Abstract
The additive manufacturing industry achieved a corporate annual growth rate of 25.9% according to the Forbes analysis of the Wohlers Report 2016. This high growth rate is placed in perspective when looking at the past 27 years where the corporate annual growth rate has averaged 26.2% each year indicating that additive manufacturing is clearly a growing industry. Such growth needs to be supported by suitable quality testing methods: with the economic success achieved in this market and the associated transition from mass production toward mass customization comes the need for new and innovative methods to assess the quality of the 3D printed geometries. This will be especially important for pharmaceutical products where a sub-standard quality of the final product can have detrimental consequences for patient health and safety.

Conventional quality control
Quality control is in its simplest form performed by visual inspection of the dosage form by the operator. This is of course a very subjective quality control method and is highly dependent on the skill of the operator in question. Furthermore, it is also a time-consuming, labor-intensive and thus expensive operation [Citation1]. It is therefore crucial to develop standardized methods with quantitative potential for quality control purposes. Conventional production of pharmaceutical products is characterized by a high output volume of a given product, the so-called production batches. This high batch volume output allows for monitoring the product quality by measuring the batch-to-batch consistency. Thus, in a conventional production setting product consistency can be related to, for example, the mass variation of tablets or the release profile of the drug in a dissolution test, where a small portion of a produced batch of tablets is subjected to either a weight measurement or a dissolution experiment [Citation2].
Quality control for 3D printed dosage forms
Additive manufacturing in all its current embodiments provides endless possibilities for designing geometries using a wide range of materials [Citation3] and a recent study has investigated how patient's rate different shapes of 3D printed oral dosage forms [Citation4]. In essence, even the cheapest consumer 3D printer can render infinitely many designs, so everybody capable of using computer-aided design (CAD) software can now create shapes that would have been otherwise too complex to produce using conventional manufacturing methods. An interesting question is what ramifications such transition from mass production toward mass customization will bring to various industries. As an example, given the highly regulated nature of the pharmaceutical market, it is hard to envisage commercial production of 3D printed pharmaceutical dosage forms without incorporating a well-structured and approved quality control system into the 3D printing production platform [Citation5–9]. This necessitates a strict requirement of the quality control techniques for the 3D printed dosage form to be sensitive to the features of customization, such as different geometries, drug concentrations and drug combinations, while remaining sufficiently robust to be applicable to all variations within a product line and sensitive to determine the analytical marker in question. So in essence, the product diversity that directly follows from the opportunities provided by mass customization means that quality measurements can no longer be solely based on measuring the variation between the produced dosage forms because potentially the produced dosage form may be a ‘one of a kind’ that will only be administered once to a single patient. In this context, a simulation approach may be the only feasible path for predicting the release profile of a given 3D printed pharmaceutical product [Citation10].
Quality control becomes an even more tenacious issue when anticipating the regulatory demands that will be required for 3D printed dosage forms [Citation11]. This is related to the personalization of, inter alia the drug dose and drug-release controlling structures (), which may yield a formulation that provides adequate treatment for a specific patient, but only for this one patient. Hence, a strong emphasis on supplying the correct 3D printed dosage form to the correct patient is crucial for ensuring safe medication.
Visualization of 3D printed drug products
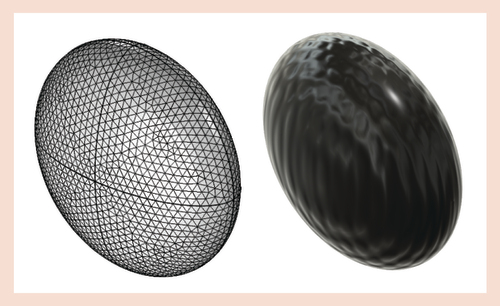
Many aspects of 3D printing rely on the fact that the 3D printed dosage form is printed according to a specific CAD file and it is hence necessary to have analytical techniques in place that can verify whether the printed dosage form matches the geometry specified in the CAD drawing (). Furthermore, an additional prerequisite is of course that the evaluation technique/measurement is nondestructive.
