Abstract
Aim: Knee osteoarthritis is a degenerative disease complicated by pain and functional limitation. Newer pain-relieving interventions include pulsed radiofrequency (PRF), but studies on its efficacy have limitations including lack of control group and retrospective design that prevent sound conclusions. Materials & methods: We conducted a blind prospective randomized sham-controlled crossover pilot trial according to the CONSORT guidelines, to evaluate the efficacy of ultrasound-guided saphenous nerve PRF in gonarthritis pain. Results: Sixteen patients completed the study. Pain and function significantly improved after real PRF (numerical rating scale mean difference = 3.31), which was superior to sham PRF over time for pain (3 months) and function (6 months). Conclusion: PRF of the saphenous nerve is an alternative to relieve pain in gonarthritis. Our results provide data to support a sample size calculation for future trials.
Clinical trial registration: NCT04454710
Lay abstract
Aim: Knee osteoarthritis is a degenerative disease associated with severe pain and functional limitation. While treatment options exist to manage knee arthritis symptoms, few have achieved very good results. Newer pain-relieving treatments include pulsed radiofrequency (PRF), where electrical pulses are delivered to the painful nerves to change the way electrical signals are transmitted and reduce pain, but studies on its efficacy have limitations that prevent sound conclusions. Materials & methods: We conducted a study specifically designed to reveal efficacy of PRF over a sham (fake) treatment in patients affected by severe knee arthritis by targeting one single nerve involved in transmitting pain signals from the knee. Results: Pain and function significantly improved after real PRF, which was superior to sham PRF over time for pain (3 months) and function (6 months). Conclusion: PRF of the saphenous nerve is an alternative to relieve pain in knee arthritis.
Knee osteoarthritis (OA) is a chronic degenerative and multifactorial disease [Citation1] which is clinically relevant in a patient population with multiple comorbidities, thus narrowing the available treatment options [Citation2]. Progressive joint degeneration is the leading feature of knee OA, which is aggravated by aging and obesity [Citation1,Citation3]. It is characterized by functional limitation, severe pain, decreased function and quality of life [Citation4]. There is a variety of treatment options to manage the knee OA related symptoms, including nonpharmacological, pharmacological and surgical interventions. Indeed, lifestyle modifications such as weight loss and physical therapy are considered first-line interventions whereas second line pharmacological treatments include paracetamol, nonsteroidal anti-inflammatory drugs and opioids [Citation5]. In addition, intra-articular corticosteroids [Citation6], hyaluronic acid [Citation7] and platelet-rich plasma injections [Citation8] have been used to manage OA-related symptoms, despite studies on efficacy of these agents produced inconclusive or temporary results [Citation1]. Recent evidence suggests that pain management is a key feature for optimal nonpharmacological management of gonarthritis [Citation9], but none of the proposed interventions has clearly demonstrated improvement and/or prevention of the underlying pathology and disease progression. Hence, there is still a need for effective pain relieving strategies to delay or avoid total knee arthroplasty [Citation9].
Minimally invasive techniques such as radiofrequency ablation (RFA) and cooled RFA (CRFA) have been investigated for OA pain. Current in the radiofrequency range (500 KHz) delivered to neural tissues provides a heat-mediated lesion of nerve structure [Citation10], which targeting nerves that convey nociceptive inputs from the knee, can result in long-term pain relief. Indeed, a recent review showed that, genicular nerve RFA led up to 60% improvement from the baseline knee pain for at least 6 months [Citation11] and a number of clinical trials have demonstrated the efficacy of CRFA in providing 12 months of pain relief in knee OA [Citation12,Citation13]. However, unwanted adverse effects of irreversible tissue damage have been described after ablative radiofrequency of genicular nerves due to injury of neighboring neurovascular structures (pseudoaneurysm, hemarthrosis, patella injury) [Citation14].
An alternative to conventional RFA and CRFA is pulsed radiofrequency (PRF) which is executed in intermitted electrical pulses (usually delivering a current of 500 KHz in 20 ms pulses at a frequency of 2Hz), to keep target temperature below 42°C and thereby avoiding macroscopic destruction of neural tissue from thermal injury, while preserving the pain relief benefit via electrostatic field neuromodulation. Indeed, evidence exists for changes in ion channel activity and c-fos production in the spinal cord after PRF that may lead to long-term depression of nociception [Citation15].
There is enough basic science and clinical evidence to support PRF for neuropathic pain, whereas its role in nociceptive pain still deserves investigation [Citation16].
