Abstract
Background. Ear, nose, and throat (ENT) problems are common in childhood and are important reasons to visit the general practitioner. Objective. To examine trends in incidence rates, antibiotic prescribing, and referrals of five common ENT problems in children. Design. Netherlands Information Network of General Practice (LINH), a nationally representative general practice database. Setting. A total of 50 000 children, aged 0–17 years, registered in Dutch general practice over the period 2002–2008. Methods. Incidence rates were calculated and trends were analysed using linear regression analysis, with incidence rates per age group, proportion treated with antibiotics, and referrals as dependent variables and year of observation as independent variable. Results. In general, incidence rates of acute otitis media, serous otitis, sinusitis, tonsillitis, and tonsil hypertrophy remained stable over the period 2002–2008. An increasing trend was observed for serous otitis media in children aged 0–4 years (RR = 1.04, p < 0.001). A decreasing trend was observed for sinusitis in children aged 5–11 and for tonsillitis in children aged 11–17 years (RR 0.99, p < 0.001 and RR 0.94, p < 0.001, respectively). Antibiotics were prescribed in 10–60% of the diagnoses. An increasing trend for antibiotic prescription was found for acute otitis media (beta = 0.07, p < 0.001), mainly on account of amoxicillin. Although antibiotic treatment of tonsillitis remained stable, pheneticillin prescriptions showed a downward trend (beta = −0.10, p < 0.001). First-choice antibiotics were prescribed in >80% of cases. Conclusions. This study showed remarkably stable trends in incidence rates, antibiotic prescribing, and referrals of common ENT problems. The low proportion of antibiotic treatment in ENT problems did not show negative consequences.
Otitis media, glue ear, sinusitis, and tonsillitis are common in childhood. Decreasing consultation rates in general practice have been reported in many countries.
In Dutch primary care, most incidence rates for ENT problems in children remained stable over the period 2002–2008.
Antibiotic prescribing and referrals to a specialist for ENT problems in children in the Netherlands were relatively low. This did not show negative consequences.
Ear, nose, and throat problems such as otitis media, serous otitis media, sinusitis, and tonsillitis are common in childhood and important reasons for parents and children to visit the general practitioner (GP) [Citation1]. In the Netherlands cough, sore throat, and earache together account for nearly 25% of consultations with children in general practice [Citation2–4]. Treatment options for ENT problems in general practice include watchful waiting, medication for symptomatic relief, and antibiotics or referral.
For planning of health services and guideline development, recent data on incidence, antibiotic use, and referrals are important. Few studies have examined incidence rates of ENT problems in children in general practice over time [Citation5]. In some countries a decreasing trend in GP consultations for respiratory symptoms and ENT problems was found [Citation1,Citation5].
In the last 10 years the Dutch College of General Practitioners has published several evidence-based guidelines for the management of ENT problems, i.e. for acute otitis media [Citation6], serous otitis media [Citation7], sinusitis [Citation8], tonsillitis, and tonsil hypertrophy [Citation9]. These guidelines might have changed GPs’ management. Most guidelines are cautious about recommending antibiotics; however, when antibiotics are still needed, small-spectrum penicillin is advised for tonsillitis, tetracycline or broad-spectrum penicillin for sinusitis, and a broad-spectrum penicillin for acute otitis media. No antibiotics are advised for serous otitis media and tonsil hypertrophy. In Europe and the US, GPs were encouraged to reduce their prescribing of antibiotics [Citation10–12]. In the few studies available, the trend for prescribing antibiotics for ENT problems showed a decrease or a stabilization [Citation1,Citation5]. However, a drawback of these studies is that the prescription rates were calculated for all respiratory symptoms together and not specified by diagnosis.
When children are referred to specialized care it is generally for ENT problems [Citation4]. In the Netherlands the GP acts as a gatekeeper for specialized care. In the Netherlands, compared with 1987, in 2001 the population-based referral rate for acute otitis media decreased from 6.9 to 1.9 [Citation13]. Information on trends in referring children to a specialist is scarce. Moreover, study populations were either small or restricted to referrals to a single outpatient clinic [Citation14,Citation15]. The present study explores trends over the years 2002–2008 in incidence rates, antibiotic prescribing, and referral to a medical specialist of five common ENT problems.
Material and methods
We derived data from electronic medical records of Dutch general practices participating in the Netherlands Information Network of General Practice (LINH) [Citation16,Citation17]. During the seven-year registration period (2002–2008), 135 general practices throughout the Netherlands participated. In the Netherlands, general practices have a fixed patient list; all inhabitants are listed in a general practice, and GPs have a gate-keeping role for specialized care. The patients enlisted in the participating practices are comparable to the general Dutch population with respect to age, gender, and type of healthcare insurance [Citation16].
