold, but this did not reach statistical significance.Citation56 Furthermore, in a subsequent study, the combination of irbesartan plus amiodarone decreased the rate of AF recurrence in a dose-dependent manner in lone AF patients.Citation57
ARBs in the prevention of new AF
In the Study on Cognition and Prognosis in the Elderly (SCOPE), there was a marked reduction in nonfatal stroke compared with placebo in elderly patients with hypertension who received treatment with an ARB, which may have been due to a reduction in AF ().Citation71
Table 2 Studies of the effectiveness of ARBs in the prevention of AF (new onset and recurrent)
Similarly, the results of the LIFE study indicated that ARB-based treatment produced a 25% reduction in fatal and nonfatal stroke compared with atenolol-based treatment in hypertensive patients with left ventricular hypertrophy. This was attributable in part to a 45% lower rate of stroke (24.1 vs 46.5 strokes per 1000 patient-years of follow-up) on ARB treatment in patients with a history of AF,Citation29 but may have also been a reflection of benefits from a reduced incidence of new-onset AF. In a subsequent subanalysis of ECG data from patients without AF by history at baseline, new-onset AF occurred in 150 patients randomized to losartan vs 221 to atenolol (6.8 vs 10.1 per 1000 person-years; relative risk [RR] 0.67, P < 0.001) despite similar levels of blood pressure reduction ().Citation28 Patients who received losartan tended to stay in sinus rhythm longer (mean, 1809 vs 1709 days from baseline, P =0.057) than those who received atenolol. Patients with new-onset AF had 2-, 3-, and 5-fold increased rates, respectively, of cardiovascular events, stroke, and hospitalization for heart failure, but there were fewer composite endpoints and strokes in patients who developed new-onset AF in the losartan arm compared to the atenolol treatment arm of the study.Citation28
In the VALUE trial, new-onset AF was a secondary prespecified endpoint and ECG recordings were obtained every year and centrally analyzed. During the study, the incidence of at least 1 documented occurrence of new-onset AF was significantly lower in the valsartan treatment group (3.7%) than in the amlodipine treatment group (4.3%, odds ratio 0.84) (). The incidence of persistent AF was also significantly lower with valsartan than with amlodipine (odds ratio 0.68, ), and the effects of valsartan on the incidence of AF remained significant even when potential confounding covariates (age, history of coronary artery disease, left ventricular hypertrophy) were taken into account.Citation27,Citation30
In addition, the noninferiority of ARBs compared to ACE inhibitors in the prevention of new-onset AF was demonstrated in the ONTARGET study (Ongoing Telmisartan Alone and in Combination With Ramipril Global Endpoint Trial) in patients with vascular disease or high-risk diabetes ().Citation72 In this study, which compared the effectiveness of telmisartan and ramipril in reducing cardiovascular death, myocardial infarction, stroke, and hospitalization for heart failure in patients at risk, the diagnosis of new-onset AF was a secondary endpoint.Citation72 Telmisartan treatment produced a greater reduction in blood pressure than ramipril and, after a median follow-up of 56 months, the primary outcome of death from cardiovascular causes, myocardial infarction, stroke, or hospitalization for heart failure had occurred in 1412 patients in the ramipril group (16.5%) vs 1423 patients in the telmisartan group (16.7%, RR 1.01). However, the combination of the 2 drugs was associated with a greater frequency of adverse events without an increase in benefit.Citation72
ARBs in the prevention of recurrent AF
Patients with hypertension and type 2 diabetes have an elevated risk of cardiovascular events and typically require combination antihypertensive therapy to achieve goal blood pressure levels. In view of this, Fogari et al Citation73 compared the effectiveness of valsartan + amlodipine and atenolol + amlodipine combinations on the prevention of AF recurrence in hypertensive patients with well-controlled type 2 diabetes in sinus rhythm who had at least 2 ECG-documented episodes of AF in the previous 6 months. Significantly fewer patients who were followed up for 1 year had recurrent AF with an ARB in addition to antiarrhythmic agents than with atenolol ().Citation73 Overall, despite similar levels of blood pressure reduction, the valsartan + amlodipine