Interventional studies that applied PRF either on genicular nerves or saphenous nerve concluded that PRF is safe, and may act as a new noninvasive technique by providing significant pain reduction and increased function [Citation17–20]. The saphenous nerve is an alternative candidate target for PRF to reduce pain perception in knee OA. It is a sensory cutaneous branch of the femoral nerve that gives the innervation of the knee joints in the medial area by giving off suprapatellar and infrapatellar genicular nerves [Citation21]. This nerve is a common target for nerve block in case of procedural anesthesia and postprocedural pain management [Citation22].
Despite promising results of PRF of the saphenous nerve, the previous studies were affected by limitations including underpowered sample, lack of control group, short follow-up duration and poor procedural methodology [Citation18,Citation23]. Here we propose a prospective pilot randomized sham-controlled trial with the aim of evaluating efficacy and safety of ultrasound-guided saphenous nerve PRF in patients with chronic OA knee pain, and its impact on disability and quality of life. Our secondary objective is to provide data to support a sample size calculation for future fully powered trials.
Materials & methods
Trial design
This is a pilot double-blind randomized crossover interventional study of 16 participants with knee OA. The study protocol was approved by the ethics committee of the Policlinico Tor Vergata Hospital in Rome, Italy (Study Protocol 1204; Trial Register 144/2018) and complied with the declaration of Helsinki and the CONSORT statement. The trial is registered with ClinicalTrials.gov. Written informed consent was obtained from all participants prior to enrollment in the study.
Participants & eligibility criteria
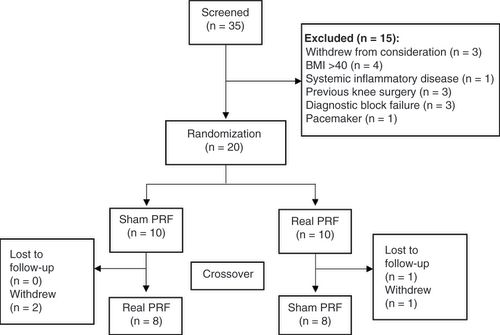
Thirty-five patients diagnosed with chronic knee OA (diagnosed with medical history, presentation, physical examination, x-ray and/or MRI) were screened for eligibility. Three declined participation and 12 did not meet the inclusion criteria Thus, twenty participants were enrolled in this trial ().
Inclusion criteria were: age between 18 and 80 years; Kellgren-Lawrence OA grades 3 or 4; duration of chronic pain of at least 6 months; patients unresponsive to conservative treatment as pharmacological therapy and physiotherapy; Pain relief >60% after two consecutive diagnostic blocks of the saphenous nerve.
Exclusion criteria were: BMI >40 kg/m2; systemic inflammatory disease; uncontrolled diabetes mellitus, malignancy, uncontrolled coagulopathy; previous history of allergic reactions to local anesthetics; previous history of knee surgery; any implanted electrical devices such as a cardiac pacemaker.
Intervention
After acquiring the informed consent, all patients underwent an ultrasound-guided diagnostic block of the saphenous nerve in adductor canal with 2 ml 2% lidocaine. Patients with a pain relief >60% were considered responders to the block and repeated the block for confirmation before entering the study. Responders were then randomized in two treatment groups using a computer-generated list: ‘real PRF’ and ‘Sham PRF’. All the procedures were performed in the supine position with the treated leg flexed at 30° and externally rotated by about 40°. A 10 cm long, 22 G straight radiofrequency cannula with a 120 mm radiofrequency probe and 5 mm active tip was used. All patients underwent sensitive stimulation (50 Hz, 0.3V) to detect the saphenous nerve. After a 2 ml of lidocaine 2% injection, either the real or the sham procedure was performed, according to the randomization schedule. In the PRF group the radiofrequency generator (Kimberly-Clark Baylis PMG-230-TD v3.1) was set to provide 20 ms bursts at a frequency of 2Hz for 120 s. The full procedure took 8 min, composed of four sessions of 120 s in which the temperature was below 42°C. In the sham group the radiofrequency generator operator carried out an equally long simulation and sham treatment. After a washout period of 6 months, subjects crossed over to the other arm of the study ().
Outcome measures
The outcome measures were selected among the core outcome domains suggested by the Initiative on Methods, Measurement, and Pain Assessment in Clinical Trials (IMMPACT) recommendations and included measures of pain intensity, physical functioning, quality of life and adverse events [Citation24].
Outcomes were evaluated at baseline (T0) and after 2 weeks (T1), 1 month (T2), 3 months (T3) and 6 months (T4). In addition, clinical and demographical data were gathered, including age, gender, BMI, comorbidities and previously used medications.
Pain intensity
The primary outcome was to assess pain relief evaluated by changes in the numerical rating scale (NRS) scores between baseline (T0) and at different times post-intervention. The 11-point NRS ranges from 0 (no pain at all) to 10 (the worst pain ever possible) and is a validated questionnaire with high sensitivity and specificity for the assessment of pain intensity [Citation25].
