To the Editor,
Head and neck cancers are a heterogeneous group of malignancies with different prognosis according to histopathology, site of origin, TNM stage at diagnosis. Independent of the prognosis every diagnosis of a head and neck malignancy is going to have a relevant impact on a patient's quality of life also caused by treatments, which involve structures fundamental for relational life, feeding, breathing, verbal and non-verbal communication [Citation1]. In particular, radiotherapy for head and neck cancer using standard techniques is associated with several side effects, which are usually permanent and relevant for the quality of life [Citation2–4].
The development and diffusion of intensity- modulated radiation therapy (IMRT) in the last decade has allowed a dose escalation to sites of gross disease while reducing the dose given to critical tissues [Citation5–9].
One of the more characteristic late toxicities of radiotherapy in head and neck cancer is xerostomia, recorded in many patients after irradiation, and associated with persistent discomfort, dental problems, oral infection and dysphagia for solid food. The IMRT parotid-sparing treatment is associated with a dose reduction to the salivary tissue and a markedly lower incidence of xerostomia.
Nevertheless, in our institution we observed one case of nodal recurrence within the deep lobe of a spared parotid gland after IMRT and therefore we reviewed the literature to find other reports, guidelines and/or recommendations.
Case presentation
A 48-year-old man came to our observation with right monolateral progressive nasal obstruction and omolateral fullness and conductive hearing loss.
During physical examination and flexible endoscopy a reddish exophytic mass implanted on the lateral wall of the nasopharynx was located.
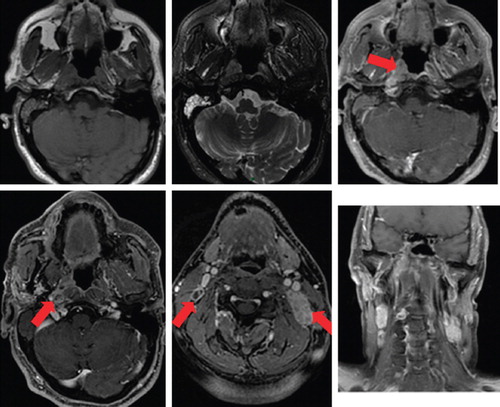
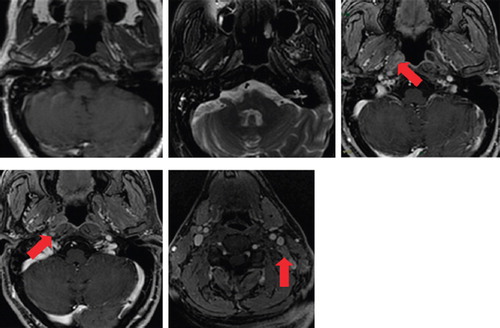
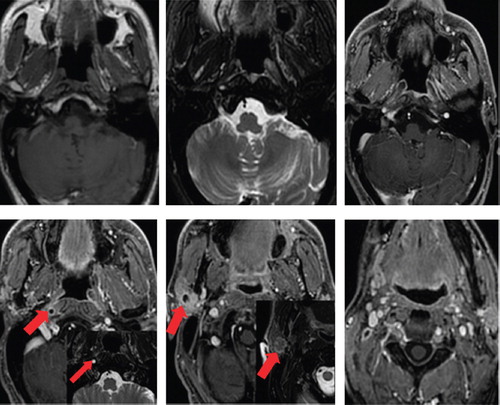
A magnetic resonance imaging (MRI) of the face and skull showed an asymmetric mass in the right later wall of the nasopharynx extending to lateral pharyngeal recess, torius tubarius and Eustachian tube. Bilateral regional adenopathies (level II and III) were revealed, demonstrating hypermetabolic activity on positron emission tomography (PET). There were no distant metastases.
The nasopharyngeal biopsy confirmed the diagnosis of an undifferentiated nasopharyngeal carcinoma [Type 2b (III) according to WHO]. The multidisciplinary tumor board of our institution, basing upon the endoscopic, clinical, radiological and nuclear medicine findings, staged the disease as cT1N2M0 and recommended an induction chemotherapy followed by radio-chemotherapy with a curative intent.
