Abstract
Objective. The aim of this study was to calculate the incidence and prevalence of radiating low back pain, to explore the long-term clinical course of radiating low back pain including the influence of radiculopathy (in a subsample of the study population) and non-radiating low back pain thereon, and to describe general practitioners’ (GPs’) treatment strategies for radiating low back pain. Design. A historic prospective cohort study. Setting. Dutch general practice. Subjects. Patients over 18 years of age with a first episode of radiating low back pain, registered by the ICPC code L86. Main outcome measures. Incidence and prevalence, clinical course of illness, initial diagnoses established by the GPs, and treatment strategies. Results. Mean incidence was 9.4 and mean prevalence was 17.2 per 1000 person years. In total, 390 patients had 1193 contacts with their GPs; 50% had only one contact with their GP. Consultation rates were higher in patients with a history of non-radiating low back pain and in patients with a diagnosis of radiculopathy in the first five years. In this study's subsample of 103 patients, L86 episodes represented radiculopathy in 50% of cases. Medication was prescribed to 64% of patients, mostly NSAIDs. Some 53% of patients were referred, mainly to physiotherapists and neurologists; 9% of patients underwent surgery. Conclusion. Watchful waiting seems to be sufficient general practice care in most cases of radiating low back pain. Further research should be focused on clarifying the relationship between radicular radiating low back pain, non-radicular radiating low back pain, and non-radiating low back pain.
Radiating low back pain is a condition predominantly treated by general practitioners, yet most descriptive studies have been performed in hospital settings.
In general practice, in 50% of cases of radiating low back pain, there is only one consultation between patient and doctor. When the GP establishes radiculopathy, there is a significantly increased consultation rate.
The ICPC code L86 registers radiating low back pain. This does not translate to a diagnosis of radiculopathy in all cases.
In most episodes, watchful waiting was sufficient general practice care. However, this does not necessarily mean that patients were entirely free of symptoms.
Introduction
Low back pain is a common health problem, affecting up to 80% of the population at some point in life [Citation1]. The prognosis of radiating low back pain is less favourable than that of non-radiating low back pain in terms of pain, disability, chronicity, loss of productivity, quality of life, and use of health care resources, especially if the pain radiates to below the knee, indicating radiculopathy [Citation2,Citation3,Citation4,Citation5].
Several aspects of radiating low back pain in general practice have not yet been clarified. Most descriptive research on the subject is performed in hospital settings with a short-term follow-up. Incidence and prevalence rates vary widely between studies because populations and definitions vary [Citation6,Citation7]. Little is known about the long-term clinical course of illness of radiating low back pain in general practice or about the treatment strategies employed by GPs. Radiating low back pain is registered with the ICPC code L86, which includes radiculopathy as well as non-radicular radiating low back pain in unknown proportions [Citation8,Citation9]. It is unclear if and how the presence of non-radiating low back pain at any time in a patient's medical history influences the course of illness in radiating low back pain.
We performed a historic prospective cohort study in a general practice population with a 10-year follow-up, aiming to calculate incidence and prevalence of radiating low back pain, explore the long-term clinical course of illness including the influence of non-radiating low back pain and radiculopathy thereon, to investigate what proportion of patients were initially diagnosed with radiculopathy and to describe the GPs’ treatment strategies for radiating low back pain.
Material and methods
Our study is a historic prospective cohort study for which the data were extracted from the Registration Network Groningen (RNG). The RNG consists of three group practices with a combined patient population of approximately 30 000. Anonymized data on reasons for encounter, prescriptions, and referrals are uploaded from the electronic patient records to the RNG database. In the Netherlands, with no free access to hospital care, a general practitioner is first consulted for every health problem. The RNG therefore contains a complete overview of its population's health care consumption. The GPs who participate in the RNG are trained and experienced in accurate registering [Citation10]. Health problems are registered in electronic patient files using units called episodes. An episode contains all information concerning a single health problem: correspondence, investigations, out-of-hours general practice encounters, (repeat) prescriptions, and personal work notes. It is important to note that these healthcare episodes represent the general practice care provided. This correlates to, but does not equal, disease. All elements within one episode are coded with one ICPC code [Citation8,Citation9]. The ICPC code L86 registers radiating low back pain. Our study database was created by including all patients over 18 years of age who had their first episode of radiating low back pain in 1998 or 1999 and following them for 10 years. Registration mistakes were assessed by two independent researchers and excluded.
