To the Editor,
Ipilimumab is a monoclonal antibody that specifically blocks the inhibitory signal of cytotoxic T lymphocyte antigen 4 (CTLA-4) which results in T cell activation, proliferation and lymphocyte infiltration into tumors, leading to tumor cell death. Two phase 3 trials in patients with advanced melanoma showed an improvement of overall survival. The first trial showed that ipilimumab, with or without a gp100 peptide vaccine, as compared to gp100 alone, improved overall survival in patients with previously treated metastatic melanoma [Citation1]. The second trial showed that ipilimumab in combination with dacarbazine, as compared to dacarbazine plus placebo, improved overall survival in patients with previously untreated metastatic melanoma [Citation2]. Adverse reactions of ipilimumab were most commonly the results of an increased or excessive immune activity. Most of these adverse events, including grade 3 and 4 toxicity, resolve following initiation of appropriate medical therapy or withdrawal of ipilimumab. The most common side effects (affecting more than 10% of patients) are related to skin (rash, pruritus), gastrointestinal (diarrhea, nausea, vomiting and abdominal pain) and general (fatigue, decreased appetite) side effects [Citation3]. We report a case of severe colitis caused by treatment with ipilimumab for which a colectomy was ultimately indicated. The patient fully recovered and showed a clinical and radiological response to ipilimumab.
Case report
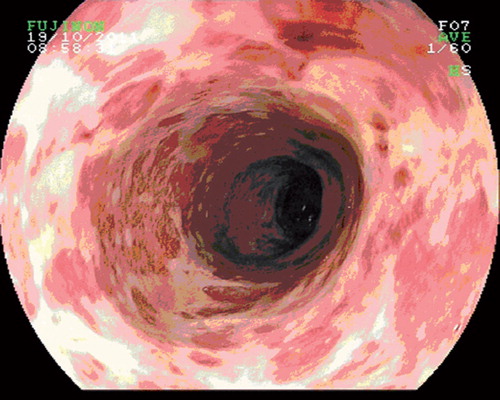
A 59-year-old female patient was referred to our hospital because of metastatic melanoma progressive under treatment with dacarbazine. Her medical history included an osteomyelitis of the leg with a brain abscess, a mastectomy because of ductal carcinoma in situ (DCIS), a transurethral resection (TUR) because of superficial bladder cancer and a nodular melanoma (Breslow's depth 8 mm, Clark level 5) on the back for which wide excision and axillary lymph node dissection was performed in July 2008. A few months before she received three courses dacarbazine because melanoma metastasis in the liver and a portocaval lymph node were diagnosed. After three courses computed tomography (CT) evaluation showed progression of the liver metastasis. We started treatment with ipilimumab 3mg/kg every three weeks in the named patient program in which a total of four courses were planned. A few days after the fourth course, she was admitted to the hospital because of grade 3 diarrhea. No pathogenic microorganisms were cultured from her feces. Colonoscopy showed a pancolitis. A biopsy showed infiltration with eosinophilic granulocytes and plasma cells in the lamina propria with cryptitis with neurophilic granulocytes; this was suggestive of an ipilimumab-induced colitis. We treated her with prednisone intravenously and mesalazine and she recovered in a couple of days. However, after two days the diarrhea started again and did not react to prednisone treatment anymore. We gave her an infusion of 5 mg/kg infliximab and she recovered. CT evaluation showed progression of the target and non-target lesions. After two and a half weeks the diarrhea started again. Again no pathogenic microorganisms were cultured from her feces and Clostridium difficile toxine was negative. We treated her with 5 mg/kg infliximab an additional two times. However, this was complicated by a necrotic fasciitis of her arm, probably evoked by a phlebitis. Since the diarrhea continued and the endoscopic inflammatory lesions did not show any sign of improvement and were not suggestive for pseudomembranous colitis, we finally decided to perform a colectomy, since she also had developed a sincere complication of the immunosuppressive therapy. (). A laparoscopic assisted subtotal proctocolectomy was performed with an ileostomy. Histopathology showed a severe mucosal colitis met with loss of crypts, ulcerative inflammation, cryptabscesses and pseudomembranes. She fully recovered afterwards within one month and restored to good clinical condition (WHO 0). CT evaluation two months after ipilimumab treatment showed decrease of both target and non-target lesions and no new lesions (according to RECIST 1.1). After five months we saw a further decrease of one target lesion with stable other lesions on CT evaluation.