Physical functioning
Secondary outcomes included the assessment of physical function and disability by using the Italian version of the Oxford Knee Score (OKS) [Citation26].
The OKS have 12 items on daily activities, each item is scored from 1 (normal function) to 5 (extreme difficulty). The total score is the sum of the 12 items scores; thus, the best possible score is 12 and the worst possible score is 60 [Citation26].
Quality of life
Among other secondary outcomes we assessed the quality of life by the SF-36 questionnaire [Citation27]. The SF-36 consists of 36 items encompassed in 8 domains of health: physical function, role-physical, bodily pain, general health, vitality, social functioning, role-emotional and mental health. The higher the score the less disability, whereas the average score is 50 [Citation27]. We used the Italian validated version of SF-36 [Citation28].
Adverse events
We narratively collected any complaints and symptoms from patients undergoing the procedure at follow-up visits.
Blinding
Both, the patient and the doctor who collected post procedural questionnaires and pain ratings were blinded to what procedure was performed (real or sham). An independent physician performed the PRF in either real or sham mode. This physician was not engaged in recording, collecting or processing the data.
In order to improve the quality of blinding, after sensory testing and before PRF treatment, we injected 2 ml of lidocaine 2% through the infusion line of the RF cannula in order to reduce the degree of discomfort perceived by patients of the PRF group and to mask the lack of perception in those who were allocated in the sham group. Neither the patient nor the physician could look at the RF machine display during the procedure, and false operation sounds were emitted during the simulated procedure.
Statistical analysis
Since little has been published on the effects of PRF on pain, function and quality of life in patients with knee OA, a power analysis could not be based on previous research. Therefore, we chose an exploratory approach that did not limit sample size and enrolled volunteers who met the inclusion criteria.
The variables’ distribution was evaluated with the Shapiro–Wilk test, which showed normal distribution of the variables. The t-test was used to examine differences between groups at baseline. The repeated-measures analysis of variance (ANOVA) (with one between-subject factor [sham vs real PRF] and one within-subject factor [pre vs post-PRF T0, T1, T2, T3 and T4]) followed by post hoc t-tests (with Bonferroni correction) analyses for multiple comparisons were performed. A level of significance of p < 0.05 was set for all measures. Analysis was conducted in blind, using IBM-SPSS-22.
Results
Participant characteristics
Twenty patients were enrolled () and 16 participants (mean age 70.63 ± 9.51) completed the study. No significant baseline difference was found for each variable analyzed. The demographic and baseline clinical characteristic of the participants are displayed in . No adverse events were reported by any of the patients throughout the study.
Table 1. Clinical and demographical characteristics at screening of 16 participants who completed both arms of the crossover intervention.
Pain intensity
Mean NRS scores at different time points is provided in A. Mean NRS score decreased only in the PRF group compared with baseline and improvement was significant over 1-month (A). Repeated measure ANOVA, revealed that the main effect for time was statistically significant (F[4,60] = 12.23, p < 0.001, η2 = 0.44). Post hoc analysis indicated a significant difference between pre- and post-intervention (NRS mean difference = 3, p < 0.001) and a trend toward significance between pre-intervention and 1-month follow-up (NRS mean difference = 3.31, p < 0.001). However, post hoc analysis showed no significant differences between pre-intervention and 3 months follow-up or 6 months follow-up. ANOVA analysis revealed a significant main effect of time for pain severity scores (p < 0.001). A significant interaction between time × group was found also for NRS scores (p = 0.04) ().
(A) Pain Intensity measured by NRS at study time points (baseline [T0] and after 2 weeks [T1], 1 month [T2], 3 months [T3] and 6 months [T4]). A statistically significant pain reduction was observed only after real PRF until 1-month after the procedure. (B) OKS at study time points (baseline [T0] and after 2 weeks [T1], 1 month [T2], 3 months [T3] and 6 months [T4]). A statistically significant improvement of function was observed only after real PRF until 3 months after the procedure.
m: Mean; NRS: Numerical rating scale; OKS: Oxford Knee Score; PRF: Pulsed radiofrequency; SD: Standard deviation.
