Abstract
Objectives. To investigate the relationship between the length of a medical consultation in a general practice setting and the biopsychosocial information obtained by the physician, and to explore the characteristics of young physicians obtaining comprehensive, especially psychosocial information. Design. A prospective, longitudinal follow-up study. Setting. Videotaped consultations with standardized patients on two occasions were scored for the amount of biopsychosocial information obtained. Consultation length was recorded in minutes. Subjects. Final-year (T-1) medical school students (n = 111) participated in the project. On completion of their internship one and a half years later (T-2), 62 attended a second time, as young physicians. Main outcome measures. Content lists. Results. Pearson's r correlations between content and length at T-1 and T-2 were 0.27 and 0.66, respectively (non-overlapping confidence intervals). Psychosocial content increased significantly when consultations exceeded 13 minutes (15 minutes scheduled). Physicians using more than 13 minutes had previously, as hospital interns, perceived more stress in the emergency room and had worked in local hospitals. Conclusions. A strong association was found between consultation length and information, especially psychosocial information, obtained by the physicians at internship completion. This finding should be considered by faculty members and organizers of the internship period. Further research is needed to detect when, during the educational process, increased emphasis on communication skills training would be most beneficial for students/residents, and how the medical curriculum and internship period should be designed to optimize young physicians’ use of time in consultations.
The length of a medical consultation can make a difference concerning the information obtained, especially when it comes to psychosocial issues.
For graduating students, a weak significant association occurred between length of consultation and information obtained in a typical GP consultation.
At internship completion, this association was significantly strengthened, especially for psychosocial issues with at least two minutes above mean consultation length.
Those using more time were characterized by having experienced more stress in the emergency room and having worked in local hospitals.
Introduction
Physicians’ understanding of their patients’ biological, psychological, and social situations may be critical for reliable diagnoses and adequate interventions [Citation1,Citation2], as well as allowing patients to disclose their concerns about symptoms, signs, and psychosocial issues [Citation3].
The amount of time a general practitioner (GP) needs to obtain sufficient and necessary information for adequate diagnosis and treatment has been investigated to some extent. In a study of Scottish GPs, Stirling et al. [Citation4] found that an increase in consultation length from nine to 13 minutes resulted in a 32% increase in psychological distress issues disclosed by patients. In a cross-sectional study in six European countries, Deveugele et al. [Citation5] found that consultation length increased from 11 to 12 minutes when disclosed psychosocial problems were acknowledged by the GP. An Australian study of GPs supported the connection between the number of identified problems and consultation duration [Citation6]. In a review, consultations with patients presenting with psychosocial problems were found to take the most time [Citation7].
Our research questions were as follows:
1a. What is the relationship between the amount of information obtained and the length of consultation?
1b. Will this relationship differ between student physicians when ending medical school and the same physicians one and a half years later when completing their internships?
2. Will the amount of psychosocial issues, cancer concerns, and somatic issues addressed depend on the length of the consultations?
3. If so, what characterizes those physicians who spend enough time to obtain a satisfactory amount of information?
On this basis, our main aims were to investigate the association between the duration of the consultation and the information obtained by the physician in a standardized patient's first-time, 15-minute scheduled consultation in a prospective, observational design.
Material and methods
Subjects
Final-year students (n = 320, 65% females, mean age = 27 ± 3 years) from all four Norwegian medical schools were invited to perform a GP-like consultation with a simulated patient. Of the 320 invited, 111 responded (70% females, mean age = 27.8 ± 3 years). At T-2, 78 of the 111 were completing their internships, and of these, 75 agreed to perform a second videotaped consultation. For logistical and geographical reasons, only 62 of the 75 were eligible (random loss). The final sample constituted 69% females, with a mean age of 29.4 ± 3.4 years. [Citation8].
