Abstract
Background. The precise etiology of fecal incontinence (FI), which occurs frequently following external beam radiotherapy (EBRT) for prostate carcinoma is unknown. It is possibly related to pelvic nerve injury. The aim of this study was to assess the incidence of pudendal nerve dysfunction in men with FI after EBRT for prostate cancer compared to men with FI but no history of EBRT.
Material and methods. Data were evaluated from 74 men with intact anal sphincters on endo-anal ultrasound (17 post-EBRT) who had been investigated for FI at a tertiary center. Wexner incontinence scores, pudendal nerve function, anorectal manometry, and rectal sensitivity were compared between the two patient groups.
Results. Post-radiotherapy patients were older (77 ± 6 vs. 62 ± 17 years, p < 0.005) and had worse incontinence than those with no history of radiotherapy (Wexner score; 13 ± 3 vs. 8 ± 4; p < 0.005). Bilateral pudendal nerve terminal motor latency (PNTML) was abnormal in 87% of radiotherapy versus 22% of non-radiotherapy patients (p < 0.001) and the significant difference persisted even after correction for age differences. Anal sphincter pressures and rectal sensitivity for both groups were similar.
Conclusion. There is a markedly higher incidence of pudendal nerve dysfunction in men with FI after EBRT for prostate cancer compared with men with FI from other etiologies. The increased severity of incontinence in radiotherapy patients is not matched by alterations in either anal sphincter pressures or rectal sensitivity compared to FI in non-ERBT patients.
Carcinoma of the prostate is a significant cause of mortality and morbidity in men [Citation1]. External beam radiotherapy (EBRT) is a well established treatment modality for locally advanced prostate carcinoma and is associated with a 50% reduction in the 10-year prostate cancer mortality [Citation2]. Planning and delivery of EBRT has evolved to improving targeting of tumor irradiation while minimizing exposure to surrounding organs [Citation3] but inclusion of a part of the rectum and anal canal cannot be avoided in the radiation field. Thus, patients frequently report anorectal sequelae, such as increased stool frequency, fecal urgency, fecal incontinence (FI) and rectal bleeding [Citation4,Citation5]. FI in particular is a significant complication of EBRT because it leads to major impairment of patient quality of life, is persistent and is refractory to treatment [Citation6]. Previously the incidence of anorectal symptoms has been largely underestimated but recent data shows the incidence of soiling and FI post-EBRT for prostate cancer to be over 50% even three years post-radiotherapy [Citation5].
The mechanisms underlying FI after radiotherapy for carcinoma of the prostate remain incompletely understood, but both external anal sphincter (EAS) and internal anal sphincter (IAS) dysfunction are considered important [Citation7]. In addition, decreased rectal compliance, reflecting increased rectal wall stiffness and reduced rectal capacity may also have a role [Citation8].
The etiology of anorectal dysfunction after radiotherapy is unclear. The pelvic nerves and their branches, have a major role in regulation of motor, sensory and autonomic activity in the anorectum. As the pudendal nerve innervates the EAS and IAS, radiation damage could contribute to the development of FI in these patients. Pudendal nerve dysfunction has been implicated in the pathogenesis of FI from other etiologies [Citation9] but neural structures, such as the pudendal nerve, which are outside the high dose radiation field have been considered relatively resistant to radiation injury. The possible contribution of pudendal nerve injury to FI incontinence post-radiotherapy has therefore received limited attention. However, recent data reporting neural dysfunction after radiotherapy for rectal carcinoma suggest that moderately high dose radiation may impact directly on neural activity [Citation10].
We therefore assessed pudendal nerve function, along with incontinence severity, and anorectal motor and sensory function in men with FI who had previously undergone EBRT. The incontinence severity, neural and anorectal function data were compared with that of men with FI who had not undergone EBRT as a control group.
Material and methods
Study population
A prospectively collected database was interrogated to determine all patients with FI (n = 1305) who had undergone anorectal manometry at the tertiary institution between January 1998 and November 2013. In total 114 men had been investigated for FI with pudendal nerve terminal motor latency (PNTML) testing, and anorectal manometry. Thirty-six patients were excluded from the analysis due to a structural defect in the anal sphincter (n = 34) or incomplete evaluation (n = 2) on standardized endoanal ultrasound. A further four men who had radiotherapy for causes other than prostate cancer were also excluded. Of the remaining 74 men, 17 had previously undergone EBRT for prostate carcinoma while 57 had no history of radiation treatment ().
Patient characteristics
The patient age, etiology of symptoms and duration of symptoms prior to testing were recorded along with any prior history of anorectal surgery. Incontinence severity was assessed using the Wexner incontinence score [Citation11].
