Abstract
Although the pathogenesis of migraine is not fully understood, accumulating evidence indicates migraine may be driven by impaired brain energy metabolism in the context of pathologically high levels of adenosine. Considerable evidence indicates that aminophylline, an adenosine receptor antagonist, can provide strong therapeutic relief in pain, particularly post-dural headache. Moreover, direct observations from a previously published observational case series have demonstrated a strong therapeutic impact of low-dose aminophylline in patients with severe, unremitting migraine attacks. Although higher doses of aminophylline are associated with an unfavourable adverse effect profile, low doses of aminophylline are associated with minimal adverse effects. Despite this promise, double-blinded randomized trials will be needed to determine the true therapeutic efficacy of low-dose aminophylline in migraine.
Migraine & adenosine
Migraine is associated with impaired brain energy metabolism, which may be driven by pathologically high levels of adenosine.
Aminophylline & pain
By acting as an adenosine antagonist, considerable evidence indicates that aminophylline and its active ingredient, theophylline, can provide strong therapeutic relief in pain, particularly post-dural headache.
Aminophylline & migraine
Direct observations from a previously published observational case series indicated a strong analgesic role for low-dose aminophylline in severe, unremitting migraine.
Adverse effects
Low-dose aminophylline possesses a favourable safety profile compared with other existing drugs.
Migraine is a leading cause of disability worldwide, which leads to a huge socio-economic burden [Citation1,Citation2]. For a long time, migraine was thought to be of a vascular origin, but many researchers now agree that it is more of a neurological disorder [Citation3,Citation4]. In this brief review, we will describe the metabolic basis of migraine, including the essential role played by adenosine. Subsequently we will discuss the potential therapeutic application of aminophylline, an adenosine receptor antagonist, in the treatment of migraine, including a personal reflection on a previously published observational case series, which demonstrated that low-dose aminophylline was highly effective and safe in the treatment of patients with severe, unremitting migraine attacks.
Migraine & adenosine
Multiple lines of evidence indicate that migraine is fundamentally driven by impaired brain energy metabolism [Citation5–14]. Magnetic resonance spectroscopy studies have demonstrated impaired brain and muscle metabolism and mitochondria function in migraine patients, leading to inefficient glucose metabolism, decreased ATP levels and amplified oxidative stress [Citation12,Citation13]. It has been proposed that the migraine itself acts as an adaptive response to deficient cerebral energy reserves or excessive oxidative stress levels, which acts to restore energy levels and lowers levels of oxidative stress [Citation9,Citation14]. Increased levels of ADP, as well as decreased levels of organic phosphate and phosphorylation potential, are also seen in migraine patients [Citation9,Citation14], which implies that oxidative phosphorylation is diminished both during and between migraine attacks. Moreover, some observational studies have demonstrated an increased association of migraine sufferers with other disorders associated with impaired energy metabolism [Citation15,Citation16], such as Alzheimer’s disease [Citation17]. Furthermore, a metabolic-based treatment, the ketogenic diet, may reduce migraine attacks [Citation11,Citation17,Citation18].
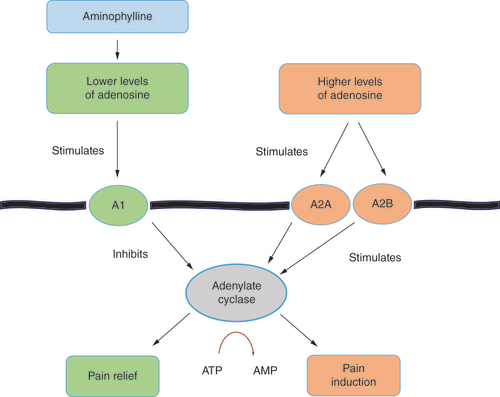
Adenosine, a catabolite of ATP that plays a role in many essential metabolic processes involved in inflammation, immune function, growth and sleep [Citation19–21], is positioned as a primary causal factor in the pathogenesis of migraine [Citation3]. Metabolic and mitochondrial dysfunction can impact the production of extracellular adenosine, which may contribute to inflammation and tissue hypoxia [Citation20,Citation22], leading to elevated levels of adenosine in the blood as seen in migraine [Citation21]. Adenosine is a vital molecule in metabolism, but it is a double-edged sword for pain, with lower levels associated with reduced pain [Citation3,Citation23–25], whereas higher levels are associated with the induction of pain [Citation3,Citation21,Citation26,Citation27]. In mice, for example, activation of adenosine A2B receptors on myeloid cells causes nociceptor hyper-excitability and promotes chronic pain via soluble IL-6 receptor trans-signalling [Citation26]. In a recent 2023 study involving human subjects, 18 patients received a relatively high-dose infusion of 120 mg per min over 20 min, of which 14 patients reported headache, although not the entire migraine syndrome [Citation27].
