To the Editor,
Primary bone and soft tissue sarcomas are primarily treated with surgery, chemotherapy, and radiotherapy [Citation1,Citation2]. For limb sarcoma, wide en bloc resection and limb salvage surgery is commonly performed to preserve function [Citation3]. This procedure involves reconstruction of the bony defect because limb salvage surgery requires a wide resection of bone and soft tissue. The methods of skeletal reconstruction include prosthesis implantation, allografting, and autogenous bone grafting. Autogenous bone graft has the following advantages: 1) it can be adapted to any site; 2) it does not need a bone bank; 3) it does not promote an immunologic response or viral disease transmission; 4) the size and shape approximately adapt to the bony defect; 5) preserves the ligamentous tissue attaching to bone; and 6) if bony union is completed, it can preserve the bone strength better than allografting [Citation4].
Irradiated autogenous bone grafting is a type of autogenous bone grafting. The long-term efficacy and safety of this treatment in a large number of patients remains to be elucidated. In this study, we investigated the long-term results of intraoperative extracorporeal irradiation of autogenous bone grafts on primary bone and soft tissue malignancies.
Patients and methods
Patient characteristics
We retrospectively analyzed the clinical results of 74 patients (42 patients in Osaka University Hospital and 32 patients in Osaka Medical Center for Cancer and Cardiovascular Diseases) between 1988 and 2012. All patients were diagnosed by imaging and biopsies. Median follow-up interval after definitive surgery was 75 months (range 6–240 months).
The average age at the time of surgery was 29 years (range 5–76). The most common histologic type was osteosarcoma (39 patients, 53%) and the second was chondrosarcoma (8 patients, 11%). The disease sites included 54 lower limbs, 17 upper limbs, two pelvises, and one clavicle. The graft types included osteoarticular in 29 cases, intercalary in 18 cases, composite with endoprosthesis in 17 cases, and hemicortical in 10 cases. Stage IIA of the disease as per the TNM classification was most common among the patients, and five patients had distant metastases.
Treatment
Surgery consisted of four procedures. First, the bone affected by the tumor was resected using a wide margin. Second, curettage of the tumor tissue from the resected bone was performed. The ligaments and tendons were preserved for the possibility of reconstruction. Third, the bone was irradiated using Liniac with 6 or 10-MV photons. The irradiation dose in one fraction was 50 Gy for 71 patients, 60 Gy for one patient, and 80 Gy for two patients. Finally, the irradiated autogenous bone was reimplanted into the remaining bone with intramedullary rods, plates, or both.
Fifty-seven patients were intravenously or intra-arterially administered preoperative and/or postoperative anticancer agents. The NCI’s Common Terminology Criteria for Adverse Events (CTCAE) version 4.0 is the preferred method for capturing adverse events.
Functional criteria
We evaluated postoperative function until the time of the last follow-up according to the Musculoskeletal Tumor Society (MSTS) graft evaluation system [Citation5].
Statistical analysis
Disease-specific survival rate and the survivorship of the irradiated bone were actuarially calculated according to the Kaplan-Meier method. The survivorship of the irradiated bone was considered from the date of implantation to the date of the last follow-up or to the removal of all or part of the bone because of complication or recurrence.
Results
Local control and disease-specific survival
Treatments were safely performed in all 74 patients. No patient experienced a local recurrence within the irradiated field, although there were three local recurrences outside the reimplanted bones. Two patients were treated with amputations, and the other patient underwent irradiated bone removal and total femur replacement. Two patients received postoperative chemotherapies. They were all alive without a second recurrence at the time of last follow-up. Distant metastases were detected in 13 patients, with the most common site being the lung in 10 patients. Five- and 10-year disease-specific survival rates were 94% and 86%, respectively ().