Data on all physician–patient contacts, prescriptions, and referrals during the study period were extracted from the electronic medical records of all children aged 0–17 years listed in the participating practices. Diagnoses were coded by the GP using the International Classification of Primary Care (ICPC) [Citation18]. Several validity studies were carried out, e.g. vignette studies and other studies addressing completeness and validity of ICPC coding. Over the seven years the number of participating practices ranged from 71 to 86. The included practices are considered representative of all Dutch practices regarding urbanization, gender, age, and region. Single-handed practices are slightly underrepresented [Citation19].
Study population
The total number of children in the participating practices ranged from 53 137 to 62 862 per observation year. Over the seven years, the percentage of boys was around 51%; the percentage of children aged 0–4, 5–11, and 12–17 years was around 28%, 33%, and 39%, respectively.
Outcomes
The first outcome measure was the annual incidence rate of acute otitis media (ICPC code H71), serous otitis media (H72), sinusitis (R75), tonsillitis (R76), and tonsil hypertrophy (R90).
Incident cases were defined as patients with at least 30 days without GP practice attendance for the same problem before the current consultation with this diagnosis. For the diagnoses serous otitis media and tonsil hypertrophy we used a period of 90 days. The second outcome measure was the proportion of cases in which oral antibiotics were prescribed in the first consultation for each of the five diagnoses under study. The third outcome measure was the proportion of cases referred in the first consultation to an otorhinolaryngologist or pediatrician.
Statistical analysis
We calculated incidence rates per 1000 children per year using the annual mid-time population size as denominator and the number of incident cases as numerator. Trends were analysed by Poisson linear regression analysis using the incidence per age group as the dependent variable and the years as independent variable. This allows the change to be expressed in relative risk (RR) per year (significance level p = 0.05). We corrected for multiple testing with the step-down Bonferroni method.
Percentages prescribed antibiotics and referrals were calculated using the incident cases as denominator, and the number of antibiotic prescriptions and referrals, respectively, as numerator. Trends were analysed by linear regression analysis using number of antibiotics or referrals as the dependent variable and the years as independent variable. We report beta values with significance level set at p < 0.05.
Results
Incidence rates
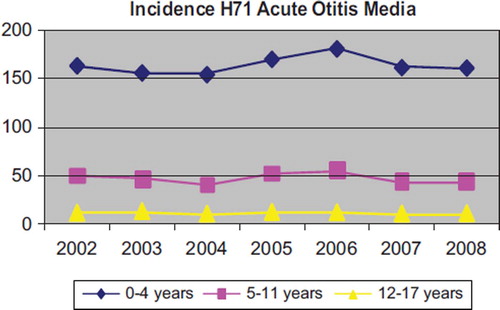
The incidence rates ranged from about two per 1000 for sinusitis in children 0–4 years of age to about 25 per 1000 for serous otitis, tonsillitis, and tonsil hypertrophy and 150 per 1000 for acute otitis media in the same age group. As an example, shows the trend in incidence rates of acute otitis media presented in general practice over the years 2002–2008 (All figures available online as supplementary files). Most incidence rates remained stable, with three exceptions. An increasing trend was found for serous otitis media in children aged 0–4 years old with a relative risk (RR) of 1.04 (p < 0.001). Decreasing incidence rates were found for sinusitis in children aged 5–11 years (RR = 0.95, p = 0.001) and for tonsillitis in children aged 11–17 years (RR = 0.94, p < 0.001).
Antibiotic prescriptions
For sinusitis and tonsillitis the percentage of antibiotic prescribing in the first consultation was nearly 60%. The antibiotic prescribing rate for acute otitis media was nearly 50%, followed by tonsil hypertrophy at 20% and serous otitis media at 9%. shows in what proportion of the incident cases of otitis media oral antibiotics were prescribed during the first consultation over the period 2002–2008.
Figure 2. Percentage of antibiotic prescriptions in children with acute otitis media (H71) for 2002–2008.