Individual characteristics at T-2
Gender (female = 1, male = 2), age, and type of hospital during internship (regional/central [large] = 0, local [small] = 1), were recorded. Perceived stress in the emergency room was scored from 1 (low pressure) to 5 (high pressure), and actors’ ratings of the opportunities the physicians provided for the patient to “disclose important issues” were measured on a five-point scale (1 = no, 5 = much opportunity).
The simulated patient
At T-1, the “patient” was a 43-year-old woman seeing her GP for the first time, presenting with irregular menstrual bleeding, with psychosocial distress related to a recent divorce and relocation, a stressful job, and fear of uterine cancer, which her mother had died from 10 years earlier.
At T-2, the “patient” was a 43-year-old woman, also seeing her GP for the first time, worried about blood on the toilet paper. Psychosocial stressors were recently moving into the house of her father (a dementia sufferer), having a stressful new job, and a fear of bowel cancer, which her mother had died from 10 years earlier. Although different symptoms, similarity between the cases was intended to minimize patient variation between the two assessments.
Four professional actors played the role of the patient at T-1, four different actors at T-2. The same professional instructor trained actors together on both occasions for optimal standardizing of the role.
The consultation
Participating physicians were instructed to perform a first-time consultation as a trainee GP within 15 minutes. Consultation length was recorded in whole minutes and grouped (based on a normal distribution curve) into short (≤ 10 minutes, n = 16), medium (11–13 minutes, n = 25), and long (> 13 minutes, n = 21). Mean consultation length at T-1 was 14.5 minutes ± 3.1 (range = 8.0–24.0, median = 15.0), and at T-2 was 12.0 ± 3.3 (range = 6–18, median = 12.0). To simplify the characterizing analyses, the time variable was dichotomized by merging the short and medium time groups.
Assessment of the consultation content: outcome variables
At T-1, an instrument for rating the information obtained, comprising 15 dichotomous items, was constructed (). One external rater scored all videos on each item, according to whether the student physician had addressed the specific issue (1) or not (0). A second independent rater scored 16 randomly selected tapes, obtaining very similar mean counts (rater 1: 7.50 ± 2.28, rater 2: 8.06 ± 2.22), which correlated strongly (r = 0.84).
Table I. Correlations between the 15 individual content items and consultation length at T-1.
At T-2, the instrument was expanded to cover a broader range of issues; 22 items were scored on a scale from 0 to 3 (). Cronbach's alpha was 0.80, giving substantially more variability than the T-1 instrument. In a PCA, the 22 items yielded a Scree plot revealing three components, explaining 44% of the variance. Items with factor loadings above 0.40 on one component, and at least 0.20 difference from factor loadings on other components, were chosen. Indices based on raw scores from the three components were labelled “psychosocial issues”, “cancer concern”, and “somatic issues”, and showed internal consistency (α) of 0.87, 0.70, and 0.74, respectively ().
Table II. Correlations between the 22 individual content items and consultation length at T-2.
To determine inter-rater reliability at T-2, two trained raters independently scored the same 20 videos using the Arizona Communication Interview Rating Scale (ACIR), which assesses clinical communication skills [Citation9]. The Intra-Class Correlation Coefficient (ICC [1.1]) was 0.84 [Citation8]. Because of the high correlation between ACIR and the sum of content scores for the 22 items (r = 0.82), we considered the inter-rater reliability for the content assessment at T-2 to be acceptable.
Statistics
Means, Pearson's correlations, ANOVA, Linear Regression Analyses, Principal Component Analysis with Varimax rotation, ICC, and reliability tests were conducted using the SPSS, version 16.0.