Pudendal nerve terminal motor latency (PNTML)
PNTML assessment was performed by trained colorectal surgeons using a disposable glove-mounted St Mark's electrode and a transrectal nerve stimulation technique (13L40 St Mark's Pudendal ElectrodeTM, Medtronic Functional Diagnostics A / S, Skovlunde, Denmark). Square wave stimuli of 0.05 ms duration and 10 mA were delivered at one-second intervals. The electromyography (EMG) recordings were acquired via a MacLab or PowerLab 8S or 4S system with a MacLab or PowerLab bioamplifier using ScopeTM (V3.4.3-4.1) software (ADInstruments Pty. Ltd, Castle Hill, NSW, Australia). Multiple recordings were taken on each side and the most well defined action potentials selected for the determination of the latency. The mean latency from these multiple curves was determined. Latency was defined as the time between the stimulation of the pudendal nerve at the level of the ischial spine and commencement of depolarization of the anal sphincter [Citation12]. The stimulus artefact (recorded electrical pulse) was clearly visible as evidence of correct technical functioning of the recording technique. A lack of pudendal nerve response was defined as no sphincter contraction or EMG recording in response to stimulus ().
Anorectal motility
Patients who had received radiotherapy underwent anorectal testing at a mean interval of 8.3 ± 5.1 (range 3–18) years post-EBRT. Manometry was performed in the left lateral position, in an unprepared bowel. The water-perfused, three-channel catheter (external diameter 3.0 mm) (Dentsleeve Pty. Ltd, Adelaide, Australia or Mui Scientific, Ontario, Canada) was attached to three pressure transducers (Sorrenson Transpac Abbot Critical Care Systems, IL, USA). Each channel had a side hole, and the side holes were arranged circumferentially, 120° to each other and 5 mm apart. Data were recorded with a MacLab or PowerLab recording system with a Maclab or PowerLab bridge amplifier using ChartTM (V3.4.3-V7.0.1) software (ADInstruments Pty. Ltd, Castle Hill, NSW, Australia) and a MacIntoshTM computer (Apple Computer Inc., Cupertino, CA, USA).
A station pull-through technique using a standard protocol was used with the catheter pulled through the anal canal at regular intervals with pressure recordings taken at each station. The mean maximal resting (MRP) and squeeze (MSP) pressures of the three channels were determined as previously described [Citation12].
Rectal capacity and time to first rectal sensation were assessed using a low compliance balloon inserted into the rectum. This was inflated with air to fixed volumes for one minute then deflated (volumes of 10, 20, 40, 70, 100, 150 and 200 mls were used). The patient reported the first sensation of the balloon, and maximal tolerated volume. The presence of the recto-anal inhibitory reflex (RAIR) was recorded.
Modeling of radiation dose distributions based on available 3D CT planning scans and radiation dose prescriptions
Of the 17 patients constituting the radiotherapy group in this study, 16 received radiotherapy as primary treatment for localized (T1, T2 N0 M0) prostate carcinoma and one patient was treated by salvage radiotherapy for recurrent disease after radical prostatectomy. The radiotherapy received by the whole patient group between 1995 and 2010 was delivered in 14 of the 17 patients using a 23 MV photon four rectangular (AP/PA and laterals) field with a two-dimensional (2D) no shielding technique to encompass the prostate target [top left digitally reconstructed radiograph (DRR), ] to a total dose of 66 Gy prescribed to the isocenter in 2 Gy fractions treating 5×/week as 3D conformal radiotherapy did not become available at the affiliated radiation oncology facilities until 2003. Two of the 3D patients also receiving radiotherapy as primary treatment were treated to a total dose of 74 Gy in 2 Gy fractions treating 5×/week using a 23 MV five-field (anterior, APO, PAO and laterals) 3D technique with multileaf collimators to shape the fields around the prostate target (Top right DRR, ). The patient treated by salvage radiotherapy for recurrent prostate carcinoma after radical prostatectomy received 3D conformal radiotherapy which first targeted the lesser pelvic lymph nodes to a dose of 45 Gy in 25 fractions treating 5×/week (Bottom right DRR, ) followed by a boost to the prostate bed of 16.2 Gy in 9 fractions treating 5×/week (Bottom left DRR, ) using a 23 MV photon four-field (AP/PA and laterals) multi-collimated technique for both target volumes.
Figure 3. Relationship of the pudendal nerve (in green) with the target volumes (in blue) encompassed by the digitally reconstructed radiograph of the right lateral field corresponding to the simulated 2D (top left) and simulated 3D (top right) plans and actual 3D plan of the patient treated to the lesser pelvic nodes (bottom right) with a boost to the prostate bed (bottom left).