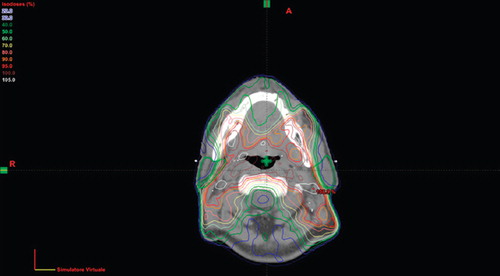
The patient received induction chemotherapy with taxanes, platinum and 5-fluoruracil, for a total of three cycles, every three weeks. The treatment was on the whole well-tolerated. After one month from the end of chemotherapy he was re-evaluated with MRI and PET that showed a good response to induction therapy. So the patient was treated definitively with IMRT using a dose-painting technique, in which the planning target volume of the gross disease and high-risk subclinical regions received 59.4 Gy at 1.8 Gy per fraction, followed by a boost of 10.8 Gy on gross disease volume. The isodose curves of cumulative dose-volume histogram (DVH) for the treatment are shown in . The average bilateral parotid dose was 19 Gy. He received concurrent chemotherapy with cisplatin at the dose of 100 mg/mq every three weeks for a total of three cycles.
Eighteen months after the end of radio- chemotherapy a MRI scan demonstrated a 16 mm nonspecific nodule within the deep lobe of the right parotid gland (). The pre-treatment imaging was reviewed without evidence of any nodule within the right parotid ( and ).
Following the recommendation of the multidisciplinary tumor board, a total parotidectomy and omolateral selective neck dissection of levels II, III, Va was performed; the pathology report showed metastatic undifferentiated carcinoma to a parotid lymph node while the neck dissection specimen was negative.
The tumor board decided not to recommend any further treatment so the patient was closely followed up. He is at present alive without disease one year after the salvage surgery.
Discussion
In patients who underwent to parotid-sparing definitive radiotherapy, the majority of local-regional recurrences are in-field [Citation8–12], that is in areas of previous disease judged to be at high risk at the time of radiotherapy planning. These findings motivate the attempt to escalate the dose to the highest risk regions. On the other hand, few cases of recurrences within the out-field regions as the spared parotid glands are reported in literature.
Disease recurrence in the region of a spared parotid gland after IMRT for head and neck cancer has been previously reported by Chao et al. [Citation13] in a patient who underwent IMRT, but in this case the recurrence occurred postoperatively after a partial pharyngectomy and neck dissection and the singular pattern of recurrence may also be explained with a postsurgical alteration of lymphatic drainage.
On one hand, in 2008, Cannon et al. [Citation14] published three cases of periparotid treatment failure in patients who underwent definitive parotid-sparing IMRT for head and neck cancer. They concluded that the presence of multiple and/or level II nodal metastases could increase the risk of subclinical disease in the parotid. In our case, at diagnosis there was a periparotid positive node, in correspondence of the inferior pole of the parotid gland, but no clear alterations within the parotid gland. Similar situations deserve careful evaluation before prescribing definitive IMRT with bilateral and even monolateral (in case of bilateral clinical nodal involvement) parotid gland sparing. Generally, ours as Cannon's cases suggest an evaluation of a paradigm shift for parotid sparing by IMRT, e.g. it may be contraindicated in the case of omolateral clinical involvement of level II nodes. On the other hand, IMRT offers several different options to preserve salivary flow, one is of course to spare only the contralateral parotid, another, in the case of bilateral involvement of level II nodes, is theoretically the sparing of the submandibular glands, which may result in good preservation of unstimulated salivary flow [Citation15]. Nevertheless, even if the submandibular gland contains no intraparenchymal lymph nodes, locoregional recurrence inside the spared gland may occur, for contiguity with an oral/oropharyngeal primary or with an involved adjacent lymph node [Citation16]. Other authors described the surgical transfer of submandibular glands outside of the radiation target volumes to preserve their function [Citation17,Citation18].
Conclusion
As reported in our patient and in similar cases in the literature, the sparing of the omolateral parotid gland can be questioned when lymphonodal metastases are close to the parotid boundaries. As an alternative solution, in order to preserve the salivary flow, a dose reduction to controlateral parotid and/or submandibular gland could be considered, if oncologically safe. It should be emphasized that the avoidance of xerostomia by IMRT cannot justify any decrease in loco-regional control.