![Figure 2. Within-groups variation of pain intensity and OKS at study time-points compared to baseline. (A) Pain Intensity measured by NRS at study time points (baseline [T0] and after 2 weeks [T1], 1 month [T2], 3 months [T3] and 6 months [T4]). A statistically significant pain reduction was observed only after real PRF until 1-month after the procedure. (B) OKS at study time points (baseline [T0] and after 2 weeks [T1], 1 month [T2], 3 months [T3] and 6 months [T4]). A statistically significant improvement of function was observed only after real PRF until 3 months after the procedure.m: Mean; NRS: Numerical rating scale; OKS: Oxford Knee Score; PRF: Pulsed radiofrequency; SD: Standard deviation.](/cms/asset/77daeeeb-9eaa-4158-bb55-bf26d068adea/ipmt_a_12344472_f0002.jpg)
The Bonferroni post hoc comparison showed a statistically significant difference in NRS scores between real and sham PRF groups at T1 (NRS mean difference = 2, p < 0.001), T2 (NRS mean difference = 2.18, p < 0.001), and T3 (NRS mean difference = 1.28, p = 0.03) compared with baseline T0, but no significant difference was observed between T0 and T4 (NRS mean difference = 0.75, p = 0.20).
No difference between baseline NRS scores was observed between the groups matched according to the order of randomization (sham then real and real then sham).
Physical function
Function and disability improved significantly only after real-PRF and these improvements are sustained 1 month and 3 months after the intervention (B). Repeated measure ANOVA, revealed that the main effect for time was statistically significant (F[4,60] = 10.67, p < 0.001, η2 = 0.41). Post hoc analysis revealed a significant difference between pre- and post-intervention (OKS mean difference = -8.50, p < 0.008), a trend toward significance between pre-intervention and 1-month follow-up (OKS mean difference = -13, p < 0.000), and between pre-intervention and 3 months follow-up (OKS mean difference = -10, p < 0.003). By contrast, sham-PRF showed no improvement in disability or function at any time point. ANOVA analysis revealed a significant main effect of time for physical function and disability scores (p < 0.001). A significant interaction between time × group was found also for OKS scores (p < 0.001) ().
The Bonferroni post hoc comparison showed a significant improvement in OKS scores between real and sham PRF groups at T1 (OKS mean difference = -5.25, p < 0.001), T2 (OKS mean difference = -7.65, p < 0.001), T3 (OKS mean difference = -5.87, p < 0.001) and T4 (OKS mean difference = -4.40, p = 0.03) compared with baseline T0.
Quality of life
All the patients completed the SF-36 questionnaires at each visit during the study period. The real-PRF showed no significant improvement in the SF-36 items except the pain items that improved significantly in all time points compared with baseline (). Patients who received sham-PRF showed no significant improvement in the quality of life at any time point ().
Table 2. SF-36 domains at study time points (baseline [T0], after 2 weeks [T1], 1 month [T2], 3 months [T3] and 6 months [T4]).
Concerning SF-36 items, a main effect of time was found for pain (p < 0.001), energy and fatigue (p < 0.001), and role of limitation from emotional problems (p < 0.001). In addition, significant interaction between time × group was observed only in energy and fatigue item (p < 0.001). No significant interactions between time × group were found for other SF-36 items after real versus sham stimulation ().
Table 3. Between groups changes in primary and secondary outcomes (ANOVA with repeated measures).
The results of Bonferroni post hoc comparison pointed out a significant improvement in pain item between real and sham PRF group at T1 (mean difference = -8.90, p < 0.001), T2 (mean difference = -11.64, p < 0.001), T3 (mean difference = -9.92, p = 0.02) and T4 (mean difference = -10.10, p = 0.01) compared with baseline T0. In addition, Bonferroni post hoc comparison results showed a significant difference between real and sham PRF groups in the role of limitations from emotional problems item at T2 (mean difference = -19.78, p = 0.02) and T3 (mean difference = -35.41, p < 0.001) compared with baseline T0, however, no significant differences were observed at T1 (mean difference = -11.21, p = 0.60) or T4 (mean difference = -23.25, p = 0.11) compared with baseline. Bonferroni post hoc comparison between real and sham PRF group showed that energy and fatigue items significantly improved only at 3 months follow-up (T3) (mean difference = -14.40, p < 0.001) compared with baseline T0.
Adverse events
No major adverse events or side effects were reported by any of the patients throughout the study. Ten out of twenty patients complained for discomfort during the needle positioning to obtain optimal stimulation parameters and this was the reason why three patients dropped out.