Results
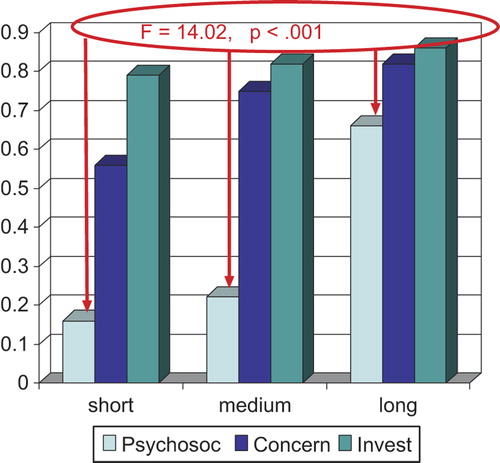
The correlation between the sum of obtained content and consultation length was r = 0.27 at T-1 (CI 95 = 0.022–0.468), and r = 0.66 at T-2 (CI 95 = 0.492–0.783). On item level, the correlation range at T-1 was 0 to 0.381, with the highest correlations for the two cancer items (see ). At T-2, the range was 0–0.644, with the highest correlations for the typical psychosocial items (see ). Correlations between the psychosocial, cancer concern, and somatic indices and consultation length at T-2 were r = 0.62 (p < 0.001), r = 0.32 (p = 0.012), and r = 0.16 (n.s.), respectively. The index of psychosocial issues showed the greatest increase from medium to long consultations at T-2 ().
Figure 1. Level (%) of the different content sub-indices by consultation length at internship completion. Notes: Psychosoc = psychosocial issues, Concern = the two cancer concern items, Invest = somatic issues. Short = consultation duration ≤ 10 minutes; medium = 11–13 minutes; long > 13 minutes. The F-value indicates difference in psychosocial content between the consultation-length groups.
The 34% (n = 21) of physicians spending more than 13 minutes at T-2 (time-spenders) obtained the most psychosocial content. In exploring the characteristics of these time-spenders (17 women, four men, n.s.), bivariate analyses yielded significant associations for perceived work stress in the emergency room, type of hospital, and giving the “patients” (i.e. the actors) an opportunity to disclose important issues. In a multivariate logistic regression, perceived work stress in the emergency room (more) and hospital type (local) during internship maintained significant independent influence on the dichotomous dependent variable (time-spenders > 13 minutes; non-spenders ≤ 13 minutes, 29% explained variance).
Discussion
As expected, a significant correlation between consultation length and content occurred at T-1, although at a low level. At T-2, this correlation was significantly stronger (non-overlapping CI intervals). This increased correlation can be seen to be in line with earlier findings in this sample regarding improved communication skills during internship (10), indicating both an enhanced awareness in the young physicians about using communication skills to obtain essential information, and their ability to organize the consultation. In an earlier study, we argued for the need to improve training in such skills, because the level we found in our sample at completion of medical school should have been higher (10). Possible ways of improving student physicians’ communication skills are to intensify training courses and introduce graduating examinations within the course, providing more motivation and emphasizing the importance of obtaining such skills. The results of the current study indicate the importance of the internship phase for the promotion of ongoing postgraduate development of skills when physicians are seeing many patients but are still in the education phase.
The strong positive association between the number of psychosocial issues addressed and length of consultation at T-2 is interesting, as the gain in psychosocial information occurred in consultations lasting for more than 13 minutes, consistent with the findings cited above (4,7).
The time-spending physicians (n = 21), who obtained the most psychosocial content, reported more work stress in the emergency room and had worked in local hospitals during their internships. More stress can indicate adaptable personality features making these physicians devoted to and/or conscientious about using time to relate adequately to patients and obtain relevant psychosocial information from them. These personality traits can be viewed as beneficial, even if they may generate more time pressure. A certain level of stress can be optimal for performing as expected, included the ability to address the patient's psychosocial aspects. Thus, the physicians can straighten out such patients more effectively by deciding whether to explore the issues further within their own setting or transfer the patient to a specialist. The significant association between the patients’ perceived opportunity to disclose important issues and consultation length was not maintained, but was mediated by hospital type, indicating that better opportunities exist for this purpose in smaller, rather than larger, hospitals.