Such a concentration-dependent impact of adenosine on pain may relate to the different effects of its various receptors on adenylate cyclase, which catalyzes ATP to AMP (). Adenosine receptors are widely present in blood vessels, many organs, platelets, dendritic cells and the brain itself [Citation3,Citation20]. They are also present in every cell of the immune system [Citation20]. There are four known adenosine receptors: A1, A2A, A2B and A3. The A1 receptors, which are mainly associated with the relief of pain, are more active at lower adenosine levels than the other receptors [Citation3,Citation23]. Conversely, the A2A and A2B receptors are usually associated with the induction of pain, especially if adenosine levels are high [Citation3]. The A2B receptors have a much lower affinity for adenosine than the other three receptors and are activated at higher (including pathological) levels of adenosine [Citation3,Citation22].
Aminophylline & pain
Aminophylline is a compound of theophylline with ethylenediamine in a 2:1 ratio. Ethylenediamine improves the water solubility of theophylline, which is the active ingredient. Although these drugs have been used in asthma and chronic obstructive airways disease for over 80 years, more recent research has shown that aminophylline is also effective in relieving pain and migraine [Citation28–34], which may relate to aminophylline’s action as an adenosine antagonist. For example, in a 2002 randomized double-blinded study, aminophylline significantly reduced the pain of renal colic in most of the 70 patients studied [Citation28]. Moreover, a 2004 study noted that ischemic arm pain induced by experimentally prolonged blood pressure cuff inflation in healthy humans was attenuated by aminophylline [Citation29]. In a recent 2022 study, post-operative deep vitrectomy eye surgery patients experienced decreased post-operative pain when aminophylline was infused during the operation [Citation30].
Aminophylline and theophylline have also been well-studied in post-dural puncture headache, which was recently summarized in a 2023 systematic review and meta-analysis of 15 clinical studies that showed a therapeutic effect for both drugs [Citation31]. Even relatively low dosages of aminophylline and theophylline appear to be efficacious. For example, a 2011 study divided a cohort of 60 patients with post-dural puncture into three groups: group 1 received 200 mg theophylline + 1000 ml dextrose Ringer lactate (DRL) over 30 min; group 2 received 100 mg oral caffeine + 500 mg paracetamol + 1000 ml DRL; and group 3 received oral and intravenous placebo with 1000 ml DRL [Citation32]. The patients were asked to assess the degree of pain before and 1 h after the treatments using the Visual Pain Scala (VPS). In the first group (the theophylline treatment group), a statistically significant difference in the VPS was noted after the infusion. No statistically significant difference was noted in the second and third groups. It was concluded that theophylline infusion after spinal anesthesia was efficient, fast and did minimal harm during the headache therapy. Moreover, in a notable 2015 case report, a patient with a post-dural puncture headache was initially treated with tramadol, caffeine, and gabapentin but did not obtain significant relief [Citation33]. On day 4 of the headache, a moderately low dosage of 250 mg aminophylline in normal saline was commenced, which resulted in complete relief of the headache within 35 min, with no recurrence. There were no adverse effects of the aminophylline treatment. Furthermore, in a 2020 study, 55 of 65 patients with post-dural puncture headache were successfully treated with 200 mg aminophylline given over 45 min [Citation34]. Importantly, there were zero adverse side effects with the moderately low dosages infused. Blood pressures and pulse rates remained stable and were not significantly different pre- and post-infusion.