combination was more effective in preventing AF in patients treated with amiodarone or propafenone.Citation73 In addition, ARB therapy with valsartan led to significantly fewer recurrences of AF after 12 weeks of treatment than amlodipine, and significantly less recurrence than both amlodipine and ramipril after 1 year in patients with mild hypertension and a history of AF ().Citation74 Although blood pressure lowering could be a beneficial mechanism of action for the reduction of AF with both types of RAAS inhibitors, there were no statistically significant differences in blood pressure between the 3 treatment groups in this study. This suggested that both ARBs and ACE inhibitors may exert an antiarrhythmic effect beyond their effects on blood pressure.Citation74 However, no statistically significant reduction in the recurrence of AF was noted with valsartan treatment compared with placebo in the recent GISSI-AF study (Gruppo Italiano per lo Studio della Sopravvivenza nell’Infarto Miocardico: Use of Valsartan and Angiotensin II AT1-Receptor Blocker in the Prevention of Atrial Fibrillation Recurrence).Citation75 This may have been due to issues relating to the study design, broad selection criteria, and/or the patients’ relatively low-risk clinical conditions (and possible consequent low level of RAAS activation), and optimized background therapy. Moreover, the use of candesartan had no influence on echocardiographic variables or on the recurrence rate of AF after cardioversion in the 6-month Candesartan in the Prevention of Relapsing Atrial Fibrillation (CAPRAF) study.Citation76,Citation77
Ongoing trials of ARBs in AF
It is hoped that a range of ongoing and planned future studies will help to clarify the possible beneficial effects of treatment with ARBs in terms of prevention of AF complications and prevention of AF recurrence (). The Atrial Fibrillation Clopidogrel Trial with Irbesartan for Prevention of Vascular Events (ACTIVE I) trial will randomize 9000 patients with a history of AF to receive irbesartan or placebo with a planned mean follow-up of 3 years. ACTIVE I is part of the ACTIVE trial program investigating the effect of irbesartan on the occurrence of stroke, myocardial infarction or vascular death, hospitalization for heart failure (primary endpoints) and recurrence of AF, development of cardiac structural remodeling, microalbuminuria, cognitive function, and quality of life (secondary endpoints).Citation78 In addition, the Angiotensin II Antagonist in Paroxysmal Atrial Fibrillation (ANTIPAF) trial will compare the effect of olmesartan and placebo in patients with paroxysmal AF,Citation79 and the aim of the planned I-PACE trial is to investigate the effects of irbesartan in hypertensive patients with pacemakers who have recurrent atrial high-rate episodes (Irbesartan for the Prevention of Atrial Arrhythmias and Cardiac Electrical Remodeling in Patients With Hypertension and Permanent Pacemakers).Citation80
Table 3 Summary of ongoing prospective trials of ARBs in patients with AF
Conclusions and clinical recommendations
The prevention of AF is particularly challenging because of its high incidence.Citation1,Citation3,Citation81 Because ARBs block the actions of angiotensin II, it seems likely that they interfere with structural and electrical remodeling and consequently provide benefits in terms of prevention of new-onset AF and recurrence of AF. So far, the body of evidence supports that ARBs may be useful in combination with other antiarrhythmic agents and not as sole antiarrhythmic therapy in suppressing AF recurrences. However, while the possibility of hemodynamic benefits and direct antiarrhythmic effects cannot be excluded, it is hoped that the results of ongoing prospective studies, such as ACTIVE I and I-PACE, will clarify the benefits of ARB treatment in relation to AF. Although valsartan was ineffective in suppressing AF in GISSI-AF, this study and the results of ACTIVE I may be limited by the high percentage of patients who had background ACE inhibitor therapy. The results of ACTIVE I may support the use of ARBs related to meaningful endpoints and not surrogates such as AF recurrence. Although it is not currently possible to specifically recommend the use of ARBs for prevention of AF in routine clinical practice, ARBs are well tolerated and may be considered for use in patients with AF and coexisting clinical conditions such as hypertension, coronary heart disease, CHF, and type 2 diabetes.
