Abstract
Background. Our study aims to investigate whether information given by radiation oncologists to their patients is tailored to the patient's desired level of information and, if so, what the effect of tailoring is on patient-reported outcomes, i.e. satisfaction, health, anxiety and self-efficacy. Material and methods. Consecutive radiotherapy patients (n = 150) completed a baseline questionnaire one week before their initial consultation, immediately following this consultation, and again one week prior to their first follow-up visit. The initial consultation was videotaped and 10 radiation oncologists’ information giving behavior (content and duration) analyzed. Results. The overall amount of information provided by the radiation oncologists matched with patients’ information needs in 50.8% (k = 0.07) of the consultations. No significant associations between tailored information giving and patient-reported outcomes were found, except for tailoring of information on procedures, and patients’ anxiety and global health. These associations were no longer significant when correcting for patients’ background characteristics. Conclusion. This study shows that radiation oncologists poorly tailor their information to the needs of their patients. However, lack of tailoring is not associated with worse patient-reported outcomes. Until more evidence is available, radiation oncologists may explicitly ask patients about their information preferences and tailor the information provided accordingly.
About half of cancer patients in the Netherlands receive radiotherapy during their treatment [Citation1]. However, patients have difficulty understanding radiotherapy because it is relatively unfamiliar and not immediately ‘visible’. Thus, although information can reduce patients’ fears about radiotherapy [Citation2], optimal information provision remains a challenge.
Radiotherapy patients vary in their information needs [Citation3]. Some prefer limited information because this helps them to stay optimistic [Citation4]. A lower information need was associated with being older and male, having lung or rectal cancer, more difficulty with understanding, and a higher trait anxiety level [Citation5]. Radiotherapy patients’ preference for information about side effects differed depending on their expected severity and odds of occurring [Citation6]. Physicians have strived for an optimal balance between giving the information they are required to give and allowing for the individual patient information needs. Such tailored information giving could indeed lead to better patient outcomes [Citation7].
One review showed that most studies focussing on tailoring of physician behavior and patients’ information needs investigated the concordance between patient and physician through questionnaires [Citation7]. A better match was indeed found to be associated with better patient outcomes [Citation7]. Only one study addressed tailoring of information giving to radiotherapy patients by investigating the match between patient information preferences and observed physician information giving during the consultation [Citation8]. However, all patients in this study had high information needs and most radiation oncologists used a similar communication style for most of their patients.
Our study aims to investigate whether information given by radiation oncologists to their patients is tailored to the patient's desired level of information and, if so, what the effect of tailoring is on patient-reported outcomes, i.e. satisfaction, health, anxiety and self-efficacy. This prospective study addresses three research questions: 1) Are there differences between and within radiation oncologists in the amount of information giving? 2) If so, are these tailored to the patients’ information needs? and 3) What is the effect of such tailoring on patient-reported outcomes, more specifically satisfaction, anxiety, health status and self-efficacy?
Material and methods
Study sample
Nine senior radiation oncologists and six residents in training at our Academic Medical Center agreed to study participation. Consecutive eligible patients referred for radiotherapy were asked to participate. Inclusion criteria were: age ≥ 18 years, no previous radiotherapy, being able to adequately read and write Dutch, and not having cognitive problems or a brain tumor.
Procedures
Eligible patients received a questionnaire by mail before their first radiotherapy consultation. Patients who declined participation were asked a question addressing their overall information preference, as included in the study questionnaire; their gender and date of birth were recorded from the medical chart.
Patients giving informed consent were asked to complete a baseline questionnaire (T1) in the week before the initial visit and a follow-up questionnaire (T3) on average three to five weeks after this visit. The initial visit was videotaped and patients were asked to complete a checklist (T2) immediately afterwards.
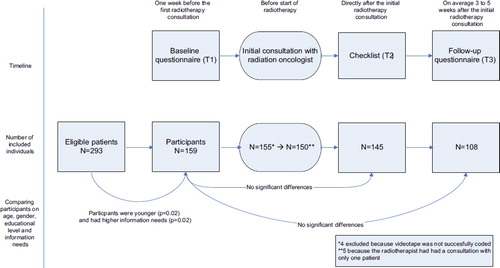
presents the study design. The study was approved by the local Medical Ethical committee.
