Abstract
Despite significant improvement in therapy and management, heart failure remains a worrisome disease state that is especially problematic in special populations. African Americans suffer a disproportionately higher prevalence of heart failure when compared to other populations. It has been recently demonstrated that vasodilator therapy using the combination of isosorbide dinitrate (ISDN) and hydralazine (HYD) as an adjunct to background evidence-based therapy appears to display the strongest signal of benefit in reducing mortality and morbidity in the African American population. Through review of the retrospective and more recent prospective data, we will focus on the benefit of ISDN-HYD as adjunctive therapy for use in African Americans with systolic heart failure on concomitant appropriate evidence based therapy. This review also closely examines some of the potential contributions to endothelial dysfunction in African Americans, and the relationship of vascular homeostasis and nitric oxide. The role of oxidative stress in left ventricular dysfunction will also be explored as a reduction of oxidative stress offers particular promise in the management of heart failure. Although neurohormonal blockade has been responsible for notable event reductions in patients with systolic heart failure, the addition of ISDN-HYD, vasodilator therapy that enhances nitric oxide and reduces oxidative stress, further improves quality of life and survival in African American patients with heart failure. These findings strongly imply that nitric oxide enhancement and/or oxidative stress reduction may be important new therapeutic directions in the management of heart failure.
Despite significant advances in therapy, heart failure remains a disease state associated with significant morbidity and mortality. At the age of 40, the estimated lifetime risk of developing heart failure is as high as 40%, depending on the presence of uncontrolled hypertension or other morbid cardiovascular conditions (CitationAmerican Heart Association 2006). In response to this disease burden, a number of clinical trial efforts have yielded remarkable improvements in our understanding and treatment of systolic heart failure (CitationYancy 2005). The deleterious effects of an activated neurohoromonal system in response to left ventricular dysfunction have proven to be responsible for disease progression, and treatment strategies to counteract these actions, eg, angiotensin converting enzyme-inhibitors (ACE-I) and beta blockers, are now associated with notable reductions in systolic heart failure hospitalizations and improvement in overall survival (CitationKonstam et al 1992; CitationBristow 2000; CitationHunt et al 2005). However, a fundamental question has been raised—do all patient populations benefit similarly from the advances noted in systolic heart failure management?
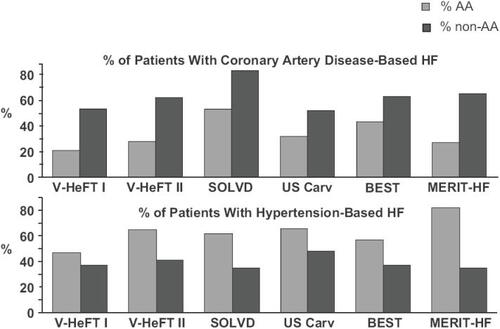
African Americans continue to suffer a disproportionately higher prevalence of heart failure when compared to Caucasians (CitationDries et al 2001). Systolic heart failure in African Americans is less likely to correlate with a burden of coronary artery disease, but is more likely to be associated with younger age and the presence of hypertension (). However, the exact mechanism and progression of hypertensive heart disease to systolic dysfunction is not well understood. Effects of drug therapy in African Americans with heart failure are also difficult to interpret. A major obstacle prohibiting the evaluation of heart failure therapy in African Americans is the inadequate representation of African Americans in clinical trials. Data pertaining to drug effect and outcome of heart failure in African Americans are almost always based on post hoc analyses, which fail to have sufficient power to detect meaningful endpoints within this group. Therefore, the evidence for most systolic heart failure drug therapy in African Americans is speculative at best. Even so, treatment of heart failure in African Americans should follow evidence based guidelines, as there is no evidence to date to suggest that such a management plan is harmful for this group (CitationHunt et al 2005; CitationYancy 2005).
Figure 1 Etiology of congestive heart failure in African Americans. Adapted from CitationCohn et al 1986; CitationCohn et al 1991; CitationThe SOLVD Investigators 1991; CitationPacker et al 1996; CitationMERIT-HF Study Group 1999;The Beta-Blocker Evaluation of Survival Trial Investigators 2001.