Declaration of interest:
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Harrison L, Zelefsky M, Pfitzer D, Carper E, Raben A, Kraus DH, . Detailed quality of life assessment in patients treated with primary radiotherapy for base of tongue. Head Neck 1997;19:169–75.
- Scully C, Epstein J. Oral health care for the cancer patient. Oral Oncol 1996;32B:281–92.
- Valdez IH, Atkinson JC, Ship JA, Fox PC. Major salivary gland function in patients with radiation-induced xerostomia: Flow rates and sialochemistry. Int J Radiat Oncol Biol Phys 1993;25:41–7.
- Korsten MA, Rosman AS, Fishbein S, Shlein RD, Goldberg HE, Biener A. Chronic xerostomia increases esophageal acid exposure and is associated with esophageal injury. Am J Med 1991;90:701–6.
- Cheng JCH, Chao KSC, Low DA. Comparison of intensity modulated radiation therapy (IMRT) techniques for nasopharyngeal carcinoma. Int J Cancer 2001;96: 126–31.
- Chao KSC, Low DA, Perez CA, Purdy JA. Intensity modulated radiation therapy in head 6 neck cancers: The Mallinckrodt experience. Int J Cancer 2000;90:92–103.
- Chao KSC, Majhail N, Huang CJ, Simpson JR, Perez CA, Haughey B, . Intensity-modulated radiation therapy reduces late salivary toxicity without compromising tumor control in patients with oropharyngeal carcinoma: A comparison with conventional techniques. Radiother Oncol 2001;61:275–80.
- Lee N, Xia P, Fischbein NJ, Akazawa P, Akazawa C, Quivey JM. Intensity-modulated radiation therapy for head & neck cancer: The UCSF experience focusing on target volume delineation. Int J Radiat Oncol Biol Phys 2003;57:49–60.
- Eisbruch A, Marsh LH, Dawson LA, Bradford CR, Teknos TN, Chepeha DB, . Recurrences near base of skull after IMRT for head & neck cancer: Implications for target delineation in high neck and for parotid gland sparing. Int J Radiat Oncol Biol Phys 2004;59:28–42.
- Dawson LA, Anzai Y, Marsh L, Martel MK, Paulino A, Ship JA, . Patterns of locoregional recurrence following parotid sparing conformal and segmental intensity- modulated radiotherapy for head & neck cancer. Int J Radiat Oncol Biol Phys 2000;46:1117–26.
- Wolden SL, Chen WC, Pfister DG, Kraus DH, Berry SL, Zelefsky MJ. Intensity-modulated radiation therapy (IMRT) for nasopharynx cancer: Update of the Memorial Sloan-Kettering experience. Int J Radiat Oncol Biol Phys 2006;64:57–62.
- Daly ME, Lieskovsky Y, Pawlicki T, Yau J, Pinto H, Kaplan M, . Evaluation of patterns of failure and subjective salivary function in patients treated with intensity modulated radiotherapy for head and neck squamous cell carcinoma. Head Neck 2007;29:211–20.
- Chao KS, Ozyigit G, Tran BN, Cengiz M, Dempsey JF, Low DA. Patterns of failure in patients receiving definitive and postoperative IMRT for head and neck cancer. Int J Radiat Oncol Biol Phys 2003;55:312–21.
- Cannon DM, Lee NY. Recurrence in region of spared parotid gland after definitive intensity-modulated radiotherapy for head and neck cancer. Int J Radiat Oncol Biol Phys 2008; 70:660–5.
- Saarilahti K, Kouri M, Collan J , Kangasmäki A, Atula T, Joensuu H, . Sparing of the submandibular glands by intensity modulated radiotherapy in the treatment of head and neck cancer. Radiother Oncol 2006;78:270–5.
- Spiegel JH, Brys AK, Bhakti A, Singer MI. Metastasis to the submandibular gland in head and neck carcinomas. Head Neck 2004;26:1064–8.
- Jha N, Seikaly H, Harris J, Williams D, Liu R, McGaw T, . Prevention of radiation induced xerostomia by surgical transfer of submandibular salivary gland into the submental space. Radiother Oncol 2003;66:283–9.
- Pathak KA, Bhalavat RL, Mistry RC, Deshpande MS, Bhalla V, Desai SB, . Upfront submandibular salivary gland transfer in pharyngeal cancers. Oral Oncol 2004;40:960–3.