Measures
Background variables. Patients’ gender, age, educational level, trait anxiety and health literacy were assessed by self-report at baseline (T1) [Citation4]. Trait Anxiety was measured with the trait scale of the State-Trait Anxiety Inventory (STAI; [Citation9]). Health literacy was measured with three items assessing the ability to perform basic reading and numerical tasks required to function in the healthcare environment [Citation10]. Diagnosis was recorded from the medical chart.
Patients’ information needs. The Information Preferences of Radiotherapy Patients Questionnaire (IPRP) [Citation5] assesses patients’ need for information about radiotherapy. This 35-item questionnaire consists of six domains: 1) Disease (5 items; α = 0.93); 2) Treatment (5 items; α = 0.79); 3) Procedures (6 items; α = 0.89); 4) Side effects (7 items; α = 0.92); 5) Prognosis (7 items; α = 0.94); and 6) Psychosocial aspects (4 items; α = 0.86). For all questions, response categories (5-point scale) ranged from ‘I want to know nothing about it’ to ‘I want to know all about it’. Higher score reflects a higher information need. Subscale scores were calculated, as well as a total IPRP score (range 1–5). As the number of items in the subscales of the IPRP varies, mean percentage scores were calculated to compare subscale scores.
Radiation oncologists information giving. The content of the consultations was coded by four raters. We used the IPRP [Citation5] to categorize the different topics of information given during the consultation. We distinguished between information given about: 1) disease and diagnosis; 2) prognosis; 3) radiotherapy and related treatment; 4) other medical treatments; 5) the radiotherapy procedure; 6) side effects of radiotherapy; 7) psychosocial issues; and 8) other information given (see ). The occurrence and length of information given on a specific domain was coded by marking the beginning and end of every information content domain in the conversation.
Table I. Coding instrument.
The coding instrument was integrated in specialized software, the Observer® XT (Noldus). Comparisons of ratings were used to facilitate the training of raters in using the coding instrument and to feed discussion at regular consensus meetings. To assess inter-rater reliability, two raters independently coded a different random subsample of 15 consultations, leading to five double-coded consultations per couple of raters.
Patient-reported outcomes. Patient satisfaction concerning the initial consultation was assessed directly afterwards (T2) with the Patient Satisfaction Questionnaire [Citation11], consisting of five items (Cronbach's α = 0.89). A higher score reflects more satisfaction.
The patients’ state anxiety was assessed at follow-up (T3) with the seven-item Anxiety-subscale (Cronbach's α = 0.86) of the Hospital Anxiety and Depression Scale (HADS; [Citation12]).
Self-reported health status was assessed at follow-up (T3) with two items of the EORTC-QLQ-C30 [Citation13] measuring global health. The sum score ranges from 0 to 100.
Patients’ self-efficacy in obtaining medical information and physicians’ attention to their concerns was assessed at follow-up (T3) with the Perceived Efficacy in Patient-Physician Interactions (PEPPI), consisting of 10 items (Cronbach's α = 0.94) [Citation14]. Item scores are summed, with the scores ranging from 10 to 50. Higher scores reflect higher self-efficacy.
Data analyses
Descriptive statistics were used to characterize the study sample. We compared included patients with the total sample of eligible patients with Pearson χ2, Fisher's Exact, Mann-Whitney and independent t-tests as appropriate.
Inter-rater reliability. Variance components were estimated by using the restricted maximum likelihood method. Based on these estimations relative and absolute agreement between individual raters were calculated. We calculated relative (i.e. the level of agreement per domain between two raters for the ranking of duration of information giving) and absolute agreement (i.e. agreement per domain between two raters on the absolute rating of duration of information giving) for every couple of two raters who observed the same five videotapes. The relative agreement coefficient varies between 0 (no agreement) and 1 (perfect agreement), the absolute agreement coefficient varies between 0 and the value of the relative agreement coefficient.