Discussion
To best of our knowledge, this is the first double blind randomized control trial that assessed efficacy and safety of PRF of the saphenous nerve on pain, function and quality of life of patients with gonarthritis. Real PRF is effective to reduce pain severity compared with sham PRF and pain relief is sustained up to 3 months follow-up. Consistently, function showed a sustained significant improvement in the same time frames. Moreover, the improvement of SF-36 domains ‘pain’, ‘fatigue and energy’ as well as ‘limitations from emotional problems’ may be a consequence of pain relief. Overall, our analysis favors real PRF over sham to improve pain and function and quality of life. In line with our results, two previous retrospective studies of PRF treatment of the saphenous nerve showed a significant reduction in pain and function scores in 115 OA patients resistant to conventional therapies [Citation18] and in 84 patients with cardiac comorbidities affected by grade 3–4 gonarthritis [Citation23], respectively. Both these studies revealed a 6 months efficacy of PRF on pain and function, but their retrospective design and the lack of a control group limit the generalization of their results. Our trial was designed to reveal superiority of real PRF over sham PRF. A longer effect over time should be investigated on a dedicated trial. In fact, PRF treatment is not a disease-modifying intervention. As such, it does not affect the etiology of pain, rather, it is hypothesized that it exerts a modulating effect by influencing the activity of the synapses of the dorsal horn and/or it reduces nociceptive input. Persistence of nociceptors activation from peripheral mechanism may act against the PRF effect and shorten the analgesic effect. Indeed, it is unknown how long the supposed mechanisms of analgesia could last, and there might be a wide inter-individual variability.
Two prospective studies include the saphenous nerve as part of a combined procedure on OA knee pain [Citation17,Citation29]. Tabasco et al. combined conventional and PRF on genicular and saphenous nerves respectively, and showed no relevant reduction in pain intensity after treatment [Citation29]. Vas et al. reported sustained pain relief and muscle relaxation in ten patients after PRF on sensory and motor nerves supplying the knee [Citation17].
Current evidence on PRF of the saphenous nerve brings out a limited time laps efficacy compared with other radiofrequency procedures to the knee. Indeed, a prospective, multi-center, randomized, cross-over trial comparing CRFA of genucular nerves to a single hyaluronic acid injection revealed a 12-month ≥50% pain relief and a 46.2% improvement of the Western Ontario and McMaster Universities Arthritis (WOMAC) score in 65.2% of subjects undergoing CRFA [Citation30]. Likewise, a 6-month efficacy was shown in a randomized trial comparing RFA to analgesic block with corticosteroid [Citation31]. By contrast, a retrospective study reporting 3 months efficacy of RFA of the genicular nerves (50% pain relief in 52% of patients), showed loss of efficacy at 6 months [Citation11]. This variability in study outcomes may depend on several reasons, including trial design. Indeed, we believe that two items are of utmost importance in this setting, in other words, patient selection and technique application method, which may represent the strengths of this study, together with its randomized controlled trial (RCT) design. We selected patients carefully after two consecutive diagnostic blocks of saphenous nerve before PRF treatment. Indeed, given the complexity of the innervation of the knee joint, an anesthetic block to confirm analgesia is mandatory before targeting the saphenous for PRF. Pain can arise from any portion of the knee joint, and several peripheral nerves may convey the nociceptive input with different contributions. In addition to the saphenous nerve, the innervation of the knee derives from the branches of the sciatic and obturator nerves. In particular, superomedial and inferomedial genicular nerves derive from the tibial nerve and convey information from the posterior knee joint while the common peroneal nerve contributes to the superior lateral genicular nerve to the anterior portion of the knee. With a variable contribution, a posterior branch of the obturator nerve can provide a branch to the posterior knee. Thus, pain transmission may continue in spite of single nerve block or RF treatment.
As for PRF technique application method, ultrasound guidance and a precise sensitive stimulation to better localize the target nerve may ensure better outcomes.
A recent systematic review and meta-analysis explored ultrasound guided RF procedures for pain relief in knee OA targeting genicular nerves, sciatic nerve or intra-articular treatment targets [Citation32]. Ultrasonography guidance resulted an effective, safe and easily applicable method for radiofrequency pain relief in knee OA. Indeed, ultrasonography has several advantages over fluoroscopy, besides preventing exposure to ionizing radiation. It ensures a dynamic examination and tissues and arteries visualization as well as real-time needle advancement. As such, ultrasonography can improve the accuracy of the needle proximity and thus the efficacy of the procedure. Once on the target nerve, a sensitive stimulation performed through the radiofrequency needle may add accuracy to the target search. Indeed, experimental studies suggest that an electrode placed beyond 2000 μm is too far to get any effect on target nerve, whereas if closer than 500 μm, either continuous or PRF, produce tissue damage, being a distance of 1000–500 μm the optimal one [Citation33]. In the attempt to obtain an always equal needle-nerve distance, we standardized sensitive stimulation in our series and applied the treatment protocol only if a pain or paresthesia was evoked in the usual region of pain by 0.3 V current at 50Hz. However, we are aware that other factors may affect the treatment performance and reproducibility.
A recent RCT showed that RFA was superior to PRF on genicular nerves of patients suffering from gonarthritis grade 3–4 [Citation34]. These results, together with the evidence of efficacy of CRFA in the recent literature [Citation30] may render our results obsolete. However, we believe that PRF of the saphenous nerve can still be an effective method to relieve knee pain caused by OA when RFA treatment of the genicular nerves proves to be technically difficult. Moreover, PRF can be applied when RFA fails to relieve pain by inducing nerve lesions and subsequent neuropathic pain. Furthermore, in patients whose compliance is poor, a single nerve treatment appears to be more acceptable than four genicular nerves treated. At last, PRF may predict peripheral stimulation implantation.