Acknowledgments and financial disclosure
This study was supported by the Bristol-Myers Squibb/Sanofi-Synthelabo Partnership. All authors contributed to the interpretation of data, its development, and the approval of the final manuscript. The authors received no financial support or other compensation related to its development. The authors thank Pam Milner and Stephanie Eide who provided editorial services on behalf of Bristol-Myers Squibb and sanofi-aventis.
References
- PhillipsSJWhisnantJPO’FallonWMFryeRLPrevalence of cardiovascular disease and diabetes mellitus in residents of Rochester, MinnesotaMayo Clin Proc19906533443592248634
- GoASHylekEMPhillipsKAPrevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) StudyJAMA2001285182370237511343485
- KannelWBBenjaminEJStatus of the epidemiology of atrial fibrillationMed Clin North Am20089211740ix18060995
- MiyasakaYBarnesMEGershBJSecular trends in incidence of atrial fibrillation in Olmsted County, Minnesota, 1980 to 2000, and implications on the projections for future prevalenceCirculation2006114211912516818816
- KannelWBWolfPABenjaminEJLevyDPrevalence, incidence, prognosis, and predisposing conditions for atrial fibrillation: population-based estimatesAm J Cardiol1998828A2N9N
- PsatyBMManolioTAKullerLHIncidence of and risk factors for atrial fibrillation in older adultsCirculation1997967245524619337224
- NovoGGuttillaDFazioGCooperDNovoSThe role of the renin-angiotensin system in atrial fibrillation and the therapeutic effects of ACE-Is and ARBSBr J Clin Pharmacol200866334535118782141
- FusterVRydenLECannomDSACC/AHA/ESC 2006 guidelines for the management of patients with atrial fibrillation-executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Revise the 2001 Guidelines for the Management of Patients with Atrial Fibrillation)Eur Heart J200627161979203016885201
- BenjaminEJWolfPAD’AgostinoRBSilbershatzHKannelWBLevyDImpact of atrial fibrillation on the risk of death: the Framingham Heart StudyCirculation199898109469529737513
- HartRGHalperinJLAtrial fibrillation and stroke: concepts and controversiesStroke200132380380811239205
- WolfPAAbbottRDKannelWBAtrial fibrillation as an independent risk factor for stroke: the Framingham StudyStroke19912289839881866765
- AllessieMAAtrial electrophysiologic remodeling: another vicious circle?J Cardiovasc Electrophysiol1998912137813939869538
- AusmaJvan der VeldenHMLendersMHReverse structural and gap-junctional remodeling after prolonged atrial fibrillation in the goatCirculation2003107152051205812681996
- HeidbuchelHA paradigm shift in treatment for atrial fibrillation: from electrical to structural therapy?Eur Heart J200324232077207814643265
- HobbsWJFynnSToddDMWolfsonPGallowayMGarrattCJReversal of atrial electrical remodeling after cardioversion of persistent atrial fibrillation in humansCirculation2000101101145115110715261
- NattelSShiroshita-TakeshitaACardinSPelletierPMechanisms of atrial remodeling and clinical relevanceCurr Opin Cardiol2005201212515596955
- SanfilippoAJAbascalVMSheehanMAtrial enlargement as a consequence of atrial fibrillation. A prospective echocardiographic studyCirculation19908237927972144217
- ThijssenVLAusmaJLiuGSAllessieMAvan EysGJBorgersMStructural changes of atrial myocardium during chronic atrial fibrillationCardiovasc Pathol200091172810739903
- AllessieMABoydenPACammAJPathophysiology and prevention of atrial fibrillationCirculation2001103576977711156892
- MattioliAVVivoliDBastiaEDoppler echocardiographic parameters predictive of recurrence of atrial fibrillation of different etiologic originsJ Ultrasound Med199716106956989323676
- VerdecchiaPReboldiGGattobigioRAtrial fibrillation in hypertension: predictors and outcomeHypertension200341221822312574085