In this respect, classical optical imaging solutions can be useful techniques due to their short acquisition times and nondestructive nature. Such simple imaging measurements of the printed pharmaceutical product can be performed by a healthcare specialist responsible for printing or dispensing the product [Citation8], or even by the patient using a mobile phone or other suitable camera [Citation12]. Simple optical images provide information on the external dimensions, the surface area as well as overall shape and structure. The images can resolve visual homogeneity or lack thereof of the 3D printed dosage form. Furthermore, the comparatively low cost of many classical optical imaging systems and accessories compared with other analytical equipment makes such solutions ideal techniques for initial characterization purposes. Optical imaging may deliver information on the print accuracy by providing geometrical assessments on the macro-scale of the object [Citation13]. Furthermore, in cases where the 3D printed dosage forms are subjected to dissolution testing, conventional imaging may provide additional information on the erosion and/or dissolution of the 3D printed dosage form in situ during the dissolution test [Citation14]. It is important to note that the nondestructive nature of optical imaging at visible frequencies is lost if fracturing, erosion and dissolution of the sample is required in order to assess, for example, inner structures.
Different image analysis algorithms will assist in transforming either optical images or scanning electron microscopy (SEM) images into providing quantifiable outputs [Citation8]. Such quantifiable outputs may be of high relevance when comparing images in relations to, for example, surface porosities. In general, it can be inferred that the possibility for converting images that are inherently qualitative into quantifiable outputs greatly diminishes the subjectiveness of such image comparisons and thus adds value to the images and their interpretations.
Implementation of machine vision may be regarded as an advancement of the previously described image analysis where machine vision in its extended form is intended to apply to setups where real-time control of the 3D printing process is achieved during actual printing of the object. The potential of implementing machine vision in the production of 3D printed geometries has been reported in the scientific literature for several decades [Citation15–19]. This technology would make it possible to implement real-time detection of defects in the object during printing [Citation19]. Misprinted objects could be discarded immediately.
In comparison to conventional optical imaging, SEM techniques provide the possibility to study the microscale of the 3D printed objects. Microscale information enables the possibility to study attributes of the 3D printing process such as print resolution, print layer heights [Citation20] and surface porosities [Citation21] in the samples. Furthermore, phenomena such as pore formation can be assessed by SEM imaging techniques [Citation22]. Using SEM imaging, it has been possible to characterize the microscale morphology of the samples as well as providing a qualitative assessment of the surface roughness [Citation23]. It has previously been shown that the surface porosity of 3D printed drug products can be quantified based on image analysis of SEM images [Citation21]. It should be noted that if the 3D printed drug product needs to be gold coated prior to SEM analysis then the nondestructive nature of SEM analysis is lost and that SEM typically samples only a very small proportion of the sample surface and hence it is imperative to identify representative samples from the object under investigation.
In addition to these relatively simple and well-established imaging methods there are a number of more advanced methods that can be used to gain tomographic insight into the 3D printed dosage form for quality testing. The potential of two methods, x-ray computed microtomography (XμCT) and terahertz pulsed imaging (TPI), has been demonstrated in this context. XμCT has been utilized for examining 3D printed structures for more than a decade [Citation24–28]. XμCT combined with appropriate data processing has been shown to provide the capability for contrasting the physical volume occupied by a 3D printed dosage form to the CAD schematics of that dosage form () [Citation27].
The blue regions represent domains where XμCT data indicate missing material according to the CAD model. The red regions represent domains where the XμCT data identifies deposited material outside the CAD model.
CAD: Computer-aided design; XμCT: x-ray computed microtomography.
Reprinted with permission from [Citation27].