Discussion
We describe a case of severe colitis induced by ipilimumab for metastatic melanoma, for which ultimately a colectomy had to be performed. Although diarrhea and colitis are both known immune related gastrointestinal events [31–46% (any grade) after a median of seven weeks of treatment], a colectomy is almost never necessary to resolve colitis [Citation4].
Based on the specific guidelines, treatment of mild diarrhea is symptomatic, with loperamide, rehydration and electrolyte substitution. For grade 2 gastro-intestinal immune-related adverse effects (irAEs), ipilimumab is suspended and budesonide, a locally acting corticosteroid with low bioavailability after oral administration, or 1 mg/kg prednisone should be started. Patients with severe diarrhea or colitis (grade ≥ 3) require high-dose steroids (e.g. methylprednisolone or dexamethasone) or, in case of no improvement after a week, infliximab, and additionally ipilimumab is permanently withheld. Refractory cases of colitis, like our case, may require ileostomy or colectomy. Treatment of gastro-intestinal irAEs according to specific guidelines is effective in reducing the occurrence of serious complications, such as perforation or colectomy, and results in 90% resolution of grade 3 or 4 events [Citation5,Citation6].
Our patient had a delayed tumor response on ipilimumab. The patterns of tumor response to ipilimumab differ from those observed with cytotoxic chemotherapeutic agents, since patients may have a delayed but yet durable response and can obtain long-term survival from the immunotherapy despite an initial tumor growth [Citation7].
Several trials have reported a possible correlation between grade 3 and 4 irAEs and clinical efficacy of ipilimumab, suggesting that tumor regression is associated with the development of autoimmunity [Citation8–10]. However, clinical benefit can still be seen also in patients who do not develop irAEs [Citation9]. Nevertheless, the association between antitumor effect and autoimmune phenomena needs to be assessed in large prospective studies. Our case is an example of a specific pattern of tumor response to ipilimumab despite a life-threatening immune-related adverse effect.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Hodi FS, O'Day SJ, McDermott DF, . Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med 2010;363:711–23.
- Robert C, Thomas L, Bondarenko I, . Ipilimumab plus dacarbazine for previously untreated metastatic melanoma. N Engl J Med 2011;364:2517–26.
- Hanaizi Z, van Zwieten-Boot B, Calvo G. The European Medicines Agency review of ipilimumab (Yervoy) for the treatment of advanced (unresectable or metastatic) melanoma in adults who have received prior therapy: Summary of the scientific assessment of the Committee for Medicinal Products for Human Use. Eur J Cancer 2012;48:237–42.
- Graziani G, Tentori L, Navarra P. Ipilimumab: A novel immunostimulatory monoclonal antibody for the treatment of cancer. Pharmacol Res Epub 2011 Sep 10.
- Lin R, Yellin MJ, Lowy I, Safferman A, Chin K, Ibrahim R. An analysis of the effectiveness of specific guidelines for the management of ipilimumab mediated diarrhea/colitis: Prevention of intestinal perforation and/or colectomy. J Clin Oncol 2008;26:9063.
- van den Eertwegh AJM, Bloemena E, Hoentjen F, van Bodegraven AA. Behandeling van auto-immuunreacties ten gevolge van een immuuntherapie met een antistof tegen CTLA-4 (ipilimumab) bij patiënten met een gemetastaseerd melanoom. Ned Tijdschr Oncol 2010;7:258–63.
- Pennock GK, Waterfield W, Wolchok JD. Patient responses to ipilimumab, a novel immunopotentiator for metastatic melanoma: How different are these from conventional treatment responses? Am J Clin Oncol Epub 2011 Feb 17.
- Beck KE, Blansfield JA, Tran KQ, Feldman AL, Hughes MS, Royal RE, . Enterocolitis in patients with cancer after antibody blockade of cytotoxic T-lymphocyte-associated antigen 4. J Clin Oncol 2006;24:2283–9.
- Attia P, Phan GQ, Maker AV, Robinson MR, Quezado MM, Yang JC, . Autoimmunity correlates with tumour regression in patients with metastatic melanoma treated with anti-cytotoxic T-lymphocyte antigen-4. J Clin Oncol 2005;23: 6043–53.
- Lutzky J, Wolchok J, Hamid O, Lebbe C, Pehamberger H, Linette G, . Association between immune-related adverse events (irAEs) and disease control or overall survival in patients (pts) with advanced melanoma treated with 10 mg/kg ipilimumab in three phase II clinical trials. J Clin Oncol 2009;27:9034.