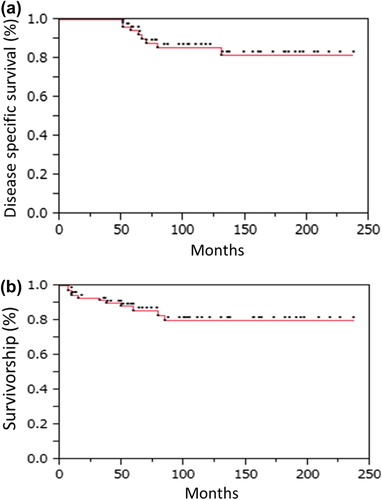
The irradiated grafts were removed in 11 patients due to complications or local recurrences outside the irradiated bone grafts. The survivorship of the irradiated bone was 86% at five years and 80% at 10 years ().
Adverse events
The major complications of the irradiated autogenous bone grafting were infections, fractures, and non-unions. Infections occurred in 13 events (18%). Surgical debridement was performed for 11 events corresponding to Grade 3, and antibiotics were administered in the other two events. For three events, all or part of the radiated bones was removed. Thirteen fractures occurred within the irradiated bone grafts in eight patients and outside of the grafts in four patients. The key images in the remaining one patient were missing. Surgery was performed for 10 events corresponding to Grade 3, and three grafts were removed. Most of the fractures were caused by a fall or vigorous exercises. Non-union occurred in 12 events, and all of them underwent a follow-up examination. Two grafts were retrieved due to other adverse events (one collapse and one plate breakage). Irradiated grafts were removed in eight patients (11%) because of complications. Grade 3 complications occurred in 35 patients (40 events), but there were no Grade 4 or 5 complications. Although 35 of the 40 Grade 3 complications required surgical interventions after the initial treatment, all patients lived normal daily lives following the intervention. Reoperation rate was 47% (35 patients).
Functional results
In our study, the average MSTS score was 21 (range 9–30). The average score of pain was 4.5, indicating that most patients experienced little pain. The average score of function was 3.4, suggesting that patients experienced some restriction in recreational activity but could live normal daily lives.
Discussion
Although previous reports used varying radiation doses ranging from 50 to 300 Gy [Citation6,Citation7], an optimal dose for irradiation of autogenous bone grafts has not yet been determined. We selected 50 Gy in one fraction for all except three cases because this dose achieved complete tumor sterilization in previous research [Citation8]. The remaining three cases received higher doses because they were radiation-resistant sarcomas, such as chondrosarcomas [Citation9]. We did not observe any local recurrences within the irradiated autogenous bones in the current study, suggesting that 50 Gy in one fraction was a dose high enough to eradicate all sarcoma cells.
For limb salvage surgery, prosthetic replacement is the most common and widely accepted reconstructive method. However, as many as 10–20% of patients who received prosthetic replacement surgery require amputation due to a complication or local recurrence [Citation10,Citation11]. The overall survivorship of prosthesis is 35–71% at 10 years in previous studies [Citation11–13], while we found that the survivorship of irradiated bone was 80% at 10 years. Therefore, the irradiated bone graft may be less troublesome compared with the prosthetic replacement once it has healed, particularly after long-term follow-up.
Infection, fracture, and non-union are common and severe adverse complications. The incidence rates of irradiated bone grafting, prosthetic replacement, or allografting were consistent with others [Citation14–18].
A few studies have investigated functionality following limb salvage surgery, with the average MSTS scores ranging from 19 to 26 [Citation17–19]. Our average functional score of 21 is comparable with that of previous findings.
Epidemiology about primary bone and soft tissue sarcoma illustrates that the peak incidence occurs between teens and 20 year olds. Recent advances in multimodality treatment increases the long-term survival rate to more than 70% at 10 years. Due to the long-term effectiveness and safety of irradiated bone grafting, this treatment may be a suitable option for young patients. However, reoperation rate following this method was high (47%) in our study, and according to Araki's study, the irradiated osteoarticular bone grafting was not favorable in the weight-bearing knee joint because it is more likely to collapse [Citation12]. In addition, it may not be a viable option for infants with a persistent growth plate because the growth plate will be disconnected and slipped.
In conclusion, the reconstruction of the intraoperative extracorporeal irradiation of autogenous bone graft is a safe and effective treatment for primary bone and soft tissue malignancies.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Pisters PWT, O’Sullivan B, Maki RG. Evidence-based recommendations for local therapy for soft tissue sarcomas. J Clin Oncol 2007;25:1003–8.