The strength of this study is the nationwide sample, and the two assessments by the same physicians. A questionable aspect is the representativeness of our sample. Slightly more than a third (n = 111) of the eligible student cohort (n = 320) took part in the project. These student physicians might have viewed themselves as more skilful than those who did not participate, or might have seen the project as an opportunity to test their skills prior to their final exam. The loss of 13 of the 75 physicians at T-2 was viewed as random because of the unforeseen circumstances. We checked for possible differences in both time use and content between those who participated at T-1 and those who did not. No differences were found, and there were similar baseline values in the two groups for these two variables. However, we cannot exclude the possibility that those who participated on both occasions may have performed better in the videotaped situation than they would have in an ordinary clinical setting. Further, our sample is not necessarily representative of experienced GPs, their need for consultation time, or their interest in psychosocial aspects. However, a possible difference may not necessarily favour experienced GPs. Aspegren et al. found that graduating medical students were significantly more sensitive and responsive to patients’ concerns than were physicians with at least 10 years of training [Citation11]).
One limitation is the single-patient design, calling for cautiousness in generalizing our conclusions. More comprehensive studies with more variation of cases are needed. Systematic variation in the actors’ performances in the patient roles could be another limitation. Although they were professionally trained together before the consultations, some between-site variations in their behaviour could be observed in the videotapes, confirmed by a slight difference in the levels of their ratings for the physicians at T-2. However, when this was controlled for in the multivariate analyses, the results did not change.
Conclusions and implications
A strong association between consultation length and information, especially psychosocial information, obtained by the physicians at internship completion was found. This finding should be considered by faculty members and organizers of the internship period. Further research is needed to detect when, during the educational process, increased emphasis on communication skills training would be most beneficial for students/residents, and how the medical curriculum and internship period should be designed to optimize young physicians’ use of time in consultations.
Ethics
Ethical approval of the study was applied for, but not considered necessary by the Norwegian Data Service for Social Sciences.
Funding
Grant from the Norwegian authorities.
Declaration of interest
The authors report no conflict of interest. The authors alone are responsible for the content and writing of the paper.
References
- Kurtz S, Silverman J, Draper J. Teaching and learning communication skills in medicine. 2nd ed. Oxford: Radcliffe Medical Press; 2005.
- Pendleton D. The new consultation: Developing doctor– patient communication. 2nd ed. Oxford: Oxford University Press; 2003.
- Smith RC, Greenbaum DS, Vancouver JB, Henry RC, Reinhart MA, Greenbaum RB, . Psychosocial factors are associated with health care seeking rather than diagnosis in irritable bowel syndrome. Gastroenterology 1990;98: 293–301.
- Stirling AM, Wilson P, McConnachie A. Deprivation, psychological distress, and consultation length in general practice. Br J Gen Pract 2001;51:456–60.
- Deveugele M, Derese A, van den Brink-Muinen A, Bensing J, De Maeseneer J. Consultation length in general practice: Cross sectional study in six European countries. BMJ 2002; 325:472–7.
- Britt H, Valenti L, Miller GC, Farmer J. Determinants of GP billing in Australia: Content and time. Med J Aust 2004; 181:100–4.
- Hutton C, Gunn J. Do longer consultations improve the management of psychological problems in general practice?A systematic literature review. BMC Health Serv Res 2007;7:71.
- Gude T, Vaglum P, Baerheim A, Anvik T, Fasmer OB, Finset A, . Observed communication skills: How do they relate to the consultation content?A nationwide, observational study of medical students interviewing a standardized family practice patient. BMC Medical Education 2007;7:43.
- Stillman P. Arizona Clinical Interview Medical Rating Scale. Med Teach 1980;2:248–51.
- Gude T, Vaglum P, Anvik T, Baerheim A, Fasmer OB, Grimstad H, . Do physicians improve their communication skills between finishing medical school and completing internship?A nationwide prospective observational cohort study. Patient Educ Couns 2009;76:207–12.
- Aspegren K, Lonberg-Madsen P. Which basic communication skills in medicine are learnt spontaneously and which need to be taught and trained?Med Teach 2005;27:539–43.