![Figure 3. 3D representation of x-ray computed microtomography data and computer-aided design model.The blue regions represent domains where XμCT data indicate missing material according to the CAD model. The red regions represent domains where the XμCT data identifies deposited material outside the CAD model.CAD: Computer-aided design; XμCT: x-ray computed microtomography.Reprinted with permission from [Citation27].](/cms/asset/00cdacdb-1ab8-4ad5-8a93-5181a7c2ba1b/idpm_a_12339815_f0004.jpg)
This method has shown that 3D printing is capable of reproducing the same geometry very accurately between repeated prints but that the geometry of the printed object may deviate significantly from the original CAD file. Furthermore, the XμCT technique can deliver quantitative information on important parameters such as pore volume, shell thickness and total print volume of the 3D printed dosage form. However, at present XμCT measurements require significant time for data acquisition and analysis. Both aspects can be potentially addressed by future developments in technology but the use of ionizing x-ray radiation will mean that these techniques will be more suited for analysis in specialized laboratories and at the production line rather than at the point-of-care. Another, potentially even more feasible technique is TPI that, when contrasted to XμCT, lacks in spatial resolution and penetration depth but on the other hand has fast measurement times and utilizes nonionizing radiation. Both XμCT and TPI are still evolving technologies for the application in quality testing of 3D printed dosage forms and further work is required to make them widely applicable and explore their full capabilities [Citation27].
Future potential of 3D printed dosage forms
The following part of the paper will provide a glance at some of the possible benefits that may be achieved by producing drug products by 3D printing. Ideally, in order to facilitate production of truly personalized medicine a universal drug delivery system should be used, which should always work for all conceivable formulations. 3D printing of a compartmental ‘container’ could be such a universal drug delivery system. In order to achieve production of truly personalized medicine, one should aspire to obtain the highest degree of freedom to incorporate modifications in the 3D printed design. Therefore, it may be prudent to subdivide the 3D printing process into smaller independent modules thereby creating a modular design.
A modular design approach could be implemented as a design principle for 3D printed medicines, so that no matter what active pharmaceutical ingredient (API) is chosen it should not affect the selection of 3D printer materials, the printing process, disintegration of the dosage form, etc. This can only be achieved by using a modular design where it is assured that the API and the 3D printer material do not interfere with each other. Thus, it may be envisioned that 3D printed dosage forms will be composed of an outer 3D printed shell that consists of a 3D printed material that has desirable attributes in relation to, for example, disintegration mechanism and aqueous solubility. Furthermore, the 3D printed dosage form can be designed to have any desirable number of internal compartments into which API in any given state of matter and drug formulation may be loaded ().

One of the main reasons for implementing a modular design approach is to avoid interactions between drugs and/or 3D printer materials, as any material interaction may affect, for example, the printing process by shifting material properties such as melting point, melt viscosity and mechanical strength. It can thus be argued that when multiple APIs may be combined in a single dosage form, the possible interactions and problems may scale toward infinity and thus it is essential that there should not be any interactions at all, that may affect the printing process, disintegration of the dosage form, etc. Otherwise it would be impossible to produce anything that is remotely personalized in such a multi-API dosage unit without first having to optimize the process settings that might have been affected by any API and 3D printer material interaction.
Future perspective
The following will sketch some of the possible directions for the advancement of research within 3D printing of medicinal products. First, 3D printing based on a modular systems approach is desirable as it provides the possibility to obtain a feasible production of personalized 3D printed medicine. Second, analytical techniques capable of assessing the print quality have to be devised and, finally, simulation packages or analytical equations must be implemented in order to estimate the behavior of a given 3D printed drug formulation.