- FreudenbergerRSWilsonACKostisJBComparison of rate versus rhythm control for atrial fibrillation in patients with left ventricular dysfunction (from the AFFIRM Study)Am J Cardiol2007100224725217631079
- HohnloserSHKuckKHLilienthalJRhythm or rate control in atrial fibrillation – Pharmacological Intervention in Atrial Fibrillation (PIAF): a randomised trialLancet200035692441789179411117910
- PedersenODBaggerHKoberLTorp-PedersenCTrandolapril reduces the incidence of atrial fibrillation after acute myocardial infarction in patients with left ventricular dysfunctionCirculation1999100437638010421597
- VermesETardifJCBourassaMGEnalapril decreases the incidence of atrial fibrillation in patients with left ventricular dysfunction: insight from the Studies Of Left Ventricular Dysfunction (SOLVD) trialsCirculation2003107232926293112771010
- MaggioniAPLatiniRCarsonPEValsartan reduces the incidence of atrial fibrillation in patients with heart failure: results from the Valsartan Heart Failure Trial (Val-HeFT)Am Heart J2005149354855715864246
- SchmiederREKjeldsenSEJuliusSMcInnesGTZanchettiAHuaTAReduced incidence of new-onset atrial fibrillation with angiotensin II receptor blockade: the VALUE trialJ Hypertens200826340341118300848
- WachtellKLehtoMGerdtsEAngiotensin II receptor blockade reduces new-onset atrial fibrillation and subsequent stroke compared to atenolol: the Losartan Intervention For End Point Reduction in Hypertension (LIFE) studyJ Am Coll Cardiol200545571271915734615
- WachtellKHornestamBLehtoMCardiovascular morbidity and mortality in hypertensive patients with a history of atrial fibrillation: The Losartan Intervention For End Point Reduction in Hypertension (LIFE) studyJ Am Coll Cardiol200545570571115734614
- WeberMAJuliusSKjeldsenSEBlood pressure dependent and independent effects of antihypertensive treatment on clinical events in the VALUE TrialLancet200436394262049205115207957
- SchoonderwoerdBAVan GelderICVan VeldhuisenDJVan Den BergMPCrijnsHJElectrical and structural remodeling: role in the genesis and maintenance of atrial fibrillationProg Cardiovasc Dis200548315316816271942
- Van WagonerDRNerbonneJMMolecular basis of electrical remodeling in atrial fibrillationJ Mol Cell Cardiol20003261101111710888261
- GoetteAArndtMRockenCRegulation of angiotensin II receptor subtypes during atrial fibrillation in humansCirculation2000101232678268110851203
- von LewinskiDKockskamperJRubertusSUDirect pro-arrhythmogenic effects of angiotensin II can be suppressed by AT1 receptor blockade in human atrial myocardiumEur J Heart Fail200810121172117618993115
- ChaYMRedfieldMMShenWKGershBJAtrial fibrillation and ventricular dysfunction: a vicious electromechanical cycleCirculation2004109232839284315197156
- FrustaciAChimentiCBellocciFMorganteERussoMAMaseriAHistological substrate of atrial biopsies in patients with lone atrial fibrillationCirculation1997964118011849286947
- Van GelderICHemelsMEThe progressive nature of atrial fibrillation: a rationale for early restoration and maintenance of sinus rhythmEuropace200681194394916973685
- VerheuleSWilsonEEverettTShanbhagSGoldenCOlginJAlterations in atrial electrophysiology and tissue structure in a canine model of chronic atrial dilatation due to mitral regurgitationCirculation2003107202615262212732604
- WijffelsMCKirchhofCJDorlandRAllessieMAAtrial fibrillation begets atrial fibrillation. A study in awake chronically instrumented goatsCirculation1995927195419687671380
- SchneeJMHsuehWAAngiotensin II, adhesion, and cardiac fibrosisCardiovasc Res200046226426810773230
- BrillaCGZhouGMatsubaraLWeberKTCollagen metabolism in cultured adult rat cardiac fibroblasts: response to angiotensin II and aldosteroneJ Mol Cell Cardiol19942678098207966349