Of all of the proven treatment regimens that have been evaluated for evidence of efficacy in African Americans with systolic heart failure, the vasodilators have emerged with the strongest signal of benefit. Through post hoc analyses of the earlier vasodilating trials, a “hypothesis-generating” concept has led to a landmark trial, the African American Heart Failure Trial [A-HeFT], which demonstrated the striking benefit of ISDN-HYD as combination therapy, in African Americans with systolic heart failure (CitationTaylor et al 2004). It is the purpose of this review article to develop the background, rationale and scientific premise for these notable benefits of ISDNHYD as adjunctive therapy for heart failure.
Vasodilator therapy in heart failure
Prior to 1980, the effects of vasodilator therapy on heart failure were not well understood. The Veterans Administration Cooperation Study (V-HeFT I) was the first double blind randomized controlled trial to examine this interaction (CitationCohn et al 1986). The initial hypothesis evolved around the possibility that peripheral vasoconstriction was responsible for hemodynamic compromise and further progression of symptoms in heart failure patients (CitationCohn et al 1986). The choice of ISDNHYD was based on the ability of this combination to reduce preload (venodilation) and afterload (arterial dilation), similar to the effects seen with nitroprusside (Pierpont et al 1978). The V-HeFT I study enrolled 642 men, of which 180 or 28% were African American. All participants received either ISDN-HYD combination (n = 186), prazosin (n = 183), or placebo (n = 273). The average dose of ISDN-HYD combination was 136 mg and 270 mg respectively. Approximately 55% of the ISDN-HYD group achieved the maximum dose (160 mg of ISDN and 300 mg of HYD). The mean period of follow-up was 2.3 years. At one year, there was a 38% reduction in mortality for the patients receiving ISDN-HYD, compared to placebo (12.1% vs 19.5% respectively). At the end of the pre-specified time point of two years, there was a 25% reduction in mortality (25.6% for the ISDN-HYD group compared to 34.3% for the placebo group, p < 0.028). The prazosin group had a mortality rate that was similar to the placebo group, although there was greater blood pressure reduction within the prazosin group when compared to the ISDN-HYD group. At the end of the trial the overall cumulative mortality reduction for the ISDN-HYD group was of borderline statistical significance (p ~ 0.05). Despite the marginal statistical signal, this trial demonstrated clinical significance and was the first trial to demonstrate improved survival with drug therapy for any heart failure population.
After the results of V-HeFT I, the effects of the ISDN-HYD combination therapy were further evaluated against an ACE-I, enalapril, in V-HeFT II (CitationCohn et al 1991). Use of enalapril in severe heart failure had previously demonstrated reduction in mortality when compared to placebo in the Cooperative North Scandinavian Enalapril Survival Study (CitationThe CONSENSUS Trial Study Group 1987) in class IV heart failure. The V-HeFT II trial enrolled 804 patients, and compared the use of ISDNHYD (maximum dose 160 mg and 300 mg repectively, divided into four daily doses) to enalapril (maximum dose 20 mg daily). At the pre-specified endpoint of two years, enalapril reduced mortality 28% more than the ISDN-HYD therapy. Although death from worsening heart failure did not differ between the groups, there was a significant reduction in sudden cardiac death with enalapril compared to the ISDN-HYD group. The results from this study suggested that enalapril was superior to ISDN-HYD therapy for improving survival in patients with mild to moderate heart failure.
