Abstract
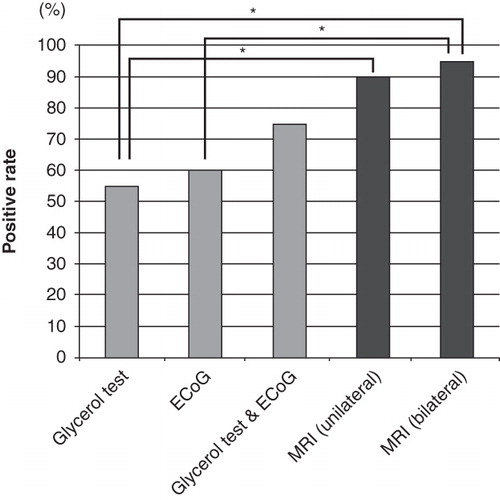
Conclusion. 3 T MRI after intratympanic injection of gadolinium-based contrast agent (GBCA) is more useful for the diagnosis of endolymphatic hydrops compared with the glycerol test and electrocochleography (ECoG). Objective: To investigate the relationship between 3 T MRI after intratympanic injection of GBCA, the glycerol test, and ECoG in patients with Meniere's disease (MD). Methods: A total of 20 patients with MD were evaluated. Diluted gadodiamide (a gadolinium-based contrast agent) was administered to the bilateral tympanic cavity by injection through the tympanic membrane. After 24 h, the endolymphatic hydrops was evaluated by a 3.0 T MR scanner. To investigate cochlear hydrops, the glycerol test and ECoG were carried out in all patients. Results: A positive result was observed in 11 patients (55%) in the glycerol test and in 12 patients (60%) by ECoG. The incidence of positive findings when evaluating the same patients with both the glycerol test and ECoG increased to 75%. Nineteen of 20 (95%) patients showed positive results for 3 T MRI.
Introduction
Meniere's disease (MD) is an idiopathic disorder of the inner ear characterized by fluctuating sensorineural hearing loss (SNHL), tinnitus, aural fullness, and recurrent spontaneous episodic rotational vertigo [Citation1]. MD has been thought to be attributable to endolymphatic hydrops (ELH), but this has only been confirmed histopathologically after death. Therefore, along with clinical symptoms, clinical tests suggestive for ELH are usually used for diagnosis. Functional testing including electrocochleography (ECoG) or the glycerol test has been used to estimate ELH. However, even if functional testing is performed, the results are still indirect proof.
Meanwhile, recent advances in imaging by three-dimensional, fluid-attenuated inversion recovery (3D-FLAIR) of magnetic resonance imaging (MRI), in association with enhancement by gadolinium-based contrast agents (GBCAs), enables visualization of ELH in patients with MD [Citation2–4]. We have succeeded in visualizing ELH semi-quantitatively in patients with MD, by using bilateral intratympanic GBCA administration with MRI [Citation5].
There have been few studies comparing 3 T MRI to other existing tests in patients with MD. In the present study, we attempted to compare the diagnostic value of 3 T MRI to ECoG and the glycerol test in patients with MD.
Material and methods
Subjects
Twenty patients with ‘definite’ unilateral MD who met the American Academy of Otolaryngology-Head and Neck Surgery (AAO-HNS) criteria participated in this study. Age, sex, period, and average hearing levels at 500 Hz, 1 kHz, and 2 kHz, are presented in .
Table I. Summary of patients' details.
To detect the ELH, all patients underwent three tests: glycerol, ECoG, and 3 T MRI. Because it is difficult to do these tests at the same time, they were done within 1 month. Eighteen of 20 patients underwent these tests during an acute phase (the period in which the patient's hearing is fluctuated). Two patients (nos 11 and 18) underwent the testing during a chronic stage of MD.
Glycerol test
The glycerol test was carried out to investigate cochlear hydrops. Pure tone audiometry (PTA) results were recorded before and 2 h after the intravenous administration of 500 ml of glycerol. A positive G-PTA was defined as an improvement of >10 dB in more than two frequencies.
ECoG test
ECoG was also used to investigate cochlear hydrops, with patients lying on a bed in a room that was acoustically and electrically shielded. An operating microscope was used to place a transtympanic electrode consisting of a sterilized stainless steel needle that was insulated except for the tip on the promontory wall. The reference and ground electrodes, applied to the earlobe and forehead, respectively, were silver chloride cup electrodes. The transtympanic ECoG was recorded by averaging 1000 sweeps after alternating click stimuli (rate: 15/s) with levels of 100 dB nHL. A ratio of the amplitudes of summation potential/action potential (SP/AP) >0.33 indicated ELH.
