Abstract
Purpose: The aim of this study was to evaluate the effects of hyperbaric oxygen therapy (HBO) on the enhancement of hyperthermic chemosensitisation to carboplatin at mild temperatures in experimental tumours. Methods: SCCVII carcinoma in C3H/He mice was used to assess tumour growth delay. The mice received intraperitoneal injections of carboplatin. For HBO treatment, the mice were exposed to HBO at 2.0 atmospheres of absolute oxygen for 60 min. For mild hyperthermia (HT), treatment at 41.5 °C for 30 min was performed. The tumour tissue pO2 levels were measured with a digital pO2 monitor during and immediately after treatment. Results: The average time taken to reach a threefold relative tumour size was significantly longer after treatment with carboplatin combined with mild HT and HBO than after treatment with carboplatin and mild HT. The relative sizes of the tumours after the combined treatment were smallest when the treatment sequence was carboplatin, mild HT, and HBO. The tumour tissue pO2 values were significantly higher immediately after mild HT followed by HBO than immediately after HBO followed by mild HT. The tumour tissue pO2 levels during mild HT and HBO generally increased, although the patterns of the increases varied. Conclusion: The administration of HBO increased the effects of hyperthermic chemosensitisation to carboplatin at mild temperatures on experimental tumours, particularly when given in the sequence of carboplatin, mild HT, and HBO, a finding that supports previous clinical outcomes for a novel combined therapy using carboplatin plus HT and HBO.
Introduction
Hyperthermia (HT) as a treatment for cancer is known to cause direct cytotoxicity and acts as a radiation sensitiser and chemosensitiser [Citation1,Citation2]. The mechanisms of action of HT are thought to involve increased drug uptake into cells, increased oxygen radical production, increased DNA damage, and inhibition of DNA repair [Citation1]. In particular, HT administered at mild temperatures of 39–42 °C (mild HT) has been shown to improve tumour oxygenation in human tumours [Citation3]. Hyperthermia-induced cytotoxicity and radio-sensitising effects are expected to be significant when the tumour temperature is elevated to at least 42–43 °C [Citation4]. Unfortunately, it is often impossible to uniformly raise the temperature of deep-seated tumours to 42–43 °C using currently available HT devices. However, it is relatively easy to raise the temperature of deep-seated tumours to the range of mild HT (39–42 °C), which is a range that can improve tumour oxygenation for up to 1–2 days by increasing tumour blood flow [Citation4]. HT enhances the cytotoxic effects of many chemotherapeutic drugs, and platinum compounds are the most heat interactive of all chemotherapeutic drugs [Citation2,Citation5–11]. Many previous in vitro/in vivo studies of carboplatin have confirmed synergism with HT at mild temperatures [Citation12,Citation13].
On the other hand, tumour oxygenation can be achieved by hyperbaric oxygen therapy (HBO), which is safe when current standard treatment protocols are followed [Citation14–16]. A few experimental studies have compared the synergism of anticancer effects between carboplatin and HBO [Citation17,Citation18]. In this context, we hypothesised that HBO increased the effects of mild temperature HT-induced chemosensitisation. Previously we conducted a preliminary clinical study to investigate a novel combination regimen consisting of chemotherapy using paclitaxel and carboplatin plus regional HT and HBO to improve the clinical outcomes of patients with non-small cell lung cancer and multiple pulmonary metastases [Citation19]. The results of our initial clinical experience were promising [Citation19]. However, to our knowledge, no experimental studies have assessed the efficacy of the combination of HBO and mild HT for improving the anti-tumour effects of chemotherapy. Therefore, we evaluated the effect of HBO on enhancement of mild temperature HT-induced chemosensitisation to carboplatin in experimental tumours and compared the efficacy of different sequences of combination therapy.