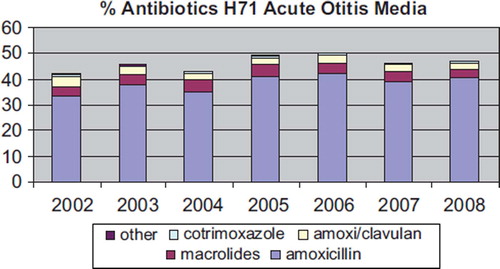
Over the whole period, in children with acute otitis media, amoxicillin was most often prescribed (in about 80% of antibiotic prescriptions). Macrolides were prescribed in 10% of antibiotic prescriptions. Children below the age of two years received antibiotics more often than older children (53% vs. 44%), which was mainly in the form of amoxicillin (45% vs. 36%), p < 0.001.
For children with sinusitis the antibiotics of first choice (doxycycline and amoxicillin) were prescribed in 38% and 43% of the prescriptions, respectively. Macrolides followed in 13% of the prescriptions. Of all doxycycline prescriptions 97% were prescribed to children above 11 years of age, and 99% were aged 10 years or older. For children with tonsillitis, pheneticillin, the antibiotic of first choice, was prescribed in 63% of the prescriptions in the first consultation. For this diagnosis, amoxicillin was prescribed in 22% and macrolides in 8% of the antibiotic prescriptions.
For each diagnosis the change in antibiotic prescribing (beta) over the consecutive years was calculated. For serous otitis media, sinusitis, and tonsil hypertrophy no significant change was found. For acute otitis media an increase was seen, i.e. an increase in antibiotic prescriptions in general, with a beta of 0.03 (p < 0.001). Of this increase in antibiotic prescriptions, most were accounted for by amoxicillin (beta = 0.07, p < 0.001). For tonsillitis the change in all antibiotics over the subsequent years was not significant; however, the percentage of the antibiotic of first choice, pheneticillin, decreased with a beta of −0.10 (p < 0.001).
Referral to otorhinolaryngologist or pediatrician
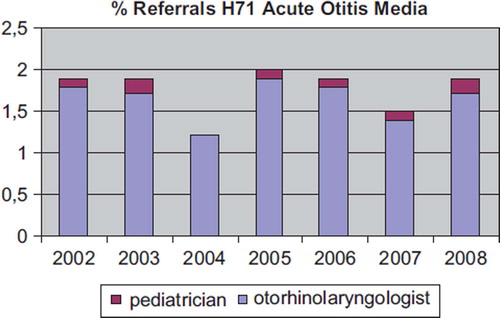
The proportion of incident cases referred by the GP ranged from 1% for sinusitis to 30% for tonsil hypertrophy. shows the seven-year trend for acute otitis media. The GPs most often referred young children aged 0–4 years with acute otitis media, serous otitis, and tonsil hypertrophy. None of the diagnoses showed a significant trend in referrals over the seven-year period.
Discussion
In this large study population the incidence rates of acute otitis media, serous otitis media, sinusitis, tonsillitis, and tonsil hypertrophy in children were remarkably stable over the years 2002–2008. An increasing incidence rate was found only for serous otitis media in children aged 0–4 years, and a decreasing incidence was found for sinusitis and tonsillitis in children aged 5–11 years and 12–17 years, respectively. Prescription of antibiotics for the five diagnosis groups also remained stable and relatively low with 10–60% prescriptions in incident cases. Exceptions were increasing antibiotic prescription for acute otitis media and a decrease in pheneticillin for tonsillitis, mostly on account of amoxicillin. Stable trends were also found for referrals to an otorhinolaryngologist or pediatrician.
Strengths and limitations
The major strength of this study is the use of unique data over a seven-year period from a large national network of practices. The study population allowed calculation of incidence rates for five ENT diseases [Citation16]. In the present study we chose to use only the first contact of an episode. In this way the GP's management will not have been affected by a previous contact in the same episode.
Single-handed practices were somewhat underrepresented; however, because this item is not related to our study outcomes it is not considered an important limitation. The results can be assumed to represent regular primary care and consultation behaviour in the Netherlands. The data were based on the diagnoses as made by the GPs during routine care. No criteria were imposed other than adhering to ICPC coding guidelines. We, for example, do not have data as to whether the GP used a Strep-A test in making the diagnosis of tonsillitis. Tympanometry is not commonly used in Dutch general practice.
Comparison with other studies
Over the past 10 years decreasing consultation rates for ENT problems in general practice have been reported in Europe and the US [Citation1,Citation5,Citation20–22], which might reflect a decrease in ‘real’ incidence in the general population. However, the present study does not confirm a considerable decline in ENT problems during 2002–2008.