Aminophylline & migraine
While working as a general internist at Mills Memorial Hospital in Terrace (British Colombia, Canada), the lead author assisted the nuclear medicine department in performing nuclear cardiac exercise stress testing, as well as simulated exercise stress testing with nuclear imaging. Patients that could not exercise significantly were administered intravenous dipyridamole, an adenosine deaminase inhibitor that allows adenosine to accumulate in the blood stream and dilate the arteries (including coronary arteries), which simulates an exercise effect (this protocol was standard in many hospitals at the time) [Citation35]. The pre- and post-dipyridamole nuclear images were compared, with myocardial perfusion reduced in an atheromatous artery compared with a normal artery. Incidentally, we noted the dipyridamole infusion created a severe headache in about 20% of our patients, which was clinically very similar to migraine. As was standard practice by most hospitals, we routinely administered a low dose (50–150 mg) of intravenous aminophylline to treat the headache. Invariably, the headache and any other symptoms, such as mild confusion and fatigue, completely disappeared within minutes.
Given that the headache and associated symptoms seemed very similar to the migraine syndrome, the lead author and colleagues were prompted to commence an observational case series to determine the potential benefit of low-dose aminophylline in migraine, which to our knowledge has not been investigated before or since this study was published. In 2011, we observed 21 patients who attended our small hospital emergency department with severe, unremitting migraine headaches usually lasting from 8 to 48 h in duration [Citation36]. The protocol involved a mini-bag infusion of normal saline containing 100 mg of aminophylline over 10 to 20 min. No other medication was given by us. In 17 of 21 patients, rapid, usually complete pain relief occurred toward the end of the infusion. In two patients, we initially administered a placebo mini-bag of normal saline that did not contain aminophylline; the headaches persisted. In both patients, the mini-bag containing 100 mg of aminophylline was then infused over 10 min with complete relief of the headache by the end of the infusion. Notably, our case series involved patients with the entire migraine syndrome (as well as a history of migraine), with low-dose aminophylline not only abolishing the migraine headache but also any associated symptoms such as mild confusion, nausea and fatigue, generally within minutes. Importantly, there were several weaknesses in our case series - for example, it was unblinded, and it did not contain a dedicated control arm. Despite these shortcomings, the results indicated a strong analgesic role for low-dose aminophylline in severe, unremitting migraine.
Adverse effects
At low dosages (50 to 150 mg), aminophylline possesses a highly favourable safety profile compared with other existing drugs, which also tend to be expensive and less well-studied over time. Perhaps the most common drug used in headache relief is caffeine, another nonselective adenosine receptor inhibitor, which also has a relatively benign adverse effect profile. However, aminophylline is far more effective [Citation32,Citation33]. When used for asthma in the past, theophylline has been associated with a high frequency of adverse effects such as nausea and headaches, as well as rare complications including seizures and cardiac arrhythmias, necessitating the monitoring of theophylline plasma levels [Citation37]. However, importantly, these adverse effects occurred at dosages that were several-fold higher than those used in the above case series [Citation38]. While performing nuclear cardiology testing, during which the lead author treated hundreds of patients with low-dose aminophylline, no adverse effects were noted from this drug [Citation36], which parallels the experiences of others who have used aminophylline at similarly low doses [Citation39].
Conclusion
In conclusion, accumulating evidence implicates migraine as a disorder of impaired brain energy metabolism that is driven by pathologically high levels of adenosine. By acting as an adenosine antagonist, aminophylline can provide substantial therapeutic relief. Our observational case series indicates that low-dose aminophylline leads to the complete and rapid relief of severe, unremitting and treatment-resistant migraine attacks, as well as their associated symptoms. Moreover, low-dose aminophylline is associated with minimal adverse effects. Despite this promise, double-blinded randomized trials will be required to determine the true efficacy of aminophylline in the treatment of migraine.
Future perspective
Aminophylline is inexpensive, well-studied over time, and associated with few adverse effects at low doses that are therapeutic for even the most severe migraine attacks. However, it will only gain acceptance upon being studied in a double-blinded randomized controlled trial. If such a trial can be achieved and shown to be positive, aminophylline may gain more widespread use as an acute treatment in migraine.