Materials and methods
Tumours and animals
SCCVII carcinomas of C3H/He mice were used for the tumour growth delay assay. The SCCVII tumour cells were cultured in Eagle’s minimum essential medium (MEM; Gibco, Grand Island, NY) containing 10% fetal bovine serum (Gibco), penicillin (50 units/mL), and streptomycin (50 mg/mL). Exponentially growing SCCVII tumour cells were collected from monolayer cultures, and a suspension of about 3 × 105 cells was inoculated subcutaneously into the hind legs of 9-week-old syngenic female C3H/He mice (n = 143). Treatment was initiated when the SCCVII tumours reached approximately 12 mm in diameter, which was approximately 14 days after tumour cell inoculation.
The mice were housed separately in a filter-topped cage in a clean barrier facility, fed commercial pellet chow and water ad libitum, and randomised into treatment groups. Each group contained nine mice for evaluation of tumour growth delay and to determine the most effective sequence for the combined treatment. Six mice in each group were used to assess tumour tissue pO2 levels immediately after the treatments. In addition, seven mice in each group were used to measure the tumour tissue pO2 levels during the treatments.
The mice were maintained according to the guidelines set forth in the Guiding Principles for the Care and Use of Animals approved by the Faculty Meeting of the University of Occupational and Environmental Health, Kitakyushu.
Chemotherapy, mild hyperthermia, and hyperbaric oxygen exposure
The mice received intraperitoneal injections of carboplatin (50 mg/kg). A circulating water bath stabilised at 41.5 °C was used to induce HT. The water bath was covered with a plastic box with a hole to allow immersion of the tumour-bearing leg of an unanaesthetised C3H/He mouse in the water, and the tumour was completely immersed in the water bath for 30 min.
Unanaesthetised C3H/He mice were placed into plastic boxes that were put into a hyperbaric chamber specifically designed for mice (HANYUDA, Niigata, Japan). After the chamber was flushed at a rate of 5 L/min for 5 min, the mice were exposed to HBO according to the following schedule: 10 min of compression to 2.0 atmospheres of absolute (ATA) oxygen, 60 min of 100% oxygen inhalation at 2.0 ATA, and 10 min of decompression to normal pressure with oxygen inhalation.
Tumour growth delay assay and tumour tissue pO2
Tumour growth delay was determined by using nine SCCVII tumour-bearing mice from each group. The tumour volume doubling time (Vdt) after treatment and relative sizes of tumours at 4, 7, 10, 14, and 17 days were evaluated and compared among the following five groups: no treatment, carboplatin alone, carboplatin plus mild HT (mild HT immediately after injection of carboplatin), carboplatin plus HBO (HBO immediately after injection of carboplatin), and carboplatin plus mild HT and HBO (mild HT immediately after injection of carboplatin and followed immediately by HBO); these sequences were selected on the basis of the findings of a previous clinical study [Citation19].
In an additional study, the relative sizes of the tumours and Vdt values were evaluated among the following six groups to determine the most effective sequence for the combined treatment of carboplatin plus mild HT and HBO: mild HT immediately after injection of carboplatin and immediately followed by HBO, HBO immediately after injection of carboplatin and immediately followed by mild HT, injection of carboplatin immediately after HBO and immediately followed by mild HT, mild HT immediately after HBO and immediately followed by injection of carboplatin, injection of carboplatin immediately after mild HT and immediately followed by HBO, and HBO immediately after mild HT and immediately followed by injection of carboplatin. Each group contained nine mice.
Tumour volume was calculated from the measured values of length (l), width (w), and height (h). Corrections for the ellipsoidal shape of a tumour were made by using the formula: l × w × h × π/6. The Vdt was calculated by assuming an exponential pattern of tumour growth. During the combined treatment consisting of carboplatin plus mild HT and HBO, the tumour tissue pO2 values were measured with a pO2 sensor (POG-203, Unique Medical, Tokyo, Japan).