The question arises as to how reliable the methods used to compare data have been in the past. In the present study we used the same method throughout the seven-year period. A comparative study among 26 European countries showed that Dutch GPs prescribe the lowest amount of antibiotics in children [Citation23]. In the present study, the percentage of antibiotic prescriptions is relatively low: 50% in acute otitis media, and 60% in sinusitis and tonsillitis. Guidelines vary across Western European countries. For example, a Finnish guideline recommends treating acute otitis media primarily with antibiotics in all children [Citation24]. In contrast, the Dutch guideline recommends prescribing antibiotics in selected cases of acute otitis media, i.e. those at risk of complications [Citation6]. The question arises as to whether Dutch GPs under-treat these children. However, because referral rates remained low, in our opinion these low antibiotic prescription rates do not indicate under-treatment. On the other hand, GPs can help reduce overuse of antibiotics for ENT problems in children [Citation10–12]. It seems that there is still room for improvement with regard to prescribing antibiotics.
In the present study, in more than 80% of the cases the GPs prescribed a first-choice antibiotic. Assuming that GPs prescribed macrolides as an alternative to penicillin (in the case of penicillin allergy or intolerance) the percentage of correct antibiotic prescribing would increase to more than 90%. This is a remarkable result in contrast with another study in which GPs prescribed more broad-spectrum antibiotics for inappropriate diagnoses [Citation25]. A disturbing trend is the decline in prescribing small-spectrum penicillins for tonsillitis. In 2005–2007 Dutch guidelines for acute otitis media, tonsillitis, and sinusitis were revised. All adjustments emphasized a reluctance to prescribe antibiotics [Citation6,Citation8,Citation9]. We found no effect of these guideline adjustments. Surprisingly, we found antibiotic prescriptions for serous otitis media and tonsil hypertrophy: 9% and 20%, respectively. These GPs either disregarded the guidelines and incorrectly prescribed antibiotics for these diagnoses or prescribed antibiotics for coexisting morbidity. An antibiotic prescribing rate of more than 60% for tonsillitis is probably not consistent with current guidelines, as we know that less than half of the cases with tonsillitis are due to beta-haemolytic streptococci [Citation26].
For sinusitis, the Dutch guidelines recommend doxycycline only for children above the age of 11, as in other countries [Citation8]. Almost all doxycycline prescriptions were for this age group. Although the vast majority of ENT problems in children presented in general practice are managed by GPs themselves, some require referral. Most referrals to the otorhinolaryngologist concerned an (adeno)tonsillectomy. It is well known that tonsillectomy rates vary considerably between countries [Citation27]. In the present study no significant trends in ENT referrals were found during the period 2002–2008.
In summary, this study showed remarkably stable trends in incidence rates, antibiotic prescribing, and referrals for ENT problems in children in general practice.
Ethical approval
This study was carried out according to Dutch legislation on privacy.
Competing interests
The authors state that there are no competing interests.
Supplementary figures 1–3
Download PDF (227.9 KB)Acknowledgements
The authors thank Sten Willemsen, Department of Biostatistics, Erasmus MC-University Medical Center Rotterdam, for his assistance with the statistical analysis.
References
- Ashworth M, Latinovic R, Charlton J, Cox K, Rowlands G, Gulliford M. Why has antibiotic prescribing for respiratory illness declined in primary care? A longitudinal study using the General Practice Research Database. J Public Health 2004;26:268–74.
- Bruijnzeels MA, Foets M, van der Wouden JC, van den Heuvel JW, Prins A. Everyday symptoms in childhood: Occurrence and general practitioner consultation rates. Br J Gen Pract 1998;48:880–4.
- Otters HB, van der Wouden JC, Schellevis FG, van Suijlekom-Smit LW, Koes BW. Changing morbidity patterns in children in Dutch general practice: 1987–2001. Eur J Gen Pract 2005;11:17–22.
- Van der Linden MW, van Suijlekom-Smit LWA, Schellevis FG, van der Wouden JC. Tweede Nationale Studie naar ziekten en verrichtingen in de huisartspraktijk: het kind in de huisartspraktijk [The child in general practice]. Utrecht, NIVEL; 2005.
- Neumark T, Brudin L, Engstrom S, Molstad S. Trends in number of consultations and antibiotic prescriptions for respiratory tract infections between 1999 and 2005 in primary healthcare in Kalmar County, Southern Sweden. Scand J Prim Health Care 2009;27:18–24.
- Damoiseaux RAMJ, Van Balen FAM, Leenheer WAM, Kolnaar BGM. NHG-Standaard Otitis media acuta [Guideline acute otitis media]. Huisarts Wet 2006;49:615–21.
- Van Balen FAM, Rovers MM, Eekhof JAH, Van Weert HCPM, Eizenga WH, Boomsma LJ. NHG-Standaard Otitis media met effusie [Guideline serous otitis]. Huisarts Wet 2000;43:171–7.