Author contributions
Barrie L Phillips was involved in concept planning, interpretation, drafting of the first manuscript, review of subsequent manuscripts, and approval of the final manuscript. Matthew CL Phillips was involved in interpretation, review of subsequent manuscripts, and approval of the final manuscript.
Writing disclosure
No writing assistance was utilized in the production of this manuscript.
Acknowledgments
We would like to acknowledge and thank M Kenyon for his crucial partnership with the lead author in their aminophylline clinical research, and B Redpath for his insightful suggestions and review of the article.
Financial disclosure
The authors have no financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
Competing interests disclosure
The authors have no competing interests or relevant affiliations with any organization or entity with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, stock ownership or options and expert testimony.
References
- GBD 2016 Neurology Collaborators . Global, regional, and national burden of neurological disorders, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 18, 459–480 (2019).
- Gupta J , Gaurkar SS . Migraine: an underestimated neurological condition affecting billions. Cureus 14, e28347 (2022).
- Fried NT , Elliot MB , Oshinsky ML . The role of adenosine signalling in headache: a review. Brain Sci. 7, 30 (2017).
- Chen D , Willis-Parker M , Lundberg GP . Migraine headache: is it only a neurological disorder? Links between migraine and cardiovascular disorders. Trends Cardiovasc. Med. 7, 424–430 (2020).
- Wang Y , Wang Y , Yue G , Zhao Y . Energy metabolism disturbance in migraine: from a mitochondrial point of view. Front Physiol. 14, 1133528 (2023).
- Sangiorgi S , Mochi M , Riva R et al. Abnormal platelet mitochondrial function in patients affected by migraine with and without aura. Cephalgia 14, 21–23 (1994).
- Welch KMA , Levine SR , D’Andrea G , Schultz LR , Helpern JA . Preliminary observations on brain energy metabolism in migraine studied by in vivo phosphorous 31 NMR spectroscopy. Neurology 39, 538–541 (1989).
- Del Moro L , Rota E , Pirovano E , Rainero I . Migraine, brain glucose metabolism and the “neurogenic hypothesis”: a scoping review. J. Pain 23, 1294–1317 (2022).
- Gross EC , Lisicki M , Fischer D , Sándor PS , Schoenen J . The metabolic face of migraine - from pathophysiology to treatment. Nat. Rev. Neurol. 15, 627–643 (2019).
- Bohra SK , Achar RR , Chidambaram SB et al. Current perspectives on mitochondrial dysfunction in migraine. Eur. J. Neurosci. 56, 3738–3754 (2022).
- de Cassya Lopes Neri L , Ferraris C , Catalano G et al. Ketosis and migraine: a systematic review of the literature and meta-analysis. Front. Nutr. 10, 1204700 (2023).
- Barbiroli B , Montagna P , Cortelli P et al. Abnormal brain and muscle energy metabolism shown by 31 P magnetic resonance spectroscopy in patients affected by migraine with aura. Neurology 42, 1209–1214 (1992).
- Reyngoudt H , Paemeleire K , Descamps B , De Deene Y , Achten E . P-MRS demonstrates a reduction in high-energy phosphates in the occipital lobe of migraine without aura patients. Cephalalgia 31, 1243–1253 (2011).
- Hassan SA , Farooque U , Choudhry AS , Pillai B , Sheikh FN . Therapeutic implications of altered energy metabolism in migraine: a state-of-the-art review. Cureus 12, e8571 (2020).
- Kristoffersen ES , Børte S , Hagen K , Zwart J-A , Winsvold BS . Migraine, obesity and body fat distribution - a population-based study. J. Headache Pain 21, 97 (2020).
- Hurh K , Jeong SH , Kim SH , Jang S-Y , Park E-C , Jang S-I . Increased risk of all-cause, Alzheimer’s, and vascular dementia in adults with migraine in Korea: a population-based cohort study. J. Headache Pain 23, 108 (2022).
- Phillips MCL , Deprez LM , Mortimer GMN et al. Randomized crossover trial of a modified ketogenic diet in Alzheimer’s disease. Alzheimers Res. Ther. 13, 51 (2021).