A sensor was inserted into the centre of the tumour, and the tissue pO2 was measured by using the digital pO2 monitor during the sequence carboplatin, mild HT, and HBO in seven mice, and during the sequence carboplatin, HBO, and mild HT in seven mice. The tumour tissue pO2 values immediately after mild HT, HBO, and HBO followed by mild HT or HT followed by HBO were also determined along five longitudinal tracks within each tumour, and each group contained six mice. The same sensor was used for the pO2 measurements made with single real-time tracings.
Statistical analysis
The Vdt values after treatment and relative sizes of tumours at 4, 7, 10, 14, and 17 days were evaluated and compared among the treatment groups with unpaired t-tests. The average time to reach a threefold relative tumour size was investigated among the treatment groups with the Mann–Whitney U test. The relative sizes of the tumours 12 days after combined treatment using all six sequences of carboplatin plus mild HT and HBO were compared with an unpaired t-test. The tumour tissue pO2 values immediately after each treatment were analysed with the Mann–Whitney U test.
Results
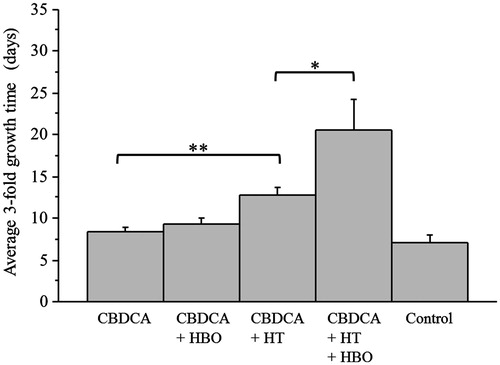
shows the tumour growth delay curves of the SCCVII tumours from the various groups. The relative tumour sizes after the combined treatment of carboplatin plus mild HT and HBO were significantly smaller than those after carboplatin plus mild HT at 7, 10, and 14 days after treatment. The relative tumour sizes after carboplatin plus mild HT were significantly smaller than those after carboplatin alone at 7, 10, and 17 days after treatment. There were no significant differences in the relative sizes of tumours among the groups that received carboplatin plus HBO and those that received carboplatin alone. The median Vdt was significantly longer for the mice that received the combined treatment of carboplatin plus mild HT and HBO (12.4 days) than for those of the groups that received carboplatin plus mild HT (8.3 days), carboplatin plus HBO (5.8 days), carboplatin alone (5.5 days), or no treatment (4.9 days). shows the average time to reach a threefold relative tumour size in each group; there were significant differences between the group that received carboplatin plus mild HT and HBO and the group that received carboplatin plus mild HT, and significant differences between the group that received carboplatin plus mild HT and the group that received carboplatin alone.
Figure 1. Tumour growth curves of the SCCVII tumours. The relative sizes of the tumours were significantly smaller for the combination of carboplatin plus mild HT and HBO than those for the combination of carboplatin plus mild HT at 7, 10, and 14 days after treatment. In addition, the relative tumour sizes were significantly smaller for treatment with carboplatin plus HT than with carboplatin alone at 7, 10, and 17 days after treatment. Medium dashed line, control; medium dotted line, carboplatin; dashed line, carboplatin + HBO; medium dashed dotted line, carboplatin + HT; medium line, carboplatin + HT + HBO. *p < 0.0001, **p < 0.001, ***p < 0.01, ****p < 0.05.
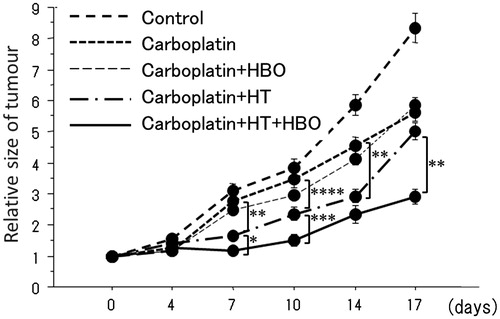
Figure 2. The average time to reach a threefold relative tumour size in each group. The average time to reach a threefold relative tumour size was significantly longer after the combined treatment consisting of carboplatin plus mild HT and HBO than after the combined treatment of carboplatin plus mild HT. In addition, the values were significantly longer after treatment with carboplatin plus HT than after treatment with carboplatin alone. *p < 0.05, **p < 0.01.