- GoetteAStaackTRockenCIncreased expression of extracellular signal-regulated kinase and angiotensin-converting enzyme in human atria during atrial fibrillationJ Am Coll Cardiol20003561669167710807475
- LiDFarehSLeungTKNattelSPromotion of atrial fibrillation by heart failure in dogs: atrial remodeling of a different sortCirculation19991001879510393686
- LiDShinagawaKPangLEffects of angiotensin-converting enzyme inhibition on the development of the atrial fibrillation substrate in dogs with ventricular tachypacing-induced congestive heart failureCirculation2001104212608261411714658
- SadoshimaJIzumoSMolecular characterization of angiotensin II – induced hypertrophy of cardiac myocytes and hyperplasia of cardiac fibroblasts. Critical role of the AT1 receptor subtypeCirc Res19937334134238348686
- BoschRFZengXGrammerJBPopovicKMewisCKuhlkampVIonic mechanisms of electrical remodeling in human atrial fibrillationCardiovasc Res199944112113110615396
- BoschRFNattelSCellular electrophysiology of atrial fibrillationCardiovasc Res200254225926912062331
- YuWCLeeSHTaiCTReversal of atrial electrical remodeling following cardioversion of long-standing atrial fibrillation in manCardiovasc Res199942247047610533582
- YueLFengJGaspoRLiGRWangZNattelSIonic remodeling underlying action potential changes in a canine model of atrial fibrillationCirc Res19978145125259314832
- NakashimaHKumagaiKUrataHGondoNIdeishiMArakawaKAngiotensin II antagonist prevents electrical remodeling in atrial fibrillationCirculation2000101222612261710840013
- AksnesTAFlaaAStrandAKjeldsenSEPrevention of new-onset atrial fibrillation and its predictors with angiotensin II-receptor blockers in the treatment of hypertension and heart failureJ Hypertens2007251152317143167
- ShiYDucharmeALiDGaspoRNattelSTardifJCRemodeling of atrial dimensions and emptying function in canine models of atrial fibrillationCardiovasc Res200152221722511684069
- ShiYLiDTardifJCNattelSEnalapril effects on atrial remodeling and atrial fibrillation in experimental congestive heart failureCardiovasc Res200254245646112062350
- HealeyJSBaranchukACrystalEPrevention of atrial fibrillation with angiotensin-converting enzyme inhibitors and angiotensin receptor blockers: a meta-analysisJ Am Coll Cardiol200545111832183915936615
- MurrayKTMaceLCYangZNonantiarrhythmic drug therapy for atrial fibrillationHeart Rhythm200743 SupplS88S9017336893
- MadridAHBuenoMGRebolloJMUse of irbesartan to maintain sinus rhythm in patients with long-lasting persistent atrial fibrillation: a prospective and randomized studyCirculation2002106333133612119249
- MadridAHMarinIMCervantesCEPrevention of recurrences in patients with lone atrial fibrillation. The dose-dependent effect of angiotensin II receptor blockersJ Renin Angiotensin Aldosterone Syst20045311412015526246
- Van NoordTCrijnsHJVan Den BergMPVan VeldhuisenDJVan GelderICPretreatment with ACE inhibitors improves acute outcome of electrical cardioversion in patients with persistent atrial fibrillationBMC Cardiovasc Disord200551315667649
- ZamanAGKearneyMTSchecterCWorthleySGNolanJAngiotensin-converting enzyme inhibitors as adjunctive therapy in patients with persistent atrial fibrillationAm Heart J2004147582382715131537
- CaballeroRDelponEValenzuelaCLongobardoMTamargoJLosartan and its metabolite E3174 modify cardiac delayed rectifier K(+) currentsCirculation2000101101199120510715269
- MorenoICaballeroRGonzalezTEffects of irbesartan on cloned potassium channels involved in human cardiac repolarizationJ Pharmacol Exp Ther2003304286287312538844
- BoldtASchollAGarbadeJACE-inhibitor treatment attenuates atrial structural remodeling in patients with lone chronic atrial fibrillationBasic Res Cardiol2006101326126716382287