The average relative agreement over the content domains was 0.61 (range 0.25–0.89) and the average absolute agreement was 0.57 (range 0.24–0.88). The information domains with the highest agreement were prognosis (absolute 0.88; relative 0.89) and side effects (absolute 0.66; relative 0.70); the lowest levels of agreement were for psychosocial issues (absolute 0.24; relative 0.25).
Patient's information needs. Given the skewed distribution of the IPRP subscale scores, the needs were dichotomized with average responses below 4 labeled as low information need, and average responses of 4 and above labeled as high information need. Mean, standard deviations (SD), and percentage of individuals having high or low information needs are reported.
Tailoring of information giving. Based on coding of the consultations, time spent on information giving per content domain, and total time spent on information giving, could be calculated. Consultations with an amount of time spent on information giving that was below the mean amount of time spent on information giving in the consultations were coded as ‘low duration of information giving’; consultations with an amount of time spent on information giving above the mean duration spent on information giving in the consultations were coded as ‘high duration of information giving’. Consequently, for each content domain, information giving fell in either one of two categories, namely under or above the mean.
Differences between radiation oncologists in duration of information giving were investigated with a one-way ANOVA. Furthermore, MLwiN version 2.22 (Centre for Multilevel Modelling, University of Bristol, UK) was used to investigate if data on information giving for radiation oncologists were nested within radiation oncologists. As data for radiation oncologists were uncorrelated we did not use multilevel methods in further analyses.
Tailored information giving was defined as a match between patients’ information need (low vs. high, see patients’ information needs) and duration of time spent on information provided by the radiation oncologist (under vs. above the mean). Consultations thereby fell in one of four categories: ‘low-low’ ‘low-high’ ‘high-low’ ‘high-high’ (see ). The percentage match that followed out of combining the categories ‘low-low’ and ‘high-high’ was calculated by cross tables and Cohen's kappa was determined to assess the degree of agreement.
Table II. Match between patients’ information needs and the duration of information giving (n = 150).
Before performing regression analyses we performed independent t-tests and Mann-Whitney tests to investigate the association between tailoring of information and patient-reported outcomes, i.e. satisfaction, anxiety, global health and self-efficacy. When a significant association was found, hierarchical multiple regression analyses were carried out to correct for gender, age, educational level, trait anxiety and health literacy. In the first step of the model, match was entered into the regression model. In the second step, gender, age, educational level, trait anxiety and health literacy were also entered.
All analyses were carried out with SPSS version 18.0 (Chicago, Illinois, USA). A p-value of 0.05 (two-sided) was considered statistically significant.
Results
Sample characteristics
Of 293 eligible radiotherapy patients, 159 (54%) agreed to participate. Non-responding patients were on average older (M = 66.61 ± 13.49 vs. M = 62.90 ± 12.83; p = 0.02), had lower overall information needs (M = 7.91 ± 2.27 vs. M = 8.55 ± 2.28; p = 0.02), but did not differ in gender. Most reported reasons for not wanting to participate were finding participation too burdensome (52%) or the study not appealing (15%). Other reasons were that patients said never to participate in studies (8%), to object video recording (8%), being too tired/sick (8%), or having no time (5%). Of 155 participants, the intake consultation could be videotaped and fully analyzed (). shows their sociodemographic and clinical characteristics.
Table III. Sociodemographic characteristics of the respondents (n = 155).
For three senior staff members and two residents in training, only one videotaped consultation was available; these oncologists and their patients were removed from the current analyses leading to 150 included consultations.
Patients’ information needs
The need for information among new radiotherapy patients was high (the average on the total IPRP scale M = 4.21; SD = 0.75). At the same time, the number of patients having lower information needs varies across information domains: from 18% for side effects to 60% for psychosocial information (see ).
Table IV. Patients’ information needs.