Racial differences in response to vasodilator therapy: lessons from V-HeFT I and II
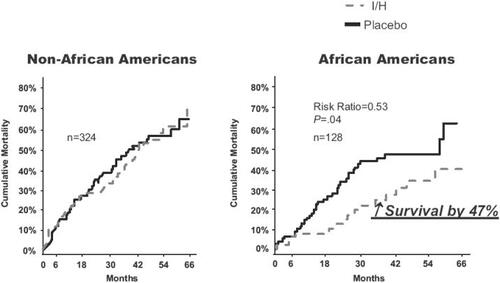
As the studies of vasodilator therapies in heart failure developed, there appeared to be a specific signal of differential outcome between African Americans and Caucasians. Retrospective analysis from the Studies of Left Ventricular Dysfunction (SOLVD) Prevention and Treatment trials demonstrated a significantly higher risk of death from all causes in African Americans when compared with Caucasians (CitationDries et al 1999). Further inspection of specific drug therapies began to suggest differential effects between races as well. A post hoc analysis of V-HeFT I and II revealed a striking difference in outcomes in the African Americans who were administered ISDN-HYD therapy (CitationCarson et al 1999). In V-HeFT I, there was a 47% reduction in mortality for African Americans receiving ISDN-HYD combination when compared with the African American patients in the placebo group (9.7% vs 17.3% respectively, p = 0.04) (). When the use of ISDN-HYD was compared to enalapril in African American patients from V-HeFT II, there was no significant difference in mortality (12.9% vs 12.8%, p = NS). However, the Caucasian patients had a 26% reduction in mortality with the use of enalapril when compared with the Caucasian patients receiving ISDN-HYD therapy (11% vs 14.9% respectively, p = 0.02). Results of this analysis suggested that African Americans patients with heart failure had a heightened response to ISDN-HYD therapy, similar to that seen with the use of ACE-inhibitors. Further evaluation of the SOLVD study using case matched Caucasians and African Americans demonstrated a similar efficacy of enalapril on mortality but a differential effect on hospitalizations (CitationExner et al 2001). Taken together, these findings suggested that benefit from ACE-I therapy in African Americans was evident and thus this therapy is strongly recommended by current guidelines for all persons with heart failure (CitationHunt et al 2005).
Figure 2 V-HeFT 1. survival benefit in subgroup analysis. Adapted from CitationCarson et al (1999).
The reasons for these findings of differential response in V-HeFT I and II were not well understood at the time. There were several baseline differences in the African American patients when compared with their Caucasian counterparts. African American patients were younger, had less CAD, and had a significantly higher incidence of hypertension (V-HeFT II only). Interestingly, the Caucasian patients had higher plasma norepinephrine when compared with the African American patients, although there was no difference in renin activity between groups. Patients with uncontrolled hypertension or hypertension requiring more than diuretic therapy were excluded from both V-HeFT I and II. This exclusion undoubtedly eliminated a population in which persistent hypertension may have been the nidus for systolic impairment.
The effects of nitric oxide (NO) and its relationship to endothelial function in African Americans became a key area of interest. Previous studies evaluating the response of innate vasodilatory stimuli on forearm arterial resistance suggested differential effects between African Americans and Caucasians (Hinderliter et al 1996; CitationCardillo et al 1998; CitationKahn and Duffy 2002). Cardillo et al evaluated the racial differences in NO mediated vasodilation on forearm arterial resistance in relation to mental stress on normal patients. Mental stress, in the form of serial seven subtractions, was used as a standard measure to increase forearm blood flow. The increase in forearm blood flow was easily demonstrated in the Caucasian subjects but not in the African American subjects. Use of a NO synthesis (NOS) inhibitor NG-monomethyl-L-arginine (L-NMMA) infusion significantly reduced forearm blood flow in Caucasian patients, where the forearm blood flow in African American patients was unaffected. Results of this study suggested impaired NO-related vasodilatory action of endothelial and smooth muscle cell function in African Americans- a finding that implicates endothelial dysfunction in this group of patients.
More recent data evaluating the use of methacholine, a parasympathetic agonist, in hypertensive patients also demonstrated less vasodilatory response of forearm blood flow in African American patients compared with Caucasians (CitationKahn and Duffy 2002). These results echoed the previous findings suggesting impaired endothelial vasomotor function in African American patients. Even in normal individuals, there are provocative data to suggest reduction in endothelium-derived NO bioavailability in African Americans, when compared with Caucasians (CitationKalinowski 2004). Moreover, these data are accompanied by findings suggestive of increased oxidative stress, ie, increased production of superoxide and peroxynitrite, further increasing the likelihood of endothelial impairment in African Americans.