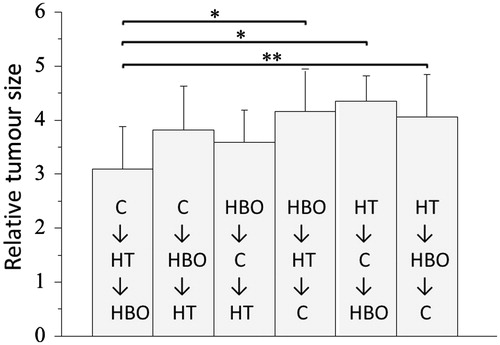
presents the results for the different sequences of combined treatment consisting of carboplatin plus mild HT and HBO. The relative size of the tumour at 12 days after treatment was smallest in the group that received the sequence carboplatin, mild HT, and HBO (). The following median Vdt values were determined for the groups treated in the various sequences: 9.3 days for carboplatin, mild HT and HBO, 8.6 days for HBO, carboplatin and mild HT, 8.0 days for carboplatin, HBO and mild HT, 7.3 days for mild HT, carboplatin and HBO, 7.0 days for mild HT, HBO and carboplatin, and 6.8 days for HBO, mild HT and carboplatin.
Figure 3. Among the different sequence schedules of the combined treatment consisting of carboplatin plus mild HT and HBO, the relative tumour size 12 days after starting the treatment was smaller for the sequence of carboplatin, mild HT and HBO than for any other sequence. C, carboplatin; HT, hyperthermia; HBO, hyperbaric oxygen. *p < 0.01, **p < 0.05.
The tumour tissue pO2 values measured immediately after treatment with mild HT, HBO, HBO followed by mild HT, or mild HT followed by HBO are shown in . The tumour tissue pO2 values immediately after the treatments significantly increased relative to those in the control group (). The tumour tissue pO2 values immediately after treatment with mild HT followed by HBO were also significantly higher than those immediately after HBO followed by mild HT (). shows the temporal changes in the tumour tissue pO2 levels in the mice with SCCVII tumours treated with the sequence of carboplatin, mild HT and HBO (seven representative mice, ) and the sequence of carboplatin, HBO and mild HT (seven representative mice, ). The tumour tissue pO2 levels during the combined therapy generally increased, although the patterns of the increases varied.
Figure 4. Histograms of the tumour tissue pO2 values immediately after mild HT, HBO, mild HT followed by HBO, or HBO followed by mild HT. Each group consisted of six mice. Each group shows individual tumours in which five parallel tracks were used to measure the different points. The total number of points used to create the histogram (n) is represented.
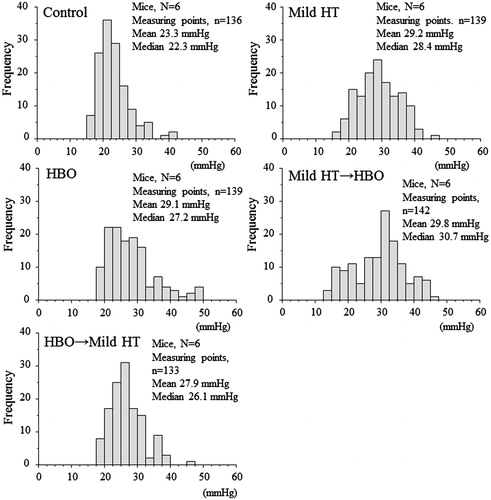
Figure 5. The tumour tissue pO2 levels during the combined treatment consisting of carboplatin plus mild HT and HBO. Shown are the pO2 levels in the sequence of carboplatin, mild HT and HBO in seven representative mice (n = 7) (A) and in the sequence of carboplatin, HBO and mild HT in seven representative mice (n = 7) (B).