- Mendenhall WM, Indelicato DJ, Scarborough MT, Zlotecki RA, Gibbs CP, Mendenhall NP, et al. The management of adult soft tissue sarcomas. Am J Clin Oncol 2009;32:436–42.
- Pakos EE, Nearchou AD, Grimer RJ, Koumoullis HD, Abudu A, Bramer JAM, et al. Prognostic factors and outcomes for osteosarcoma: An international collaboration. Eur J Cancer 2009;45:2367–75.
- Wheeler DL, Enneking WF. Allograft bone decreases in strength in vivo over time. Clin Orthop Relat Res 2005; 435:36–42.
- Enneking WF, Dunham W, Gebhardt MC, Malawar M, Pritchard DJ. A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clin Orthop Relat Res 1993;286:241–6.
- Spira E, Lubin E. Extracorporeal irradiation of bone tumors. A preliminary report. Isr J Med Sci 1968;4:1015–9.
- Davidson AW, Hong A, McCarthy SW, Stalley PD. En-bloc resection, extracorporeal irradiation, and re-implantation in limb salvage for bony malignancies. J Bone Joint Surg Br 2005;87:851–7.
- Araki N, Myoui A, Kuratsu S, Hashimoto N, Inoue T, Kudawara I, et al. Intraoperative extracorporeal autogenous irradiated bone grafts in tumor surgery. Clin Orthop Relat Res 1999;368:196–206.
- Moussavi-Harami F, Mollano A, Martin JA, Ayoob A, Domann FE, Gitelis S, et al. Intrinsic radiation resistance in human chondrosarcoma cells. Biochem Biophys Res Commun 2006;346:379–85.
- Myers GJC, Abudu AT, Carter SR, Tillman RM, Grimer RJ. Endoprosthetic replacement of the distal femur for bone tumours: Long-term results. J Bone Joint Surg Br 2007;89:521–6.
- Grimer RJ, Carter SR, Tillman RM, Sneath RS, Walker PS, Unwin PS, et al. Endoprosthetic replacement of the proximal tibia. J Bone Joint Surg 1999;81:488–94.
- Tan PX, Yong BC, Wang J, Huang G, Yin JQ, Zou CY, et al. Analysis of the efficacy and prognosis of limb-salvage surgery for osteosarcoma around the knee. Eur J Surg Oncol 2012;38:1171–7.
- Myers GJC, Abudu AT, Carter SR, Tillman RM, Grimer RJ. The long-term results of endoprosthetic replacement of the proximal tibia for bone tumours. J Bone Joint Surg Br 2007;89:1632–7.
- Poffyn B, Sys G, Mulliez A, Van Maele G, Van Hoorebeke L, Forsyth R, et al. Extracorporeally irradiated autografts for the treatment of bone tumours: Tips and tricks. Int Orthop 2011;35:889–95.
- Mankin HJ, Springfield DS, Gebhardt MC, Tomford WW. Current status of allografting for bone tumors. Orthopedics 1992;15:1147–54.
- Farfalli GL, Aponte-Tinao L, Lopez-Millán L, Ayerza MA, Muscolo DL. Clinical and functional outcomes of tibial intercalary allografts after tumor resection. Orthopedics 2012;35:e391–6.
- Puri A, Gulia A, Jambhekar N, Laskar S. The outcome of the treatment of diaphyseal primary bone sarcoma by resection, irradiation and re-implantation of the host bone: Extracorporeal irradiation as an option for reconstruction in diaphyseal bone sarcomas. J Bone Joint Surg Br 2012;94:982–8.
- Kim J-D, Lee GW, Chung SH. A reconstruction with extracorporeal irradiated autograft in osteosarcoma around the knee. J Surg Oncol 2011;104:187–91.
- Abudu A, Grimer RJ, Tillman RM, Carter SR. Endoprosthetic replacement of the distal tibia and ankle joint for aggressive bone tumours. Int Orthop 1999;23:291–4.