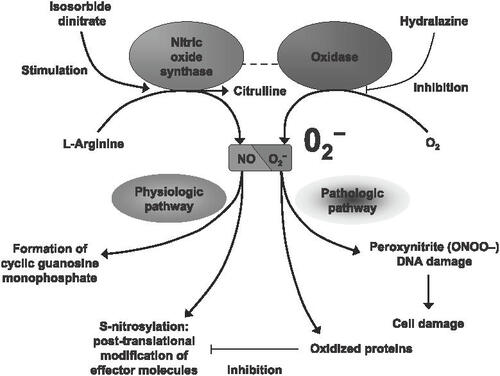
Extrapolation of these findings may implicate the effects of reduced NO bioavailability on myocyte function. Nitric oxide is generated by NOS, neuronal NOS (nNOS or NOS1), inducible NOS (iNOS or NOS2), and endothelial NOS (eNOS or NOS3), which convert L-arginine to L-citrulline in the presence of molecular oxygen, nicotinamide-adeninine dinucleotide phosphate (NADPH), calmodulin, and other cofactors (CitationPrabhu 2004, p 1155). Dysfunctional endothelium hinders the production and bioavailability of NO, which increases the production of reactive oxygen species and oxidative stress. Reduced concentrations of NO cosubstrates, such as L-arginine, promote inactivation of eNOS and 1 electron reduction of O2 to O2-, also known as superoxide. Increased production of O2-, further increases oxidative stress by reacting with available NO to form peroxynitrite [ONOO–] (CitationHare 2004; CitationMalinski 2005). Production of peroxynitrite is associated with proapoptotic effects, possibly contributing to increased ventricular remodeling and impairment of systolic function. Nitric oxide is also responsible for antihypertrophic effects, primarily mediated by cGMPdependent protein kinases (CitationWollert and Drexler 2002). Overexpression of NO synthase 3 (NOS3) has been demonstrated to reduce myocyte hypertrophy after myocardial infarction in animal models, suggesting greater antihypertrophic effects with increased production of physiological levels of NO (CitationJanssens et al 2004). Total eNOS protein appears to be increased in African Americans, but there is lack of biologically active NO production (CitationMalinski 2005). It is reasonable to presume that reduced NO bioavailability may alter myocyte function and increase cardiac hypertrophy. However, these concepts are controversial, as higher or “supernormal” levels of NO (perhaps related to iNOS activation), appear to induce caspase activation, DNA fragmentation, and cell death (CitationWollert and Drexler 2002, p 320). This is a thought-provoking hypothesis, as the majority of evidence suggests that a relative NO deficiency is present in African Americans. Utilization of ISDN-HYD therapy may indeed replete NO in this group, possibly altering steady state NO balance without causing the deleterious cellular effects ().
Figure 3 Consequences of nitric oxide and super oxide balance disruption in heart failure patients. Adapted from CitationHare (2004).
These preliminary data suggest impairment in NO production as well as endothelial dysfunction in African Americans as a mechanism for several vascular complications, including endothelial damage, hypertension-related complications, concentric left ventricular hypertrophy and possibly the progression of left ventricular dysfunction due to hypertension in the absence of ischemic heart disease. This is a hypothesis that will require careful testing before these mechanisms can be deemed definitive.
Effects of hydralazine on oxidative stress and nitrate tolerance
Although HYD is a potent vasodilator, progressive investigations suggest that reduction in oxidative stress and nitrate tolerance are as likely associated with the clinical benefit seen in patients with heart failure (CitationUnger et al 1993; CitationGogia et al 1995; CitationDiaber et al 2005). HYD has been associated with reduction of free radical scavengers in vitro, primarily from dose-dependent reduction of superoxide and peroxynitrite signaling (CitationDaiber et al 2005). Daiber and colleagues also evaluated the effects of HYD on nitroglycerin-induced superoxide and peroxynitrite production from cardiac mitochondria in vitro. In a dose-dependent fashion, HYD suppressed the production of the free radicals, suggesting that HYD attenuated oxidative stress in a nitrate rich environment.