MRI
Gadodiamide (Omniscan, Daiichi Pharmaceutical Co. Ltd, Tokyo, Japan) was diluted eightfold with saline, and 0.4–0.6 ml of the diluted gadodiamide was administered to the bilateral tympanic cavity by injection through the tympanic membrane using a 23 G needle. The injection was carried out under a microscope. The patient then remained in the supine position for 60 min. After 24 h, the ELH was evaluated by MRI. We used a 3.0 T MR scanner (Trio, Siemens, Erlangen, Germany) with a receive-only eight-channel phased-array coil. It can perform T1-weighted three-dimensional (3D) magnetization prepared rapid gradient echo (MP-RAGE). The parameters for MP-RAGE were: TR, 1500 ms; TE, 3 ms; matrix size of 320 × 290 × 320; 72 axial 0.8 mm thick slice; 0.8 × 0.8 × 0.8 mm isotropic voxels; heavily T2-weighted 3D-TSE sequence; and 3D fluid-attenuated inversion recovery (FLAIR) with variable flip angle echo train (SPACE). The parameters for heavily T2-weighted SPACE were: TR 1350 ms; TE 199 ms; echo train length (ETL), 93; matrix size of 320 × 288 × 278; 56 axial 0.8 mm thick slice; and voxel size of 0.6 × 0.4 × 0.8 mm. In addition to the methods described previously, we used 3D-FLAIR with higher in-plane spatial resolution. The scan parameters for the 3D-FLAIR sequence were as follows: repetition time of 10 000 ms, echo time of 666 ms, inversion time of 2500 ms, single slab 3D turbo spin echo with variable flip angle distribution, echo train length of 173, matrix size of 320 × 320, 52 axial 0.8 mm thick slices to cover the labyrinth with a 20 cm square field of view, acceleration factor of two using the parallel imaging technique, and generalized autocalibrating partially parallel acquisitions. Voxel size was 0.7 × 0.8 × 0.8 mm. The number of excitations was one, and the scan time was 9 min.
ELH was evaluated based on either unilateral or bilateral imaging in this study. When using unilateral MRI, ELH was evaluated qualitatively from the image of the cochlea from 3D inversion recovery utilizing real reconstruction (3D real IR) image on the axial plane. In the case of bilateral MRI, quantitative evaluation was performed using the ratio of the areas of affected/unaffected <0.90 as an indication of ELH from the multiplanar reconstruction (MPR) image. The MPR image was created from all the slices (3D-FLAIR images) that included the labyrinth by imaging analysis software (Aquarius Net Viewer). The areas enhanced by gadodiamide in the cochlea and vestibule were traced manually and measured on the image in the plane perpendicular to the modiolus. Then, the affected side/contralateral side ratios were calculated. The detailed method was described in our previous report [Citation5].
The Ethics Review Committee of Shinshu University School of Medicine approved the protocol of the study and all patients gave their informed consent to participation.
Results
In this study, 3D real IR MRI clearly showed that the gadodiamide successfully penetrated the round window membrane, entered the perilymphatic space, and delineated the gadodiamide-enhanced perilymphatic and gadodiamide-negative endolymphatic spaces of the inner ear. The endolymphatic space is comparatively small and difficult to identify as a vacant area in the normal side. In contrast, the endolymphatic space in an ear with ELH is partially or entirely expanded, making identification of the endolymphatic space easier ().