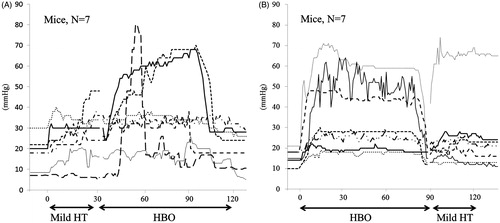
Table 1. The differences in the tumour tissue pO2 values immediately after the treatments among each group.
Discussion
This is the first study to assess the effects of HBO on enhancement of mild temperature HT-induced chemosensitisation to carboplatin in experimental tumours. The results demonstrate that HBO increases the effects of hyperthermic chemosensitisation. In our previous study a novel combination chemotherapy using carboplatin and paclitaxel plus regional HT and HBO was administered to try to improve the clinical outcomes of non-small cell lung cancer patients with multiple pulmonary metastases, and the combined therapy appeared to be a feasible and promising treatment. Both the haematological and non-haematological toxicities were mild, and 12 (75%) of 17 patients had an objective response [Citation19]. The current experimental results support the efficacy of novel combination therapy using carboplatin plus regional HT and HBO.
The thermal enhancement ratios for carboplatin’s cytotoxicity increased with temperature (2.3 at 40.5 °C, 3.2 at 41.8 °C) in vitro, and thermal enhancement of carboplatin in vivo has also been confirmed [Citation20–22]. HBO has been shown to overcome hypoxia in experiments involving administration of 100% oxygen at higher than normal atmospheric pressure. The pO2 in tumour tissue has been shown to increase significantly during HBO exposure [Citation15,Citation16]. The use of HBO in clinical practice is considered to be safe, and complications are rare if the current standard treatment protocols are followed [Citation14]. HBO exposure in combination with weekly administration of cisplatin significantly reduced the tumour volume in a human ovarian cancer xenograft model [Citation23]. Kawasoe et al. reported that HBO plus carboplatin exhibited significant synergism in the suppression of cell proliferation for highly metastatic murine osteosarcoma cell lines, and in vivo, concomitant HBO also enhanced the chemotherapeutic effects of carboplatin on both tumour growth and lung metastasis in osteosarcoma-bearing mice [Citation17]. In the current study, a significant delay was observed in tumour growth in the mice treated with carboplatin plus mild HT relative to that in the mice treated with carboplatin alone. Although a significant delay in tumour growth in the mice treated with carboplatin plus HBO relative to that in the mice treated with carboplatin alone was not seen, tumour growth was significantly delayed in those treated with the sequence carboplatin, mild HT and HBO relative to that in the mice treated with carboplatin plus mild HT.
Many cytotoxic agents (i.e. bleomycin, procarbazine, streptonigrin, actinomycin D, vincristine) show a positive relationship between oxygen tension and efficacy in cell culture, whereas mitomycin C and adriamycin exhibit higher efficacy under conditions of hypoxia [Citation24]. Some studies have suggested that the cytotoxic effects of carboplatin are altered by hypoxia [Citation25,Citation26]. For example, Koch et al. reported that carboplatin was less effective in germ cell tumour lines under hypoxic conditions [Citation26]. Griffin et al. demonstrated that mild HT followed by carbogen (95% O2, 5% CO2) inhalation further increased tumour pO2 levels and increased radiation-induced cytotoxicity for FSaII tumours grown in C3H mice [Citation27]. In the current study, the tumour pO2 values generally increased under mild HT and HBO. We speculate that tumour oxygenation played an important role in the observed positive results.
Other groups have shown that tumour oxygenation is achieved under the condition of mild HT, although the tumour pO2 levels are variable depending on the measuring point in each tumour [Citation3,Citation27]. The current study also confirms that the tumour pO2 levels at substantial measuring points increased during HBO as well as mild HT, whereas some findings obtained at different measuring points did not change. In addition, the tumour pO2 levels determined immediately after the combined treatment with mild HT followed by HBO were significantly higher than those seen immediately after HBO followed by mild HT. These results suggest a correlation between increased tumour pO2 level and the treatment response after combined treatment.