Multiple studies have evaluated HYD effects on nitrate tolerance in the setting of heart failure (CitationCohn et al 1986; CitationCohn et al 1991; CitationGogia et al 1995; CitationTaylor et al 2004; CitationDaiber et al 2005; CitationElkayam and Bitar 2005). Gogia and colleagues evaluated the hemodynamic effects of intravenous nitroglycerin with HYD in patients with heart failure. A total of 28 patients (2 groups of 14) received a 24-hour infusion of nitroglycerin either with or without oral HYD administration. Use of HYD was associated with sustained reductions in blood pressure, pulmonary artery pressure, and mean pulmonary artery wedge pressure, whereas these effects quickly weaned in the group receiving only nitroglycerin (CitationGogia et al 1995). This study and others suggest that HYD is associated with sustained effect of nitrate administration by reducing overall tolerance of therapy.
Based on this background of basic science, provocative mechanistic data and clinical observation, the African American Heart Failure Trial (A-HeFT) was initiated to evaluate the use of ISDN-HYD in African American patients with advanced systolic heart failure already treated with evidence-based neurohormonal blockade.
The A-HeFT experience
The A-HeFT study randomized 1050 African American patients with moderate to severe systolic heart failure (NYHA III and IV) to fixed-dose ISDN-HYD therapy or placebo (CitationTaylor 2003, Citation2005; CitationTaylor et al 2004). A fixed-dose tablet of HYD 37.5 mg and ISDN 20 mg was administered 3 times daily (total daily dose HYD 112.5 mg and ISDN 60 mg). The dose was titrated to 2 tablets 3 times daily, for a total dose of HYD 225 mg and ISDN 120 mg. The maximum doses and frequency of ISDN-HYD were lower in the A-HeFT trial when compared with V-HeFT I and II (HYD 300 mg, ISDN 160 mg). The majority of all patients within the trial were taking diuretics, ACE-I/angiotensin receptor blockers, beta-blockers, and digoxin. Approximately 38%–40% of the patients were receiving aldosterone antagonists at the time of enrollment. The average ejection fraction for both groups was 24%. At the end of the trial, approximately 68% of the patients achieved maximal therapy in the ISDN-HYD group. The primary endpoint was a composite score composed of weighted values for death from any cause, first hospitalization for heart failure, and quality of life at 6 months. The Minnesota Living with Heart Failure questionnaire was used to assess quality of life. This was the first heart failure trial that utilized this composite endpoint. The composite system was designed to consider all mortality/morbidity events that contribute to heart failure outcome (CitationTaylor 2003). Secondary outcome included the separate components of the composite system, death from cardiovascular causes, the total number of hospitalizations for any reason, the total number of days of hospitalization, the overall quality of life throughout the trial, the number of unscheduled emergency room and clinic visits, the change in B-type natriuretic peptide level at six months, new need for cardiac transplantation, and change in myocardial remodeling at six months (CitationTaylor et al 2004, p 2050).
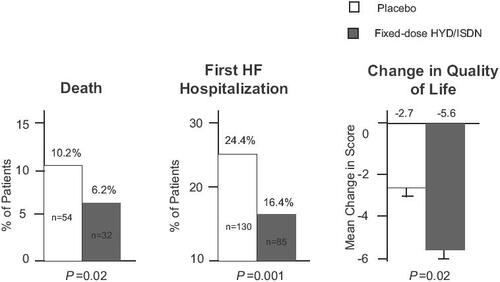
The study was terminated early as there was a significantly lower mortality in the ISDN-HYD group (6.2% vs 10.2% in the placebo group, p = 0.02). The mean duration of follow-up was 10 months. Overall, there was a 43% reduction in mortality with the use of ISDN-HYD therapy (10.2% in the placebo group vs 6.2% in the ISDN-HYD group; Hazard Ratio 0.57, p = 0.01). The primary endpoint composite score was also significantly improved in the ISDN-HYD group. Based on the prespecified endpoints, quality of life was improved as well. There was a 33% reduction in the rate of first hospitalization in the ISDN-HYD group compared with the placebo group, as well as a reduced rate of severe heart failure exacerbations in the treatment group ().