Figure 1. MRI scan for patient no. 17 (definite MD). The endolymphatic hydrops (ELH) is detectable as a black area inside the perilymphatic space filled with the gadodiamide in the left cochlea (a: arrows) and vestibule (b: arrowhead). In the right cochlea, the endolymphatic space (a significantly small area) is not detectable, probably due to strong signal intensity in the perilymphatic space. In the right vestibule, endolympatic space is detectable, but significantly smaller than that found in the left vestibule. [A detailed serial image movie can be seen at: http://www.shinshu-u.ac.jp/faculty/medicine/chair/ent/MRIleft.mov]
![Figure 1. MRI scan for patient no. 17 (definite MD). The endolymphatic hydrops (ELH) is detectable as a black area inside the perilymphatic space filled with the gadodiamide in the left cochlea (a: arrows) and vestibule (b: arrowhead). In the right cochlea, the endolymphatic space (a significantly small area) is not detectable, probably due to strong signal intensity in the perilymphatic space. In the right vestibule, endolympatic space is detectable, but significantly smaller than that found in the left vestibule. [A detailed serial image movie can be seen at: http://www.shinshu-u.ac.jp/faculty/medicine/chair/ent/MRIleft.mov]](/cms/asset/5dabbed6-7fb3-4379-982a-c27877c72526/ioto_a_635383_f0001_b.jpg)
shows the positive results observed in 11 patients (55%) in the glycerol test and in 12 patients (60%) in ECoG. The incidence of positive findings when evaluating the same patients with both the glycerol test and ECoG increased to 75%. A positive result was observed in 18 patients (90%) by evaluating qualitatively unilateral MRI. Moreover, when evaluating the bilateral MRI quantitatively, the incidence of positive findings increased to 95%. provides a vertical bar chart presentation of the positive rate of each test.
Table II. Results of the glycerol test, ECoG, and 3 T MRI.
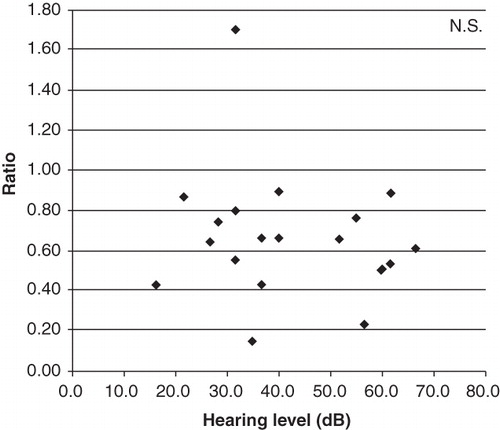
illustrates the relationship between the ratio and the hearing level, which showed no correlation.
Figure 3. A scatter plot displaying the relationship between the ratio and the hearing level (average of 0.5, 1, and 2 kHz).
No adverse effects, such as vertigo, hearing deterioration or tinnitus due to the intratympanic injection of gadodiamide were observed and there were no changes in hearing level.
Discussion
MD is a clinical disorder, characterized by fluctuating hearing loss, recurrent spontaneous episodic vertigo, tinnitus, and aural fullness, which may be defined as the idiopathic syndrome of ELH.
In general, the important tests for diagnosis of MD (to prove ELH indirectly) have been the glycerol test and ECoG. These are simple and rapid methods and several authors have confirmed their efficiency for identifying ELH. Several studies have reported that the sensitivity is about 60% with the glycerol test and the same for ECoG. Furthermore, when performed in combination, the sensitivity is about 80% [Citation6]. In this study, a positive result was observed in 11 patients (55%) in the glycerol test and in 12 patients (60%) in ECoG. The incidence of positive findings when evaluating the same patients with both the glycerol test and ECoG increased to 75%, which is consistent with previous reported findings.
On the other hand, there are a growing number of studies about diagnosing MD using 3 T MRI after intratympanic injection of GBCA [Citation2–4]. We further demonstrated the usefulness of MRI in diagnosing ELH using bilateral intratympanic GBCA administration in a quantitative manner [Citation5]. There were differences between the affected and unaffected sides in enhancement; we measured the areas enhanced by gadolinium in the cochlea and vestibule. Then, the affected side/unaffected side ratios were calculated. In patients with MD, the ratio was reduced. In this study, we used a 0.9 threshold to determine the laterality. As in our previous report, the vestibular endolymphatic space can be identified even on the unaffected side, making precise diagnosis for ELH difficult without bilateral comparison. Thus, when using unilateral MRI, we evaluated ELH only in the cochlea in contrast to bilateral MRI evaluation in which both cochlea and vestibular organs are included.
In this study, a positive result was observed in 18 patients (90%) by evaluating unilateral MRI. Moreover, when evaluating the bilateral MRI, the incidence of positive findings increased to 95%. Significant differences were found between bilateral MRI and the glycerol test and ECoG. Only one patient (no. 7) was negative based on bilateral MRI evaluation. This patient had a small eardrum perforation in the affected side, observed when intratympanic injection of GBCA was carried out. Therefore, infiltration of GBCA into the perilymphatic space might have been influenced by this perforation. However, even in this case ELH could be identified qualitatively. To avoid such factors, it is imperative that patients have no history of middle ear disease when comparing both sides.