- KumagaiKNakashimaHUrataHGondoNArakawaKSakuKEffects of angiotensin II type 1 receptor antagonist on electrical and structural remodeling in atrial fibrillationJ Am Coll Cardiol200341122197220412821247
- LiYLiWYangBEffects of Cilazapril on atrial electrical, structural and functional remodeling in atrial fibrillation dogsJ Electrocardiol200740110010617067622
- OkazakiHMinaminoTTsukamotoOAngiotensin II type 1 receptor blocker prevents atrial structural remodeling in rats with hypertension induced by chronic nitric oxide inhibitionHypertens Res200629427728416778335
- SakabeMFujikiANishidaKEnalapril prevents perpetuation of atrial fibrillation by suppressing atrial fibrosis and over-expression of connexin 43 in a canine model of atrial pacing-induced left ventricular dysfunctionJ Cardiovasc Pharmacol200443685185915167279
- DucharmeASwedbergKPfefferMAPrevention of atrial fibrillation in patients with symptomatic chronic heart failure by candesartan in the Candesartan in Heart failure: Assessment of Reduction in Mortality and morbidity (CHARM) programAm Heart J20061521869216838426
- PfefferMASwedbergKGrangerCBEffects of candesartan on mortality and morbidity in patients with chronic heart failure: the CHARM-Overall programmeLancet2003362938675976613678868
- CohnJNTognoniGA randomized trial of the angiotensin-receptor blocker valsartan in chronic heart failureN Engl J Med2001345231667167511759645
- MaggioniAPLatiniRCarsonPEValsartan reduces the incidence of atrial fibrillation in patients with heart failure: results from the Valsartan Heart Failure Trial (Val-HeFT)Am Heart J2005149354855715864246
- LithellHHanssonLSkoogIThe Study of Cognition and Prognosis in the Elderley (SCOPE): principal results of a randomized double-blind intervention trialJ Hypertens200321587588612714861
- ONTARGET InvestigatorsYusufSTeoKKTelmisartan, ramipril, or both in patients at high risk for vascular eventsN Engl J Med2008358151547155918378520
- FogariRZoppiAMugelliniAComparative evaluation of effect of valsartan/amlodipine and atenolol/amlodipine combinations on atrial fibrillation recurrence in hypertensive patients with type 2 diabetes mellitusJ Cardiovasc Pharmacol200851321722218356684
- FogariRDerosaGFerrariIEffect of valsartan and ramipril on atrial fibrillation recurrence and P-wave dispersion in hypertensive patients with recurrent symptomatic lone atrial fibrillationAm J Hypertens20082191034103918566593
- GISSI-AF InvestigatorsDisertoriMatiniRValsartan for prevention of recurrent atrial fibrillationN Engl J Med2009360161606161719369667
- GrundvoldITveitASmithPSeljeflotIAbdelnoorMArnesenHThe predictive value of transthoracic echocardiographic variables for sinus rhythm maintenance after electrical cardioversion of atrial fibrillation. Results from the CAPRAF study, a prospective, randomized, placebo-controlled studyCardiology20081111303518239389
- TveitAGrundvoldIOlufsenMCandesartan in the prevention of relapsing atrial fibrillationInt J Cardiol20071201859117113170
- Active Steering Committee, ACTIVE InvestigatorsConnollySRationale and design of ACTIVE: the atrial fibrillation clopidogrel trial with irbesartan for prevention of vascular eventsAm Heart J200615161187119316781218
- GoetteABreithardtGFetschTAngiotensin II antagonist in paroxysmal atrial fibrillation (ANTIPAF) trial: rationale and study designClin Drug Investig20072710697705
- Irbesartan for the Prevention of Atrial Arrhythmias and Cardiac Electrical Remodeling in Patients With Hypertension and Permanent Pacemakers (NCT00225667) [ClinicalTrials.gov Web site]. http://www.clinicaltrials.gov/ct2/show/NCT00225667?term=NCT00225667&rank=1Accessed June 28, 2009
- GoASHylekEMPhillipsKAPrevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) StudyJAMA2001285182370237511343485