Figure 4 Components of the composite score in A-HeFT.Adapted fromCitationTaylor et al (2004).
Although there was a dramatic reduction in mortality for the patients receiving ISDN-HYD therapy in the A-HeFT study, the Kaplan-Meier survival curves did not separate until approximately 180 days after randomization. The reason for this occurrence is not yet understood. The fact that both groups of patients were receiving optimal neurohormonal antagonism and diuretic therapy may explain why the survival curves did not separate earlier. However this may also suggest a survival advantage from improvement of pump function due to a reverse remodeling effect. Further analyses of the trial data are ongoing to confirm this hypothesis. Nevertheless, these findings of the A-HeFT study firmly establish the use of ISDN-HYD combination in addition to evidence based neurohormonal blockade in African Americans with moderately severe to severe heart failure. The data are less clear for the use of this combination vasodilator therapy in patients with mild heart failure (NYHA I or II), as there was virtually no enrollment of these populations in the A-HeFT study.
Genetic implications and “race-based therapeutics”
Although self-reported race or ethnicity is currently the basis for patient selection related to this therapeutic intervention, it is clear that race is neither a scientific or physiological grouping and merely represents a placeholder for some other more objective marker of disease and/or response to therapy. It is plausible that genetic variations or polymorphisms may offer better explanations for differential effects of some therapies (CitationYancy 2005). Genetic variants of the alpha2cadrengergic receptor (α2cDel322-325) and β1-adrenergic receptor (β1Arg389) have been associated with increased risk for heart failure (CitationSmall et al 2002). The alpha2c-adrengergic receptor is partially responsible for feedback regulation of norepinephrine release in the sympathetic nerves. The presence of the genetic variant α2cDel322-325 of this receptor is associated with decreased regulatory function and increased presynaptic release of norepinephrine from the sympathetic ganglion (CitationHein et al 1999). The β1-adrenergic receptor variant (β1Arg389) of the cardiomyocyte has been associated with increased coupling to the stimulatory G protein, increasing intracellular cyclic AMP. This overstimulation of the cardiac myocytes produce increased chronotropy and inotropy, placing the heart at greater risk for failure (CitationSmall et al 2002).
Small and colleagues evaluated a small cohort of African American and Caucasian patients with and without heart failure to assess whether these genetic variants were related to increased frequency of heart failure. Although all patients homozygous for the α2cDel322-325 allele were at greater risk for developing heart failure, the African American patients were more commonly homozygous for this allele. African Americans also had a higher association with the combination homozygous alleles of α2cDel322-325 and β1Arg389 receptor variant, which significantly increased their risk for heart failure, when compared with the Caucasian patients of the cohort (odds ratio 10.11, 95% CI, 2.11–48.53, p = 0.004).
Recent investigations from the genetics substudy of A-HeFT (GRAHF study) regarding the NOS3 gene have also yielded some intriguing findings, in relation to African Americans with heart failure. A genetic variant of the NOS3 gene (Asp298 variant) has been previously detected and correlated with worse outcome in Caucasian patients with systolic dysfunction (CitationMcNamara et al 2003). The Asp298 variant of the NOS3 gene has a shorter-half-life in vitro, which is thought to be responsible for reduce nitric oxide production (CitationTesauro et al 2000). The Genetic Risk Assessment in Heart Failure (GRAHF) study evaluated the NOS3 polymorphisms within the African American cohort, and detected the Asp298 variant in approximately 80% of the patients (CitationMcNamara et al 2005). This frequency was significantly higher than the 56% frequency detected in a previous Caucasian cohort (CitationMcNamara et al 2003). These studies and others provide new insight into the genetic variants and outcome of the African American population with systolic heart failure. Further evaluation of “gene-tailored” therapies is now required to assess whether this mode of treatment will alter the overall outcome and prognosis in this group.