There are limitations of the present study. First, our findings are based on a small sample of 16 individuals. Second, the blinding mechanism may not be sufficient to mask the sham procedure. Third, all patients were affected by severe arthritis (grade 3–4 Kellgren-Lawrence) and the average BMI was high. Perhaps, a different study population may reach longer positive outcomes. Fourth, a fixed protocol may not account for patient variability. The PRF technique could be optimized taking in mind that all the nerve fibers should receive a sufficient amount of energy/current density. By producing strong electric-fields and temperature spikes that can extend well into the 45–50°C levels, PRF induces changes in the trans-membrane potentials of neurons that may lead to lower the frequency of nociceptive inputs to the spinal cord thereby inducing a long-term depression of synaptic efficiency, which is relevant to long-term antinociception. As such, by modulating pulse-width, exposition time and by changing the needle-to-nerve angle during the procedure may increase fibers recruitment and thereby efficacy and/or duration. Previous systematic reviews that compared the effectiveness of different types of radiofrequency on knee OA reported inconsistent procedural methodology in the published studies [Citation35]. Therefore, standardizing the radiofrequency technique in order to optimize tissue exposure to current could be a key point to ensure effective results. A further limitation resides in the crossover design of the study, which might be affected by biases such as a carry-over effect or an order effect. In principle, the first might confound the estimates of the second treatment due to an insufficiently long wash-out period. The second may generate an expectation bias related to the order in which treatment is administered.
Our data show no significant long-term (T4) difference of NRS scores compared with baseline (T0). Yet, we observed no differences between the groups compared by order of randomization, in either primary or secondary outcome measures. These results may suggest a long enough washout period before the second treatment was performed. However, the analgesic effect of real PRF could last longer than the 6 months washout period used in this study, thereby affecting basal pain levels of the following sham treatment for those who received PRF first. This limitation is intrinsic in the crossover study design, and testing for analytical control of carry-over effect is debated in literature [Citation36].
Thus, we recommend further studies specifically designed to establish the mean duration of analgesia after PRF of the saphenous nerve, to identify the target population that could benefit most from the procedure and to optimize the treatment protocol. We believe that the present study will provide data to support a sample size calculation for future fully powered trials.
Conclusion
Besides pharmacological treatments, which have several limitations and limited efficacy, minimally invasive techniques represent a valid option to reduce nociceptive inputs from the knee. PRF of the saphenous nerve is an alternative to safely relieve pain in knee OA, also guaranteeing an improvement in disability. Moreover, PRF of the saphenous nerve can replace genicular nerves ablation when these nerves are difficult to find/treat. However, the procedure is operator dependent and further studies are recommended to define optimal treatment protocol and patient population.
Future perspective
While RFA and CRFA for chronic knee pain seems to be largely successful, PRF may ensure analgesia by avoiding tissue lesions. However, as several mechanisms underpin chronic gonarthritis pain, including inflammation, central sensitization as well as neuropathic pain mechanism [Citation37], the scientific community deserves the rationale behind the use of PRF in any manifestation of gonarthritis pain to be established. Future good quality research to define stimulating patterns, patient selection, stage of disease at which this approach is more appropriate [Citation16] may provide broader treatment options to offer analgesia to patients with other causes of chronic knee pain, as well as to those who complain of knee pain after total knee arthroplasty.
Knee osteoarthritis (OA) is a chronic, degenerative and multifactorial disease complicated by functional limitation, severe pain and decreased quality of life.
Pain management is a key part of the treatment algorithm for knee OA.
While a disease modifying approach of knee OA is under investigation, a safe, effective and lasting analgesia is an unmet need that deserves a more structured investigation.
Radiofrequency ablation procedures have shown clinical effectiveness but they create areas of tissue destruction due to coagulative necrosis.
Pulsed radiofrequency (PRF) is an alternative to conventional radiofrequency ablation. It seems to primarily modulate pain transmission, thereby minimizing neural tissue injury.
The saphenous nerve, the largest branch of the femoral nerve innervating the medial portion of the knee and the lower leg, is a candidate target for PRF to treat knee OA pain.
Previous studies on PRF of the saphenous nerve were affected by several limitations thereby the results are questionable.
In this sham-controlled randomized pilot study we demonstrate efficacy of the saphenous nerve PRF on pain and function for in patients with severe OA.
A fixed stimulation protocol and ultrasound guidance ensure a more standardized approach.