Person days, the number of days patients are registered in a practice, were used to calculate incidence and prevalence and to correct for incomplete follow-up. Course of illness was explored by analysing the length of LRS episodes and the number of contacts within episodes, as well as the recurrences of radiating low back pain and whether patients underwent surgery. An episode was defined as ended when no L86 entries were made for one year. Treatment strategies distinguished were watchful waiting, medication, and referral. Prescription drugs with the same pharmacological working mechanism (i.e. NSAIDs) were grouped. Non-radiating low back pain is registered with the ICPC codes L02 and L03 in the Dutch version of the ICPC-1. When a patient had episodes coded with L02 and/or L03 before or after the L86 episode, this was defined as having a ‘pre-history’ or ‘post-history’ of non-radiating low back pain. In a representative (as to sex and age) subsample of patients (n = 103), we searched the medical files to investigate whether there was an initial diagnosis of radiculopathy.
Statistical analysis was carried out with SPSS® software. Kaplan–Meier analysis was used to estimate the probability of patients consulting their GP, which provides information on the length of healthcare episodes. End point was the date an episode ended (see above), which does not necessarily mean that the patient was recovered. We stratified by gender, age group, pre-history of non-radiating low back pain, and initial diagnosis of radiculopathy or not (the last criterion only for the subsample in which this was investigated). Age groups were: 18–44 years, 45–64 years, and 65+, determined by age at inclusion. An independent sample t-test was used to compare differences in mean consultation rates between subgroups and a log-rank test to compare differences between subgroups in the Kaplan–Meier analysis. To compare incidence and prevalence the Pearson chi-square test was used. The Mann–Whitney or Kruskal–Wallis tests were used in case of a skewed distribution.
Results
Population
We included 390 patients () with a mean age of 47 years and 50% men. A total of 134 patients (34%), with a mean age of 50 and 49% men, left the database before the follow-up period finished, after a mean period of four years. Our subsample of 103 patients had a mean age of 49 years and 52% were men.
Incidence and prevalence
We found mean incidence and prevalence rates of 9.4 and 17.2 per 1000 person years (), lower in men and highest in patients in the oldest age group.
Table I. Incidence and prevalence of radiating low back pain in general practice per 1000 person-years, stratified by gender and age, for each follow-up year (RNG population 18 + years, 1998–2008).
Course of illness
In all, 381 patients (98%) had face-to-face contact with their GPs for radiating low back pain in 1193 contacts: 1006 contacts (84%) were regular visits to the GP's office, 168 (14%) were house-calls, and 19 contacts (2%) were out-of-hours general practice care. Among these patients, 189 patients (50%) had one contact, 161 patients (42%) had two to five contacts, and 31 patients (8%) had six or more. There were no significant differences between gender and age groups regarding the number of contacts.
Radiating low back pain recurred in 91 patients (23%), significantly more often in women than in men: 54 vs. 37 times, (p = 0.04). Eighteen patients had more than one recurrence. We found a pre- history (see method) of non-radiating low back pain in 96 patients and a post-history in 86, 79 patients had both, and 120 had neither. More women than men had post-histories of non-radiating low back pain: 69 versus 96, p = 0.03. Presence of a pre-history of non-radiating low back pain did not significantly influence the occurrence of a post-history. Thirty-three patients (9%) underwent one to three surgical procedures, totalling 43 interventions. Eight patients had surgery more than once. Men had surgery significantly more often than women: 24 operations in 16 men versus 19 operations in 17 women (p = 0.03). Fourteen patients were referred as medical emergencies; eight of these had surgery for cauda equina syndrome. The initial diagnosis in our subsample was radiculopathy in 53 cases, non-radicular radiating low back pain in 48 cases, and spinal stenosis in two cases.