Radiation oncologists information giving
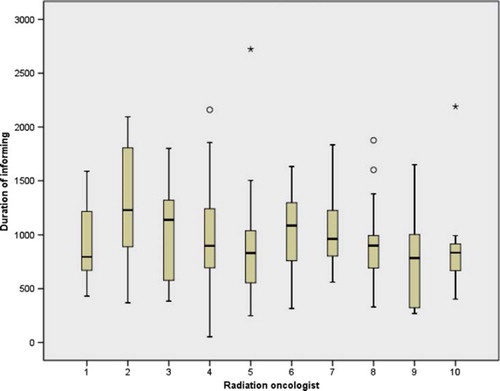
The consultations lasted on average 45.50 (SD = 15.54) min; on average 16.39 (SD = 7.76) min per consultation were spent on information giving (see ). shows the distribution of total time spent on information giving per radiation oncologist. As shown, within each individual radiation oncologist the amount of total time spent by this radiation oncologist on information giving varied. Generally, no significant differences were found between radiation oncologists in time spent on information giving [F (9, 140) = 1.37, p = 0.21]. Radiation oncologists differed in time spent on information giving on prognosis (ω = 2.13, p < 0.05) but not on other subjects.
Table V. Time spent on information giving per domain.
Tailoring of information giving
The percentage match between overall information needs of the patient in general and the total amount of information provided by the radiation oncologist was 50.8% (κ = 0.07). The highest match was seen for information on psychosocial issues (60.4%), while the lowest match was observed for information about procedures (44.2%) ().
Tailoring and patient outcomes
Tailoring of information to patient's overall information need was not associated with any of the patient-reported outcomes (satisfaction, state anxiety, health status and self-efficacy). Tailored information on ‘Procedures of radiotherapy’ was associated with reduced anxiety (p = 0.02) and increased global health (p = 0.02). Tailored information in other domains was not associated with outcomes. Mean and SD of the patient outcomes are presented in .
Table VI. Patient-reported outcome measures.
We subsequently performed multiple regression analyses for the domain procedures, with state anxiety and global health as dependent variables, and taking patients’ background characteristics into account (). The match for information giving about procedures, entered first into the model, explained 5% of the variance in state anxiety. When gender, age, educational level, trait anxiety and health literacy were added to the model, 39% of the variance in state anxiety could be explained. However, in this model match was no longer significantly associated with state anxiety. The match for information giving about procedures explained 6% of the variance in global health. Inclusion of the background characteristics in the model resulted in 40% variance of global health explained. However, in this model match was no longer significantly associated with global health.
Table VII. Hierarchical multiple regression analyses for tailoring of information for patients’ information needs about procedures.
Discussion
Since extensive information provision may not necessarily be beneficial to all patients, it is suggested that we should preferably move toward patient-tailored care taking individual variation into account [Citation15]. Patients may benefit from a tailored information giving approach [Citation16]. For example, a study in which standardized information was provided in a stepwise manner showed a decrease in anxiety and higher patient satisfaction [Citation17]. Whereas most studies on tailoring so far addressed concordance, the present study investigated the association between actual information provision by radiation oncologists and patients’ information preferences and relates these to outcomes.
Our results indicate that radiation oncologists generally do not gear their amount of information giving to the individual information needs of their patients. The chance that their behavior fits the needs of the patient is comparable to flipping a coin. This is in line with studies investigating the association between actual information giving behavior and patient preferences in cancer patients eligible for adjuvant treatment [Citation8] and in women from high-risk breast cancer families [Citation18]. Qualitative studies have also shown that it is difficult to tailor information about radiotherapy to patients’ needs [Citation19]. Also, changing needs over time [Citation3,Citation20] makes tailoring even more complicated.
However, the present study further suggests that perhaps tailored information is not as important as generally assumed. Tailoring information did not lead to higher satisfaction in the short term, or to better health, lower state anxiety or higher self-efficacy in the long term. Only tailoring of information regarding radiotherapy procedures, an important subject at the initial consultation, reduced patients’ anxiety and increased their global health. However, when corrected for background variables associated with information needs, such tailoring of information was no longer associated with anxiety and health. This contradicts a review showing that tailoring is associated with better patient outcomes [Citation7]. However, in none of the reviewed studies was the actual information provided by physicians examined.