Concerning the relationship between the ratio (degree of ELH) and hearing level, we could not find any correlation between ratio and hearing level (average of 0.5, 1, and 2 kHz).
Therefore, the present study did not support the concept that severe ELH exists in the patients with more profound hearing loss.
A series of studies reported that combination of different tests strengthens estimation of ELH. Ito et al. recently reported that with a test battery of ECoG and the furosemide test, abnormal responses were found in 51/58 (88%) patients with definite MD in each of the tests [Citation7]. Kimura et al. reported that 97% of 118 patients with definite MD showed at least one positive test result in a battery of three tests, and that the combination of three rather than two tests resulted in an improved diagnostic accuracy [Citation6]. Taguchi et al. also showed that 97% of 60 patients with ELH had at least one positive result in a battery of p-ADH, ECoG, and the glycerol test [Citation8]. The furosemide test and p-ADH are highly sensitive.
The present study clearly indicated that, among the various tests to prove ELH, 3 T MRI after intratympanic injection of GBCA is a more direct and accurate way to prove ELH, and is a powerful tool for diagnosis of MD. In addition, Miyagawa et al. reported that there is a shift of ratio as patient status changes, and bilateral MRI is beneficial to follow up individual patients [Citation9]. None of the patients who underwent 3 T MRI after intratympanic injection of GBCA had any changes in hearing level after testing, suggesting that the present imaging technique can be performed quite safely.
In conclusion, 3 T MRI after intratympanic injection of GBCA will contribute to improved diagnosis and understanding of the pathological condition in patients with MD.
Acknowledgments
We thank A.C. Apple-Mathews for help in preparing the manuscript. This study was supported by a Health and Labour Sciences Research Grant for Comprehensive Research on Disability Health and Welfare from the Ministry of Health, Labour and Welfare of Japan, by the Acute Profound Deafness Research Committee of the Ministry of Health, Labour and Welfare of Japan, and by a Health and Labour Sciences Research Grant for Research on Specific Diseases (Vestibular Disorders) from the Japanese Ministry of Health, Labour and Welfare.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Sajjadi H, Paparella MM. Meniere's disease. Lancet 2008;372:406–14.
- Nakashima T, Naganawa S, Sugiura M, Teranishi M, Sone M, Hayashi H, Visualization of endolymphatic hydrops in patients with Meniere's disease. Laryngoscope 2007;117:415–20.
- Naganawa S, Satake H, Kawamura M, Fukatsu H, Sone M, Nakashima T. Separate visualization of endolymphatic space, perilymphatic space and bone by a single pulse sequence; 3D-inversion recovery imaging utilizing real reconstruction after intratympanic Gd-DTPA administration at 3 Tesla. Eur Radiol 2008;18:920–4.
- Naganawa S, Satake H, Iwano S, Fukatsu H, Sone M, Nakashima T. Imaging endolympatic hydrops at 3 Tesla using 3D-FLAIR with intratympanic Gd-DTPA administration. Magn Reson Med Sci 2008;7:85–91.
- Fukuoka H, Tsukada K, Miyagawa M, Oguchi T, Takumi Y, Sugiura M, Semi-quantitative evaluation of endolymphatic hydrops by bilateral intratympanic gadolinium-based contrast agent (GBCA) administration with MRI for Meniere's disease. Acta Otolaryngol 2010;130:10–16.
- Kimura H, Aso S, Watanabe Y. Prediction of progression from atypical to definite Meniere's disease using electrocochleography and glycerol and furosemide tests. Acta Otolaryngol 2003;123:388–95.
- Ito M, Watanabe Y, Shojaku H, Kobayashi H, Aso S, Mizukoshi K. Furosemide VOR test for the detection of endolymphatic hydrops. Acta Otolaryngol Suppl 1993;504:55–7.
- Taguchi D, Kakigi A, Takeda T, Sawada S, Nakatani H. Diagnostic value of plasma antidiuretic hormone, electrocochleography, and glycerol test in patients with endolymphatic hydrops. ORL J Otorhinolaryngol Relat Spec 2009;71(Suppl 1):26–9.
- Miyagawa M, Fukuoka H, Tsukada K, Oguchi T, Takumi Y, Sugiura M, Endolymphatic hydrops and therapeutic effects are visualized in ‘atypical’ Meniere's disease. Acta Otolaryngol 2009;129:1326–9.