Ethical conduct of research
The authors state that they have obtained appropriate institutional review board approval or have followed the principles outlined in the Declaration of Helsinki for all human or animal experimental investigations. In addition, for investigations involving human subjects, informed consent has been obtained from the participants involved.
Financial & competing interests disclosure
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
No writing assistance was utilized in the production of this manuscript.
Data sharing statement
The authors certify that this manuscript reports original clinical trial data. Deidentified, individual data that underlie the results reported in this article (text, tables, figures and appendices), along with the study protocol, will be available for meta-analyses for five years following publication. Parties seeking access to this information should submit a formal request to the corresponding author of this study.
References
- Katz JN , ArantKR , LoeserRF. Diagnosis and treatment of hip and knee osteoarthritis. JAMA325(6), 568 (2021).
- French HP , SmartKM , DoyleF. Prevalence of neuropathic pain in knee or hip osteoarthritis: a systematic review and meta-analysis. 47(1), 1–8 (2017).
- Hulshof CTJ , ColosioC , DaamsJGet al. WHO/ILO work-related burden of disease and injury: protocol for systematic reviews of exposure to occupational ergonomic risk factors and of the effect of exposure to occupational ergonomic risk factors on osteoarthritis of hip or knee and selected other. Environ. Int.125, 554–566 (2019).
- Araujo ILA , CastroMC , DaltroC , MatosMA. Quality of life and functional independence in patients with osteoarthritis of the knee. Knee Surg. Relat. Res.28(3), 219–224 (2016).
- Steinmeyer J , BockF , StöveJ , JeroschJ , FlechtenmacherJ. Pharmacological treatment of knee osteoarthritis: special considerations of the new German guideline. Orthop. Rev. (Pavia)10(4), 147–154 (2018).
- Arroll B , Goodyear-SmithF. Corticosteroid injections for osteoarthritis of the knee: meta-analysis. Br. Med. J.328(7444), 869–870 (2004).
- Jevsevar D , DonnellyP , BrownGA , CumminsDS. Viscosupplementation for osteoarthritis of the knee: a systematic review of the evidence. J. Bone Joint Surg. Am.97(24), 2047–2060 (2014).
- Rodriguez-Merchan EC . Intraarticular injections of platelet-rich plasma (PRP) in the management of knee osteoarthritis. Arch Bone Jt. Surg.1(1), 5–8 (2013).
- Kolasinski SL , NeogiT , HochbergMCet al. 2019 American College of Rheumatology/Arthritis Foundation Guideline for the Management of Osteoarthritis of the Hand, Hip, and Knee. Arthritis Rheumatol.72(2), 220–233 (2020).
- Jankowiak B , GauciCA. Manual of RF techniques: a practical manual of radiofrequency procedures in chronic pain management. CoMedical, The Netherlands (2011).
- Iannaccone F , DixonS , KaufmanA. A review of long-term pain relief after genicular nerve radiofrequency ablation in chronic knee osteoarthritis. Pain Physician20(2), E437–E444 (2017).
- Davis T , LoudermilkE , DepalmaMet al. Twelve-month analgesia and rescue, by cooled radiofrequency ablation treatment of osteoarthritic knee pain: results from a prospective, multicenter, randomized, cross-over trial. Reg. Anesth. Pain Med.44(4), 499–506 (2019).
- Kapural L , LeeN , NealK , BurchellM. Long-term retrospective assessment of clinical efficacy of radiofrequency ablation of the knee using a cooled radiofrequency system. Pain Physician22(5), 489–494 (2019).
- Kim SY , LePU , KosharskyyB , KayeAD , ShaparinN , DownieSA. Is genicular nerve radiofrequency ablation safe?A literature review and anatomical study. Pain Physician19(5), E697–705 (2016).
- Cosman ER , CosmanER. Electric and thermal field effects in tissue around radiofrequency electrodes. Pain Med. (2005).
- Cohen SP , Van ZundertJ. Pulsed radiofrequency: rebel without cause. Reg. Anesth. Pain Med.35(1), 8–10 (2010).
- Vas L , PaiR , KhandagaleN , PattnaikM. Pulsed radiofrequency of the composite nerve supply to the knee joint as a new technique for relieving osteoarthritic pain: a preliminary report. Pain Physician17(6), 493–506 (2014).
- Akbas M , LuleciN , DereK , LuleciE , OzdemirU , TomanH. Efficacy of pulsed radiofrequency treatment on the saphenous nerve in patients with chronic knee pain. J. Back Musculoskelet. Rehabil.24(2), 77–82 (2011).