Future 3D printing based production systems will benefit from being equipped with measurement solutions that assure that the 3D printed drug product is produced as intended. For a highly regulated industry such as the pharmaceutical industry this will be a prerequisite for adopting 3D printing technology of personalized medicines. Optical imaging may be a first step toward real-time quality control as it is an affordable technique. Furthermore, the persistent growth in computer chip processing power should also facilitate quantitative image analysis as a viable path for analyzing future 3D printed dosage forms, thus achieving a real-time quantification of otherwise inherently qualitative images. The recent progress with XμCT and TPI setups points toward one feasible solution as these analytical methods provide spatially resolved tomographic characterization data of 3D printed dosage forms and as such provide more information than conventional optical imaging. The relatively higher price for XμCT and TPI setups than for their conventional optical counterparts should of course also be considered, alongside the higher complexity of the instruments and data analysis routines. However, recent advances in XμCT technologies may allow in future at-line implementation, whereas commercial TPI systems could already be used for on-line/at-line or even in-line quality control [Citation29–31].
Supplying the correct 3D printed dosage form to the correct patient is crucial.
Implementation of machine vision is needed in order to obtain real-time detection of defects.
Modular design approaches are needed in order to avoid interactions between drugs and/or 3D printer materials.
Recent advances in x-ray computed microtomography technology may in future allow at-line implementation.
Commercial terahertz pulsed imaging systems can already be utilized for in-line quality control.
Financial & competing interests disclosure
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.No writing assistance was utilized in the production of this manuscript.
References
- Trnka H , WuJX, Van De WeertM, GrohganzH, RantanenJ. Fuzzy Logic-based expert system for evaluating cake quality of freeze-dried formulations. J. Pharm. Sci.102(12), 4364–4374 (2013).
- Yu LX . Pharmaceutical quality by design: product and process development, understanding, and control. Pharm. Res.25(4), 781–791 (2008).
- Gross BC , ErkalJL, LockwoodSY, ChenC, SpenceDM. Evaluation of 3D printing and its potential impact on biotechnology and the chemical sciences. Anal. Chem.86(7), 3240–3253 (2014).
- Goyanes A , ScarpaM, KamlowM, GaisfordS, BasitAW, OrluM. Patient acceptability of 3D printed medicines. Int. J. Pharm.530(1), 71–78 (2017).
- Sandler N , KassamakovI, EhlersH, GeninaN, YlitaloT, HaeggstromE. Rapid interferometric imaging of printed drug laden multilayer structures. Sci. Rep.4, 4020 (2014).
- Vakili H , KolakovicR, GeninaNet al. Hyperspectral imaging in quality control of inkjet printed personalised dosage forms. Int. J. Pharm.483(1–2), 244–249 (2015).
- Khorasani M , EdingerM, RaijadaD, B⊘tkerJ, AhoJ, RantanenJ. Near-infrared chemical imaging (NIR-CI) of 3D printed pharmaceuticals. Int. J. Pharm.515(1), 324–330 (2016).
- Wickström H , NymanJO, IndolaMet al. Colorimetry as quality control tool for individual inkjet-printed pediatric formulations. AAPS PharmSciTech18(2), 293–302 (2017).
- Zema L , MelocchiA, MaroniA, GazzanigaA. Three-dimensional printing of medicinal products and the challenge of personalized therapy. J. Pharm. Sci.106(7), 1697–1705 (2017).
- Boetker J , RaijadaD, AhoJet al. In silico product design of pharmaceuticals. Asian J. Pharm. Sci.11(4), 492–499 (2016).
- Alhnan MA , OkwuosaTC, SadiaM, WanK-W, AhmedW, ArafatB. Emergence of 3D printed dosage forms: opportunities and challenges. Pharm. Res.33(8), 1817–1832 (2016).
- Han S , BaeHJ, KimJet al. Lithographically encoded polymer microtaggant using high-capacity and error-correctable QR code for anti-counterfeiting of drugs. Adv. Mater.24(44), 5924–5929 (2012).
- Wang J , GoyanesA, GaisfordS, BasitAW. Stereolithographic (SLA) 3D printing of oral modified-release dosage forms. Int. J. Pharm.503(1–2), 207–212 (2016).