Conclusion
Growing evidence now suggests that there are definite differences in the experience of heart failure as it affects African Americans. It is evident that the presumed etiology of left ventricular dysfunction, the natural history of the disease and responsiveness to standard therapeutic interventions may vary. Prior to the A-HeFT study, the data regarding the benefit of ISDN-HYD therapy in African Americans lacked statistical power to demonstrate significant benefit in any group. However, after almost 20 years of effort, investigators have demonstrated that utilization of ISDNHYD in addition to standard medical therapy for heart failure tested specifically for African Americans with heart failure is effective and appropriate. Although the results of A-HeFT are of interest, emphasis of other evidence based strategies must not go unnoticed, as there are no data to support discontinuance or avoidance of other appropriate therapies for African American patients with heart failure. As well, it is presumed that these findings are not race-specific but rather that within the African American cohort, there are a sufficient number of responders to uncover a strong signal of efficacy. The work that now needs to be done is that which will uncover the specific epidemiological, clinical, biological and genetic signals specific for this robust response to ISDN-HYD.
References
- American Heart AssociationHeart disease and stroke statistics–2006 update2006 Accessed January 2, 2005. URL: http://www.americanheart.org/downloadable/heart/1136308648540Statupdate2006.pdf
- BristowMRMechanistic and clinical rationales for using beta-blockers in heart failureJ Card Fail200062 Suppl 18110908093
- CarsonPZiescheSJohnsonGRacial differences in response to therapy for heart failure: Analysis of the Vasodilator-Heart Failure TrialsJ Card Fail1999517818710496190
- CardilloCKilcoyneCMCannonRORacial differences in nitric oxide-mediated vasodilator response to mental stress in the forearm circulationHypertension199831123512399622135
- CohnJNArchibaldMPZiescheSEffect of vasodilator therapy on mortality in chronic congestive heart failureN Engl J Med19863141547523520315
- CohnJNJohnsonGZiescheSA comparison of enalapril with hydralazine-isosorbide dinitrate in the treatment of chronic congestive heart failureN Engl J Med1991325303102057035
- DaiberAMulschAUlrichHThe oxidative stress concept of nitrate tolerance and the antioxidant properties of hydralazineAm J Cardiol20059625i36i15979427
- DriesDLExnerDVGershBJRacial differences in the outcome of left ventricular dysfunctionN Engl J Med19993406091610029645
- ElkayamUBitarFEffects of nitrates and hydralazine in heart failure: Clinical evidence before the African American heart failure trialAm J Cardiol200596Suppl37i43i
- ExnerDVDriesDLDomanskiMJLesser response to angiotensin-converting-enzyme inhibitor therapy in black as compared with white patients with left ventricular dysfunctionN Engl J Med20013441351711333991
- GogiaHMehraAParikhSPrevention of tolerance to hemodynamic effects of nitrates with concomitant use of hydralazine in patients with chronic heart failureJ Am Coll Cardiol1995261575807594088
- HareJMNitroso-redox balance in the cardiovascular systemN Engl J Med20043512112211415533853
- HeinLAltmanJDKobilkaBKTwo functionally distinct a2adrenergic receptors regulate sympathetic neurotransmissionNature199940218118410647009
- HuntSAAbrahamWTChinMHACC/AHA 2005 guideline update for the diagnosis and management of chronic heart failure in the adult: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Update the 2001 Guidelines for the Evaluation and Management of Heart Failure): developed in collaboration with the American College of Chest Physicians and the International Society for Heart and Lung Transplantation: endorsed by the Heart Rhythm SocietyCirculation2005112e15423516160202