- De Sutter A, Burgers JS, De Bock GH, Dagnelie CF, Labots-Vogelesang SM, Oosterhuis WW, Van der Laan JR, Stalman WAB, De Kleijn MJJ. NHG-Standaard Rhinosinusitis [Guideline rhinosinusitis]. Huisarts Wet 2005;48:615–26.
- Zwart S, Dagnelie CF, Van Staaij BK, Balder FA, Boukes FS, Starreveld JS. NHG-Standaard Acute keelpijn [Guideline acute throat pain]. Huisarts Wet 2007;50:59–68.
- Steinman MA, Yang KY, Byron SC, Maselli JH, Gonzales R. Variation in outpatient antibiotic prescribing in the United States. Am J Manag Care 2009;15:861–8.
- Nyquist AC, Gonzales R, Steiner JF, Sande MA. Antibiotic prescribing for children with colds, upper respiratory tract infections and bronchitis. JAMA 1998;279:875–7.
- Gonzales R, Malone DC, Maselli JH, Sande MA. Excessive antibiotic use for acute respiratory infections in the United States. Clin Infect Dis 2001;33:757–62.
- Otters HB, van der Wouden JC, Schellevis FG, van Suijlekom-Smit LW, Koes BW. Dutch general practitioners’ referral of children to specialists: A comparison between 1987 and 2001. Br J Gen Pract 2004;54:848–52.
- Van den Bosch WJHM, Bor H, van Weel C. Verwijzen van kinderen in vier huisartspraktijken [Referral of children in four general practices]. Huisarts Wet 1992;45:267–71.
- MacFaul R, Long R. Paediatric outpatient utilisation in a district general hospital. Arch Dis Child 1992;67:1068–72.
- Verheij RA, Van Dijk CE, Abrahamse H, . Netherlands Information Network of General Practice: Facts and figures on Dutch GP care. Utrecht/Nijmegen: NIVEL/WOK. Available at: http://www.linh.nl (accessed January 2010).
- Tacken MJAB. Quality of preventive performance in general practice: The use of routinely collected data. PhD dissertation. Nijmegen: Radboud University Nijmegen, the Netherlands; 2005.
- Anonymous. ICPC-2: International Classification of Primary care. Oxford: World Organization of National Colleges, Academies, and Academic Associations of General Practitioners/Family Physicians; 1998.
- Biermans MCJ, Spreeuwenberg P, Verhey RA, . Striking trends in the incidence of health problems in the Netherlands (2002–05). Findings from a new strategy for surveillance in general practice. Eur J Public Health 2009;19:290–6.
- Biermans MCJ, Theuns-Lamers EHM, Spreeuwenberg P, Verheij RA, van der Wouden JC, de Vries Robbé PF, Zielhuis GA. Decreasing incidence of adenotonsillar problems in Dutch general practice: Real or artefact? Br J Gen Pract 2009;59:e368–e375.
- Ashworth M, Charlton J, Ballard K, Latinovic R, Gulliford M. Variations in antibiotic prescribing and consultation rates for acute respiratory infection in UK general practices 1995–2000. Br J Gen Pract 2005;55:603–8.
- McCaig LF, Besser RE, Hughes JM. Trends in antimicrobial prescribing rates for children and adolescents. JAMA 2002;287:3096–102.
- Goossens H, Ferech M, Vander Stichele R, Elseviers M; ESAC Project Group. Outpatient antibiotic use in Europe and association with resistance: A cross-national database study. Lancet 2005;365:579–87.
- Heikkinen T, Huovinen P, Jero J, Pitkäranta A, Renko M, Sumanen M, Heikkilä E. Acute otitis media. Available at: http://www.kaypahoito.fi (accessed 15 December 2010) (in Finnish, with English summary).
- Otters HBM, van der Wouden JC, Schellevis FG, van Suijlekom-Smit LWA, Koes BW. Trends in prescribing antibiotics for children in Dutch general practice. J Antimicrob Chemother 2004;53:361–6.
- Van Staaij BK, Van den Acker EH, De Haas Van Dorsser EH, Vleer A, Hoes AW, Schilder AG. Does the tonsillar surface flora differ in children with and without tonsillar disease? Acta Otolaryngol 2003;123:873–8.
- Van den Acker EH, Hoes AW, Burton MJ, Schilder AG. Large international differences in (adeno)tonsillectomy rates. Clin Otolaryngol Allied Sci 2004;29:161–4.