Consultation rate probability and episode length
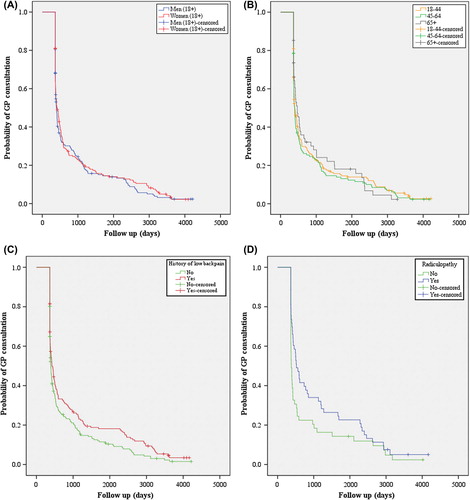
In , the Kaplan–Meier curves estimating the probability of patients consulting their GP because of radiating low back pain are shown. Within one year, 82% of episodes had ended. We found no significant differences between sexes and age groups regarding episode length. Patients with a pre-history of non-specific low back pain had a significantly higher consultation rate probability for radiating low back pain (log rank 0.036). In our subsample we found a significantly higher consultation rate probability in patients with an initial diagnosis of radiculopathy than in patients without over the course of five years (log rank 0.020) but not with a follow up of 10 years (log rank 0.059). At the end of the follow-up period there were only three patients left.
Treatment strategies
Treatment strategies chosen in subsequent contacts are shown in . No differences were found between sexes and age groups. Medication and referrals for radiating low back pain stratified by gender and age groups are shown in . Medication was prescribed to 250 patients (64%). The number of prescriptions per patient varied from 1 to 82, totalling 1321, mostly for NSAIDs (52%). Some 50% of prescriptions were written in the first year of an L86 episode. During our study period, 205 patients (53%) were referred for radiating low back pain. The number of referrals varied between one and 12 per patient, totalling 400; 60% of the referrals were to other primary care professionals, mainly physiotherapists. Referrals to medical specialists (40%) were mainly to neurolo- gists. Fourteen patients were referred to neuro- surgeons as medical emergencies. More than half of the referrals took place in the first year of the episode, with a median of 18 days after the first contact.
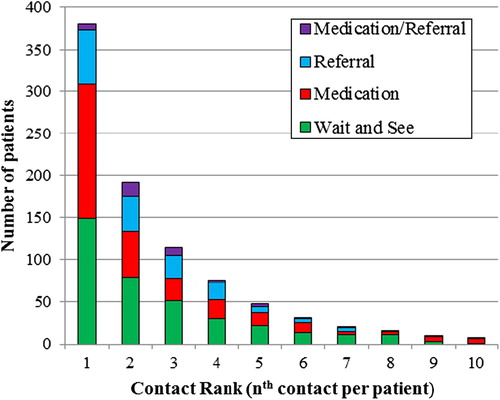
Table II. Treatment strategies: Prescriptions and referrals for radiating low back pain in general practice (RNG population 18+ years, 1998–2008).
Discussion
Principal findings
In our study, 50% of radiating low back pain episodes consisted of one contact between patient and GP. Episodes of radiating low back pain in which patients make use of general practice care over a long period of time are uncommon and are correlated with a history of non-radiating low back pain and (probably) with an initial diagnosis of radiculopathy. Episodes registered by the ICPC code L86 represented radiculopathy in about half of the cases and non-specific radiating low back pain in the other half. In most episodes, watchful waiting was sufficient general practice care. However, this does not necessarily mean that patients were entirely free of symptoms.
Strengths and weaknesses
Strengths of our study are the long-term follow-up and the general practice setting. The GPs who participate in the RNG are accurate in registering morbidity, which makes our database reliable [Citation10]. There are also limitations. From a caregiver perspective, it seems strange that GPs would choose a wait-and-see policy for radiating low back pain after five or more consultations, as was done in 40 cases (see ). It is possible that recurrences of radiating low back pain have been filed under previous episodes, giving the impression of single lengthy episodes with many contacts where in fact there were multiple, shorter episodes. Or, multiple L86 episodes may have occurred within one year, which in our study would be regarded as one episode. Finally, as mentioned earlier, general practice care provided to patients does not equal information regarding the diseases of patients. However, especially in the Dutch healthcare system where referral by a GP is necessary to obtain hospital care, consumption of healthcare does correlate to disease.