One explanation for not finding tailoring between information giving and patients’ preferences is that radiation oncologists may not be aware of the need to tailor information to patients’ needs. Also, alternative explanations are possible. First, the association between patients’ information preferences and radiation oncologists’ information giving may be mediated by the patient's behavior, such as their question asking or expression of informational cues. If so, patient's preferences would need to be reflected in their actual behavior during the consultation. For example, a study among oncology patients showed that higher information needs are associated with increased question asking during the consultation [Citation21]. In this study, we do not know whether this is indeed the case. Yet, if patient participation is limited it is difficult for physicians’ to judge their patients information preference. Further investigation is needed to better understand how tailoring may be achieved during the interaction. Second, the lack of association between tailoring and patient-reported outcomes found may result from the fact that the quality of information is more important than the quantity. Yet, we found that radiation oncologists’ information-giving behavior (e.g. the extent to which they stimulated question asking) was not associated with greater patient satisfaction (Smets et al. submitted). Thus, future studies should preferably also assess the quality of information provision.
The present study has a number of strengths. First, we are among the first to study a match between actual behavior and preferences instead of a match between preferences and ratings after the consultation. Second, inter-rater reliability of the coding of the videotapes was generally high, leading to reliable assessment of information giving. Only, the agreement for the domain psychosocial issues was low. Therefore, results for this domain should be interpreted with some caution. Third, we are among the first to study tailoring in the radiotherapy setting.
However, some limitations should also be noted. First, the overall response rate was relatively low, most likely because the patients had just received their cancer diagnosis and were not motivated to fill out an extensive questionnaire. Non-responders were older and had lower information needs. Therefore, the actual number of patients with low information needs would probably have been higher should these patients have participated. However, it is difficult to judge how this might have influenced the study outcomes. Older patients with low information needs may be more passive and as a result radiation oncologists might feel that they can more easily leave out information. In that case, the percentage of tailoring by radiation oncologists could have been somewhat higher than currently reported. On the other hand, radiation oncologists could feel the need to give at least a minimum amount of information, regardless of these patients lack of active participation. If so, the current percentage of tailoring by radiation oncologists could have become even lower. Second, our sample size is smaller than what we aimed for. A larger sample size would have allowed us to detect smaller effects. Third, possible ceiling and floor effects were seen for information needs and anxiety. This leads to low variance in the data, and made it more difficult to find significant associations. Fourth, consultations with the radiation oncologist were videotaped, possibly leading to a Hawthorne-effect: adaptation of behavior due to the observation. This could mean that our videotaped consultations do not reflect real practice. However, studies have shown that video recording has little influence on the behavior of either doctors or patients [Citation22,Citation23].
In conclusion, our study shows that radiation oncologists do often not tailor their information provision to patients needs. This might lead to the conclusion that training of radiation oncologists in this regard might be needed. Yet, a lack of tailoring was not associated with worse patient-reported outcomes. Thus, does tailoring matter to the patient? Currently, although most healthcare professionals believe that information should be tailored to patients’ needs, little evidence supports this [Citation16]. So far, most research has focused on concordance between patient and physician's preferences [Citation7]. More research on actual behavior is needed to elucidate if and how actual tailoring behavior during the consultation can influence patient-reported outcomes. Such research might also include other, more qualitative, indicators of tailoring (e.g. perception of radiation oncologists of their own capacity to tailor in a specific consultation) than we used in our study. Until then, we recommend that radiation oncologists explicitly ask their patient about information preferences and tailor the information provided accordingly.
Acknowledgments
This study was financially supported by the Dutch Cancer Society (grant UVA 2005 - 3199). The Dutch Cancer Society had no role in the study design, data collection, analysis or interpretation of the data; in the writing of the manuscript; and in the decision to submit the manuscript for publication. The authors are grateful to all patients and radiation oncologists who participated in this study, and also thank the coders who carefully coded the videotapes. The authors have no conflict of interest to be reported.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- van Daal WA, Bos MA. Infrastructure for radiotherapy in The Netherlands: Development from 1970 to 2010. Int J Radiat Oncol Biol Phys 1997;37:411–5.
- Halkett GK, Kristjanson LJ. Validity and reliability testing of two instruments to measure breast cancer patients’ concerns and information needs relating to radiation therapy. Radiat Oncol 2007;2:43.
- Halkett GK, Kristjanson LJ, Lobb E, O'Driscoll C, Taylor M, Spry N. Meeting breast cancer patients’ information needs during radiotherapy: What can we do to improve the information and support that is currently provided? Eur J Cancer Care (Engl) 2010;19:538–47.