- JanssensSPokreiszPSchoonjansLCardiomyocytespecific overexpression of nitric oxide synthase 3 improves left ventricular performance and reduces compensatory hypertrophy after myocardial infarctionCirc Res20049412566215044322
- KahnDFDuffySJEffects of black race on forearm resistance vessel functionHypertension20024019520112154113
- KalinowskiLDobruckiITTomasianDRace-specific differences in endothelial function: Predisposition of African Americans to vascular diseaseCirculation200410925111715159296
- KonstamMARousseauMFKronenbergMWEffects of the angiotensin converting enzyme inhibitor enalapril on the long-term progression of left ventricular dysfunction in patients with heart failure. SOLVD InvestigatorsCirculation19928643181638712
- MalinskiTUnderstanding nitric oxide physiology in the heart: A nanomedical approachAm J Cardiol200596Suppl13i24i15979424
- McNamaraDMHolubkovRPostavaLEffect of Asp298 variant of endothelial nitric oxide synthase on survival for patients with congestive heart failureCirculation2003107159860212668492
- McNamaraDMTamSWSabolinskiMLThe genetic risk sub-study of the African American heart failure trial (A-HeFT): Impact of genetic variation of NOS32005Abstract presented at the 2005 Heart Failure Society of America national conference Retrieved June 22, 2006 from http://www.abstracts2view.com/hfsa05/view.php?nu=HFSA5L1_232
- MERIT-HF Study GroupEffect of metoprolol CR/XL in chronic heart failure: Metoprolol CR/XL Randomised Intervention Trial in Congestive Heart Failure (MERIT-HF)Lancet19993532001710376614
- PackerMBristowMRCohnJNThe effect of carvedilol on morbidity and mortality in patients with chronic heart failureN Engl J Med19963341349558614419
- PierpontGLCohnJNFranciosaJACombined oral hydralazine-nitrate therapy in left ventricular failure: hemodynamic equivalency to sodium nitroprussideChest73813620563
- PrabhuSDNitric oxide protects against pathological ventricular remodeling: Reconsideration of the role of NO in the failing heartCirc Res20049411557
- SmallKMWagonerLELevinAMSynergistic polymorphisms of b1- and a2c-adrenergic receptors and the risk of congestive heart failureN Engl J Med200234711354212374873
- TaylorALThe African American heart failure trial (A-HeFT): rationale and methodologyJ Card Fail20039SupplS2161914583892
- TaylorALZiescheSCombination of isosorbide dinitrate and hydralazine in blacks with heart FailureN Engl J Med200435120495715533851
- TaylorALThe African American heart failure trial: A clinical trial updateAm J Cardiol200596Suppl44i8i16226935
- TesauroMThompsonWCRoglianiIntracellular processing of the endothelial nitric oxide synthase isoforms associated with differences in severity of cardiopulmonary diseases: cleavage of proteins with aspartate vs glutamate at position 298Proc Natl Acad Sci U S A2000972832510717002
- The Beta-Blocker Evaluation of Survival Trial InvestigatorsA trial of the beta-blocker bucindolol in patients with advanced chronic heart failureN Engl J Med20013441659166711386264
- The CONSENSUS Trial Study GroupEffects of enalapril on mortality in severe congestive heart failure: results of the Cooperative North Scandinavian Enalapril Survival Study (CONSENSUS)N Engl J Med19873161429352883575
- The SOLVD InvestigatorsEffect of enalapril on survival in patients with reduced left ventricular ejection fractions and congestive heart failureN Engl J Med1991324293302
- UngerPBerkenboomGFontaineJInteraction between hydralazine and nitrovasodilators in vascular smooth muscleJ Cardiovasc Pharmacol1993214784837681511
- WagonerLEStarlingRCO’ConnorCMCardiac function and heart failureJ Am Coll Cardiol2006471822
- WollertKCDrexlerHRegulation of cardiac remodeling by nitric oxide: Focus on cardiac myocyte hypertrophy and apoptosisHeart Failure Reviews200273172512379817
- YancyCWHeart failure in african americansAm J Cardiol200596Suppl3i12i