- Alhijjaj M , BeltonP, QiS. An investigation into the use of polymer blends to improve the printability of and regulate drug release from pharmaceutical solid dispersions prepared via fused deposition modeling (FDM) 3D printing. Eur. J. Pharm. Biopharm.108, 111–125 (2016).
- Fang T , JafariMA, BakhadyrovI, SafariA, DanforthS, LangranaN. Online defect detection in layered manufacturing using process signature. Presented at: Systems, Man, and Cybernetics, 1998. 1998 IEEE International Conference on. San Diego, CA, USA, 14 October (1998).
- Cheng Y , JafariMA. Vision-based online process control in manufacturing applications. IEEE Trans. Automation Sci. Eng.5(1), 140–153 (2008).
- Ceruti A , LiveraniA, BombardiT. Augmented vision and interactive monitoring in 3D printing process. Int. J. Interact. Des. Manufac. doi:10.1007/s12008-016-0347-y1–11 (2016) ( Epub ahead of print).
- Okarma K , FastowiczJ. No-reference quality assessment of 3D prints based on the GLCM analysis. Presented at: 2016 21st International Conference on Methods and Models in Automation and Robotics (MMAR). Miedzyzdroje, Poland, 29 August – 1 September (2016).
- Straub J . Initial work on the characterization of additive manufacturing (3D printing) using software image analysis. Machines3(2), 55 (2015).
- Goyanes A , Robles MartinezP, BuanzA, BasitAW, GaisfordS. Effect of geometry on drug release from 3D printed tablets. Int. J. Pharm.494(2), 657–663 (2015).
- Boetker J , WaterJJ, AhoJ, ArnfastL, BohrA, RantanenJ. Modifying release characteristics from 3D printed drug-eluting products. Eur. J. Pharm. Sci90, 47–52 (2016).
- Khaled SA , BurleyJC, AlexanderMR, YangJ, RobertsCJ. 3D printing of tablets containing multiple drugs with defined release profiles. Int. J. Pharm.494(2), 643–650 (2015).
- Water JJ , BohrA, BoetkerJet al. Three-dimensional printing of drug-eluting implants: preparation of an antimicrobial polylactide feedstock material. J. Pharm. Sci.104(3), 1099–1107 (2015).
- Narra N , BlanquerSBG, HaimiSP, GrijpmaDW, HyttinenJ. mu CT based assessment of mechanical deformation of designed PTMC scaffolds. Clin. Hemorheol. Micro.60(1), 99–108 (2015).
- Inzana JA , OlveraD, FullerSMet al. 3D printing of composite calcium phosphate and collagen scaffolds for bone regeneration. Biomaterials35(13), 4026–4034 (2014).
- Wang F , ShorL, DarlingAet al. Precision extruding deposition and characterization of cellular poly-epsilon-caprolactone tissue scaffolds. Rapid Prototyping J.10(1), 42–49 (2004).
- Markl D , ZeitlerJA, RaschCet al. Analysis of 3D prints by x-ray computed microtomography and terahertz pulsed imaging. Pharm. Res.34(5), 1037–1052 (2017).
- Gioumouxouzis CI , KatsamenisOL, BouropoulosN, FatourosDG. 3D printed oral solid dosage forms containing hydrochlorothiazide for controlled drug delivery. J. Drug Deliv. Sci. Technol.40(Supplement C), 164–171 (2017).
- May RK , EvansMJ, ZhongSet al. Terahertz in-line sensor for direct coating thickness measurement of individual tablets during film coating in real-time. J. Pharm. Sci.100(4), 1535–1544 (2011).
- Haaser M , GordonKC, StrachanCJ, RadesT. Terahertz pulsed imaging as an advanced characterisation tool for film coatings – a review. Int. J. Pharm.457(2), 510–520 (2013).
- Hancock BC , MullarneyMP. X-ray microtomography of solid dosage forms. Pharm. Technol. Hosp. Pharm.29(4), 92–100 (2005).