- Ter Hoeven CL, Zandbelt LC, Fransen S, de HH, Oort F, Geijsen D, . Measuring cancer patients’ reasons for their information preference: Construction of the Considerations Concerning Cancer Information (CCCI) questionnaire. Psychooncology 2010;20:1228–35. DOI:10.1002/pon.1841.
- Zeguers M, De Haes HC, Zandbelt LC, Ter Hoeven CL, Franssen SJ, Geijsen DD, . The information needs of new radiotherapy patients: How to measure? Do they want to know everything? And if not, why? Int J Radiat Oncol Biol Phys 2012;82:418–24. DOI:10.1016/j.ijrobp.2010.09.032.
- Barnett GC, Charman SC, Sizer B, Murray PA. Information given to patients about adverse effects of radiotherapy: A survey of patients’ views. Clin Oncol (R Coll Radiol) 2004; 16:479–84.
- Kiesler DJ, Auerbach SM. Optimal matches of patient preferences for information, decision-making and interpersonal behavior: Evidence, models and interventions. Patient Educ Couns 2006;61:319–41.
- Leighl N, Gattellari M, Butow P, Brown R, Tattersall MH. Discussing adjuvant cancer therapy. J Clin Oncol 2001; 19:1768–78.
- Spielberger CD. Manual for the State-Trait Anxiety Inventory STAI (From Y). Palo Alto, CA: Mind Garden; 1983.
- Chew LD, Bradley KA, Boyko EJ. Brief questions to identify patients with inadequate health literacy. Fam Med 2004; 36:588–94.
- Ong LML, Visser MRM, Lammes FB, de Haes JCJM. Doctor-patient communication and cancer patients’ quality of life and satisfaction. Patient Educ Couns 2000;41:145–56.
- Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983;67:361–70.
- Aaronson NK, Visser-Pol E, Leenhouts GH, Muller MJ, van der Schot AC, van Dam FS, . Telephone-based nursing intervention improves the effectiveness of the informed consent process in cancer clinical trials. J Clin Oncol 1996;14:984–96.
- Zandbelt LC, Smets EM, Oort FJ, Godfried MH, de Haes JC. Satisfaction with the outpatient encounter. J Gen Intern Med 2004;19:1088–95.
- Sepucha K, Ozanne EM. How to define and measure concordance between patients’ preferences and medical treatments: A systematic review of approaches and recommendations for standardization. Patient Educ Couns 2010;78:12–23.
- Arora NK, Street RL, Jr., Epstein RM, Butow PN. Facilitating patient-centered cancer communication: A road map. Patient Educ Couns 2009;77:319–21.
- D’ haese S, Vinh-Hung V, Bijdekerke P, Spinnoy M, De BM, Lochie N, . The effect of timing of the provision of information on anxiety and satisfaction of cancer patients receiving radiotherapy. J Cancer Educ 2000;15:223–7.
- Lobb EA, Butow PN, Meiser B, Barratt A, Gaff C, Young MA, . Tailoring communication in consultations with women from high risk breast cancer families. Br J Cancer 2002;87:502–8.
- Gamble K. Communication and information: The experience of radiotherapy patients. Eur J Cancer Care (Engl) 1998;7:153–61.
- Douma KF, Koning CC, Zandbelt LC, De Haes HC, Smets EM. Do patients’ information needs decrease over the course of radiotherapy? Support Care Cancer Epub 2011 Nov 13. DOI: 10.1007/s00520-011-1328-0.
- Eggly S, Harper FW, Penner LA, Gleason MJ, Foster T, Albrecht TL. Variation in question asking during cancer clinical interactions: A potential source of disparities in access to information. Patient Educ Couns 2011;82:63–8.
- Coleman T. Using video-recorded consultations for research in primary care: Advantages and limitations. Fam Pract 2000;17:422–7.
- Themessl-Huber M, Humphris G, Dowell J, Macgillivray S, Rushmer R, Williams B. Audio-visual recording of patient-GP consultations for research purposes: A literature review on recruiting rates and strategies. Patient Educ Couns 2008;71:157–68.