Other research
The LINH study (LINH = Dutch national information network of primary care) explored the incidence and prevalence of radiculopathy in Dutch general practice, using the same ICPC code (L86) as we did to select their patient population [Citation11]. Between 2003 and 2010, the LINH found a mean incidence of 10.3 (9.4 in our study), and a mean prevalence of 15.1 (17.2 in our study) per 1000 person years. In our study, peak incidence and prevalence occurred in the 65 + age group but in the LINH study peak incidence and prevalence (16.0 and 25.0 respectively) occurred in a younger population of 45- to 64-year-olds. During our study period, the incidence per 1000 person years remained stable while the prevalence rose. This implies that the number of new cases per year remained the same, but that the episodes lasted longer in later years. In the LINH study, this trend is not found. In 2005, Luijsterburg et al. performed a database study investigating GPs’ prescribing habits for radiculopathy, also making use of ICPC code L86. The GPs prescribed NSAIDs to the majority of patients, which is similar to what we found [Citation12].
Conclusion
The ICPC code L86 is used to identify patients with radiculopathy in both the above-mentioned studies and in others, but, as stated, it literally registers radiating low back pain [Citation2,Citation13]. From our subsample we know that this includes probably about as many cases of non-specific radiating low back pain as “true” radiculopathy. This finding has significant implications for the use of registry data since assumptions and conclusions on specific conditions may be far from the truth. More research is needed to clarify the diagnoses to which the registry code of L86 translates (and ultimately, perhaps, these codes need adjustment).
Declaration of interest
There are no conflicts of interest in connection with the paper. The authors alone are responsible for the content and writing of the paper.
No external funding was received for this study.
References
- Van Tulder M, Koes B, Bombardier C. Low back pain. Best Pract Res Clin Rheumatol 2002;16:761–75.
- Mens JMA, Chavannes AW, Koes BW, Lubbers WJ, Ostelo RWJG, Spinnewijn WEM. NHG-standaard lumbosacraal radiculair syndroom. Huisarts en wetenschap [NHG-guideline lumbosacral syndrome] 2005;48:171–8.
- Valat JP, Goupille P, Rozenberg S, Urbinelli R, Allaert F, Spine group of the Société Française. Acute low back pain: Predictive index of chronicity from a cohort of 2487 subjects. Spine Group of the Société Française de Rhumatologie. Joint Bone Spine 2000;67:456–61.
- Konstantinou K, Hider SL, Jordan JL, Lewis M, Dunn KM, Hay EM. The impact of low back-related leg pain on outcomes as compared with low back pain alone: A systematic review of the literature. Clin J Pain 2013;29:644–54.
- Kristman VL, Hartvigsen J, Leboeuf-Yde C, Kyvik KO, Cassidy JD. Does radiating spinal pain determine future work disability? A retrospective cohort study of 22,952 Danish twins. Spine 2012;37:1003–13.
- Nachemson A, Waddell G, Norlund A. Epidemiology of neck and low back pain. In: Nachemson A, Jonsson E, editors. Neck and back pain: The scientific evidence of causes, diagnosis and treatment. Philadelphia: Lippincott, Williams & Wilkins; 2000.
- Hider SL, Whitehurst DG, Thomas E, Foster NE. Pain location matters: The impact of leg pain on health care use, work disability and quality of life in patients with low back pain. Eur Spine J 2014;May 18.
- Gebel RS, Lamberts H. ICPC-1 met Nederlandse subtitels [ICPC-1 with Dutch subtitles]. Utrecht: Dutch College of General Practitioners; 2000.
- Hofmans-Okkes IM, Lamberts H. The International Classification of Primary Care (ICPC): New applications in research and computer-based patient records in family practice. Fam Pract 1996;13:294–302.
- Van der Werf GT, Smith RJA, Stewart RE, Meyboom-de Jong B. Spiegel op de huisarts; over registratie van ziekte, medicatie en verwijzingen in de geautomatiseerde huisartspraktijk [Mirroring the general practitioner; on registration of morbidity, medication and referral in Dutch general practice]. Groningen: Groningen University Publisher; 1998.
- http://www.nivel.nl/NZR/zorgregistraties-eerstelijn (accessed May 2010).
- Luijsterburg PA, Verhagen AP, Braak S, Oemraw A, Avezaat CJ, Koes BW. General practitioners’ management of lumbosacral radicular syndrome compared with a clinical guideline. Eur J Gen Pract 2005;11:113–18.
- Hagen KB, Thune O. Work incapacity from low back pain in the general population. Spine 1998;23:2091–5.