- Yao P , HongT , LiG , HanZ , WangS , DingY. Comparing the safety and effectiveness of radiofrequency thermocoagulation on genicular nerve, intraarticular pulsed radiofrequency with steroid injection in the pain management of knee osteoarthritis. Pain Physician23(4 Special Issue), S295–S303 (2020).
- Erdem Y , SirE. The efficacy of ultrasound-guided pulsed radiofrequency of genicular nerves in the treatment of chronic knee pain due to severe degenerative disease or previous total knee arthroplasty. Med. Sci. Monit.25, 1857–1863 (2019).
- Jamison DE , CohenSP. Radiofrequency techniques to treat chronic knee pain: a comprehensive review of anatomy, effectiveness, treatment parameters, and patient selection. J. Pain Res.18 (11), 1879–1888 (2018).
- Herman DC , VincentKR. Saphenous nerve block for the assessment of knee pain refractory to conservative treatment. Curr. Sports Med. Rep.17(5), 146–147 (2018).
- Baysal PK , BaysalÖ , ErklllnçAet al. Is saphenous nerve radio frequency an effective treatment for advanced gonarthrosis in elders with cardiac comorbidity? J. Back Musculoskelet. Rehabil. 31(1), 113–118 (2018).
- Dworkin RH , TurkDC , FarrarJTet al. Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain113(1–2), 9–19 (2005).
- Hjermstad MJ , FayersPM , HaugenDFet al. Studies comparing numerical rating scales, verbal rating scales, and visual analogue scales for assessment of pain intensity in adults: a systematic literature review. J. Pain Symptom. Manage41(6), 1073–1093 (2011).
- Padua R , ZanoliG , CeccarelliE , RomaniniE , BondìR , CampiA. The Italian version of the Oxford 12-item knee questionnaire – cross-cultural adaptation and validation. Int. Orthop.27(4), 214–216 (2003).
- Garratt AM , RutaDA , AbdallaMI , BuckinghamJK , RussellIT. The SF36 health survey questionnaire: an outcome measure suitable for routine use within the NHS?Br. Med. J.306(6890), 1440–1444 (1993).
- Apolone G , MosconiP. The Italian SF-36 Health Survey: translation, validation and norming. J. Clin. Epidemiol.51(11), 1025–1036 (1998).
- Monerris Tabasco MM , RocaAmatria G , RíosMárquez N , JiménezCapel Y , SamperBernal D. Assessment of the effectiveness and safety of two radiofrequency techniques for the treatment of knee pain secondary to gonarthrosis. Prospective randomized double blind study. Rev. Esp. Anestesiol. Reanim.66(7), 362–369 (2019).
- Chen AF , KhaloufF , ZoraKet al. Cooled radiofrequency ablation provides extended clinical utility in the management of knee osteoarthritis: 12-month results from a prospective, multi-center, randomized, cross-over trial comparing cooled radiofrequency ablation to a single hyaluronic aci. BMC Musculoskelet. Disord.21(1), 363 (2020).
- Qudsi-Sinclair S , Borrás-RubioE , Abellan-GuillénJF , Padilladel Rey ML , Ruiz-MerinoG. A Comparison of Genicular Nerve Treatment Using Either Radiofrequency or Analgesic Block with Corticosteroid for Pain after a Total Knee Arthroplasty: A Double-Blind, Randomized Clinical Study. Pain Pract.17(5), 578–588 (2017).
- Huang Y , DengQ , YangLet al. Efficacy and safety of ultrasound-guided radiofrequency treatment for chronic pain in patients with knee osteoarthritis: a systematic review and meta-analysis. Pain Res. Manag.(2020).
- Cahana A , VutskitsL , MullerD. Acute differential modulation of synaptic transmission and cell survival during exposure to pulsed and continuous radiofrequency energy. J. Pain4(4), 197–202 (2003).
- Santana-Pineda MM , VanlinthoutLE , Santana-RamírezS , VannesteT , Van ZundertJ , Novalbos-RuizJP. A randomized controlled trial to compare analgesia and functional improvement after continuous neuroablative and pulsed neuromodulative radiofrequency treatment of the genicular nerves in patients with knee osteoarthritis up to one year after the intervention. Pain Med.22(3), 637–652 (2021).
- Gupta A , HuettnerDP , DukewichM. Comparative effectiveness review of cooled versus pulsed radiofrequency ablation for the treatment of knee osteoarthritis: a systematic review. Pain Physician. 20(3), 155–171 (2017).
- Mills EJ , ChanAW , WuP , VailA , GuyattGH , AltmanDG. Design, analysis, and presentation of crossover trials. Trials10(27), (2009).
- Polat CS , DoğanA , SezginÖzcan D , KöseoğluBF , KoçerAkselim S. Is there a possible neuropathic pain component in knee osteoarthritis?Arch. Rheumatol.32(4), 333–338 (2017).