In summary, this is the first study to assess the effects of HBO on enhancement of mild temperature HT-induced chemosensitisation to carboplatin. The delay in tumour growth was significantly greater following treatment with carboplatin plus mild HT and HBO than following treatment with carboplatin plus mild HT. Therefore, HBO increased the effects of mild temperature HT-induced chemosensitisation to carboplatin, particularly when administered in the sequence of carboplatin, mild HT, HBO. These findings suggest that improved clinical outcomes can be achieved for treatment with this novel combined therapy consisting of carboplatin plus regional HT and HBO in patients with non-small cell lung cancer.
Acknowledgements
The authors thank Toshiyuki Norimura, Hiroyo Kakihara, and Ochi Rumiko, Department of Radiation Biology and Health, and Seung Dae Moon, Department of Radiology, University of Occupational and Environmental Health for their technical support, and Kiyotaka Kohshi, Department of Hyperbaric Medicine and Emergency Medicine, University Hospital of the Ryukyus for advice and scientific discussion.
Declaration of interest
This work was supported by the Japan Society for the Promotion of Science (JSPS KAKENHI 20790915). The authors alone are responsible for the content and writing of the paper.
References
- Jones EL, Samulski TV, Leonard RP, Dewhirst MW. Hyperthermia, 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins, 2003
- Moyer HR, Delman KA. The role of hyperthermia in optimizing tumor response to regional therapy. Int J Hyperthermia 2008;24:251–61
- Song CW, Shakil A, Osborn JL, Iwata K. Tumour oxygenation is increased by hyperthermia at mild temperatures. Int J Hyperthermia 1996;12:367–73
- Song CW, Park H, Griffin RJ. Improvement of tumor oxygenation by mild hyperthermia. Radiat Res 2001;155:515–28
- Zhao C, Dai C, Chen X. Whole-body hyperthermia combined with hyperthermic intraperitoneal chemotherapy for the treatment of stage IV advanced gastric cancer. Int J Hyperthermia 2012;28:735–41
- Huang T, Gong W, Li X, Zou C, Jiang G, Feng D. Enhancement of osteosarcoma cell sensitivity to cisplatin using paclitaxel in the presence of hyperthermia. Int J Hyperthermia 2013;29:248–55
- Heijkoop ST, van Doorn HC, Stalpers LJ, Boere IA, van der Velden J, Franckena M, et al. Results of concurrent chemotherapy and hyperthermia in patients with recurrent cervical cancer after previous chemoradiation. Int J Hyperthermia 2014;30:6–10
- Tschoep-Lechner KE, Milani V, Berger F, Dieterle N, Abdel-Rahman S, Salat C, et al. Gemcitabine and cisplatin combined with regional hyperthermia as second-line treatment in patients with gemcitabine-refractory advanced pancreatic cancer. Int J Hyperthermia 2013;29:8–16
- Yarema RR, Ohorchak MA, Zubarev GP, Mylyan YP, Oliynyk YY, Zubarev MG, et al. Hyperthermic intraperitoneal chemoperfusion in combined treatment of locally advanced and disseminated gastric cancer: Results of a single-centre retrospective study. Int J Hyperthermia 2014;30:159–65
- Sousa A, Inman BA, Pineiro I, Monserrat V, Perez A, Aparici V, et al. A clinical trial of neoadjuvant hyperthermic intravesical chemotherapy (HIVEC) for treating intermediate and high-risk non-muscle invasive bladder cancer. Int J Hyperthermia 2014;30:166–70