- Valente M , Garbo R , Filippi F et al. Migraine prevention through ketogenic diet: more than body mass composition changes. J. Clin. Med. 11, 4946 (2022).
- Bjorness TE , Greene RW . Adenosine and sleep. Curr. Neuropharmacol. 7, 238–245 (2009).
- Haskó G , Antonioli L , Cronstein BN . Adenosine metabolism, immunity, and joint health. Biochem. Pharmacol. 151, 307–313 (2018).
- Guieu R , Devaux C , Henry H et al. Adenosine and migraine. Can. J. Neurol. Sci. 25, 55–58 (1998).
- Liu H , Xia Y . Beneficial and detrimental role of adenosine signalling in diseases and therapy. J. Appl. Physiol. (1985) 119, 1173–1182 (2015).
- Jung S-M , Peyton L , Essa H , Choi D-S . Adenosine receptors: emerging non-opioids targets for pain medications. Neurobiol. Pain 11, 100087 (2022).
- Zylka MJ . Pain-relieving prospects for adenosine receptors and ectonucleotidases. Trends Mol. Med. 17, 188–196 (2011).
- Luongo L , Guida F , Maione S , Jacobson KA , Salvamini D . Adenosine metabotropic receptors in chronic pain management. Front. Pharmacol. 12, 651038 (2021).
- Hu X , Adebiyi MG , Luo J et al. Sustained elevated adenosine via ADORA2B promotes chronic pain through neuro-immune interaction. Cell Rep. 16, 106–119 (2016).
- Thuraiaiyah J , Al-Karagholi MA , Elbahi FA , Zhuang ZA , Ashina M . Adenosine causes short-lasting vasodilatation and headache but not migraine attacks in migraine patients: a randomized clinical trial. Pain 164, 1118–1127 (2023).
- Djaladat H , Tajik P , Fard SA , Alehashemi S . The effect of aminophylline on renal colic: a randomized double blind controlled trial. South Med. J. 100, 1081–1084 (2007).
- Sergedahl M , Karelov A . Experimentally induced ischaemic pain in healthy humans is attenuated by the adenosine receptor antagonist theophylline. Acta Physiol. Scand. 180, 301–306 (2004).
- Farsani DM , Rafieezadeh A , Nourian N , Mohammadi H , Naghibi K , Saghir K . Evaluating the preventive effect of metoclopramide and aminophylline on pain after deep vitrectomy. Int. J. Physiol. Pathophysiol. Pharmacol. 14, 316–323 (2022).
- Barati-Boldaji R , Shojaei-Zarghani S , Mehrabi M , Amini A , Safarpour AR . Post-dural puncture headache prevention and treatment with aminophylline or theophylline: a systematic review and meta-analysis. Anesth. Pain Med. (Seoul) 18, 177–189 (2023).
- Akdere H , Burgazli K . The efficiency of intravenous theophylline on the headache which occurs after spinal anesthesia. J. Neurol. Res. 1, 190–192 (2011).
- Wu C , Lian Y , Xie N . Aminophylline injection alleviates pain in postdural puncture headache. Pain Med. 16, 2038–2040 (2015).
- Yıldırım HU , Bakir M , Rumeli Ş . Evaluation of theophylline efficiency in post-dural puncture headache. JARSS. 28, 247–254 (2020).
- Matte GG , Barnes DC , Abrams DN . Pharmacologic interventions in nuclear medicine assessment of cardiac perfusion. J. Pharm. Pharm. Sci. 4, 255–262 (2002).
- Kenyon M , Phillips B , DeWit C . Personal observation: intravenous aminophylline treatment for migraine. CJGIM. 7, 129–130 (2012).
- Barnes P . Current therapies for asthma: promise and limitations. Chest 111, S17–S26 (1997).
- Barnes P . Theophylline, new perspectives for an old drug. Am. J. Respir. Crit. Care Med. 167, 813–818 (2003).
- Shaat AM , Abdalgaleil MM . Is theophylline more effective than sumatriptan in the treatment of post-dural puncture headache? A randomized clinical trial. Egypt J. Anaesth. 37, 310–316 (2021).