- Inman BA, Stauffer PR, Craciunescu OA, Maccarini PF, Dewhirst MW, Vujaskovic Z. A pilot clinical trial of intravesical mitomycin-C and external deep pelvic hyperthermia for non-muscle-invasive bladder cancer. Int J Hyperthermia 2014;30:171–5
- Xu MJ, Alberts DS. Potentiation of platinum analogue cytotoxicity by hyperthermia. Cancer Chemother Pharmacol 1988;21:191–6
- Herman TS, Teicher BA, Chan V, Collins LS, Abrams MJ. Effect of heat on the cytotoxicity and interaction with DNA of a series of platinum complexes. Int J Radiat Oncol Biol Phys 1989;16:443–9
- Moen I, Stuhr LE. Hyperbaric oxygen therapy and cancer – a review. Target Oncol 2012;7:233–42
- Brizel DM, Lin S, Johnson JL, Brooks J, Dewhirst MW, Piantadosi CA. The mechanisms by which hyperbaric oxygen and carbogen improve tumour oxygenation. Br J Cancer 1995;72:1120–4
- Kinoshita Y, Kohshi K, Kunugita N, Tosaki T, Yokota A. Preservation of tumour oxygen after hyperbaric oxygenation monitored by magnetic resonance imaging. Br J Cancer 2000;82:88–92
- Kawasoe Y, Yokouchi M, Ueno Y, Iwaya H, Yoshida H, Komiya S. Hyperbaric oxygen as a chemotherapy adjuvant in the treatment of osteosarcoma. Oncol Rep 2009;22:1045–50
- Suzuki Y, Tanaka K, Neghishi D, Shimizu M, Murayama N, Hashimoto T, et al. Increased distribution of carboplatin, an anti-cancer agent, to rat brains with the aid of hyperbaric oxygenation. Xenobiotica 2008;38:1471–5
- Ohguri T, Imada H, Narisada H, Yahara K, Morioka T, Nakano K, et al. Systemic chemotherapy using paclitaxel and carboplatin plus regional hyperthermia and hyperbaric oxygen treatment for non-small cell lung cancer with multiple pulmonary metastases: Preliminary results. Int J Hyperthermia 2009;25:160–7
- Cohen JD, Robins HI, Schmitt CL. Tumoricidal interactions of hyperthermia with carboplatin, cisplatin and etoposide. Cancer Lett 1989;44:205–10
- Ohno S, Siddik ZH, Baba H, Stephens LC, Strebel FR, Wondergem J, et al. Effect of carboplatin combined with whole body hyperthermia on normal tissue and tumor in rats. Cancer Res 1991;51:2994–3000
- Sakaguchi Y, Makino M, Kaneko T, Stephens LC, Strebel FR, Danhauser LL, et al. Therapeutic efficacy of long duration-low temperature whole body hyperthermia when combined with tumor necrosis factor and carboplatin in rats. Cancer Res 1994;54:2223–7
- Selvendiran K, Kuppusamy ML, Ahmed S, Bratasz A, Meenakshisundaram G, Rivera BK, et al. Oxygenation inhibits ovarian tumor growth by downregulating STAT3 and cyclin-D1 expressions. Cancer Biol Ther 2010;10:386–90
- Teicher BA, Lazo JS, Sartorelli AC. Classification of antineoplastic agents by their selective toxicities toward oxygenated and hypoxic tumor cells. Cancer Res 1981;41:73–81
- Donnelly ET, Kelley M, Rockwell S. Effects of RSR13 and oxygen on the cytotoxicity of cisplatin and carboplatin to EMT6 mouse mammary tumor cells in vitro and in vivo. Cancer Chemother Pharmacol 2004;53:43–50
- Koch S, Mayer F, Honecker F, Schittenhelm M, Bokemeyer C. Efficacy of cytotoxic agents used in the treatment of testicular germ cell tumours under normoxic and hypoxic conditions in vitro. Br J Cancer 2003;89:2133–9
- Griffin RJ, Okajima K, Barrios B, Song CW. Mild temperature hyperthermia combined with carbogen breathing increases tumor partial pressure of oxygen (pO2) and radiosensitivity. Cancer Res 1996;56:5590–3