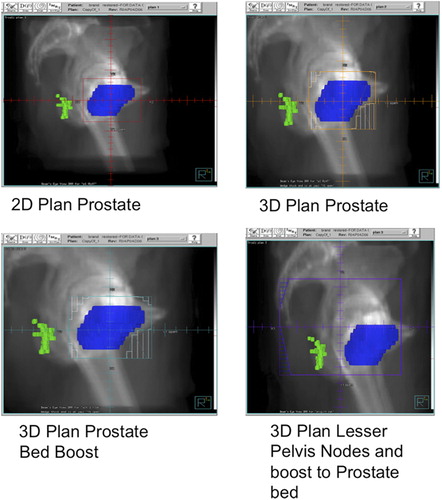
As the CT planning scans of the two of the three 3D conformal radiotherapy patients were not able to be retrieved and treatment planning in the 14 patients treated by the 2D technique was based on orthogonal (AP and lateral) treatment simulator localization films, the treatment plans of these 16 patients were based on the CT planning data of the patient treated for recurrent prostate carcinoma after radical prostatectomy downloaded on the 3D (ADAC Pinnacle) computer system. The dose volume parameters of the prostate and organs at risk (OARs), such as the rectum (contoured as a solid organ), anal canal (also contoured as solid organ from the anal verge to the anorectal junction just below the pubo-rectalis sling around the posterior wall of the rectum) and pudendal nerve were derived from the 3D planning system using the prostate bed volume of the patient treated for recurrent prostate carcinoma but adjusting the dose prescriptions (as specified in paragraph above) for the 14 2D patients and for the two 3D patients with missing CT planning data ( and ). Thus whilst the radiation dose parameters to prostate target and OARs in and represent simulated data, represent the actual data of the patient treated for recurrent prostate carcinoma after radical prostatectomy.
Table Ia. Effect on dose parameters of anal canal, rectum, pudendal nerve and prostate of 2D plan using 4 rectangular fields (AP/PA and laterals) targeting prostate to 66 Gy at isocentre in 33 fractions treating 5x/week in 14 patients.
Table Ib. Effect on dose parameters of anal canal, rectum, pudendal nerve and prostate of 3D plan using 5-field conformal technique targeting prostate to 74 Gy at isocenter in 37 fractions treating 5x/week in 2 patients.
Table Ic. Effect on dose parameters of anal canal, rectum, pudendal nerve and prostate of 3D plan using 4-field (AP/PA and laterals) conformal technique targeting lesser pelvic nodes to 45 Gy at isocenter in 25 fractions followed by boost to prostate bed for an additional 16.2 Gy at isocenter in 9 fractions treating 5x/week in 1 patient.
Statistical analysis
Data analyzed with SPSSTM (IBM Corp. Released 2010. IBM SPSS Statistics for Windows, Version 19.0 Armonk, NY, USA) were compared between the radiotherapy and non-radiotherapy groups. Due to the significant age difference between the radiotherapy and non-radiotherapy groups, a sub-group analysis was performed to compare data from the non-radiotherapy patients older than 67 (n = 27) with that from radiotherapy patients.
The ages, mean PNTML, MRP and MSP, rectal capacity and RAIR were compared between groups using ANOVA. χ2-test was used to examine differences between PNTML groups and Wexner incontinence scores were compared using Mann-Whitney U-test. Data are mean± SD. A p-value of < 0.05 was considered statistically significant in all analyses
Results
Demographics
FI patients who had undergone EBRT were older compared to those who had not received radiotherapy ().
Table II. Patient demographics and previous surgical procedures. * p < 0.005.
There was no difference in the incidence of previous anorectal surgical procedures between the two groups ().
Symptoms
Wexner incontinence scores were recorded in 35 of the 57 men (61.4%) in the non-radiotherapy and 14 of the 17 men (82.3%) in the radiotherapy group. Patients who had received ERBT had more severe incontinence compared to other patients with FI (). Age had no effect on incontinence severity with the Wexner incontinence scores remaining significantly higher in the radiotherapy patients after matching for age (13 vs. 9, p < 0.05, data not shown).
Pudendal nerve terminal motor latency (PNTML)
Normal ranges for PNTML (1.4–2.6ms) have been defined in a previous study from our unit [Citation13]. Data for PNTML were available for 16/17 (94.1%) patients in the radiotherapy group and 46/57 (80.7%) patients in the non-radiotherapy group.
There was no unilateral or bilateral pudendal nerve response in 10/16 radiotherapy patients (62.5%) compared to 3/46 (6.5%) patients in the non-radiotherapy group (p < 0.001, ). A further four patients (25.1%) in the radiotherapy group had delayed bilateral or unilateral PNTML responses compared to seven (15.2%) in the non-radiotherapy group (p < 0.001, ). Only two patients (12.5%) in the radiotherapy group had normal bilateral PNTML compared to 36 (78.3%) in the non-radiotherapy group (p < 0.001, ).
Table III. PNTML measurements; Normal range for PNTML is 1.4–2.6 ms. * p < 0.001.
Matching for age, there was no unilateral or bilateral pudendal nerve response in 10/16 EBRT patients (62.5%) compared to one patient (1 of 27 older than 67 years; 3.7%) in the non-radiotherapy group (p < 0.001, data not shown).
Anorectal manometry
Although mean resting pressure in the radiotherapy group was within the normal range for our laboratory (54–124 cm H20) it was significantly lower compared to non-radiotherapy patients (55 ± 29 cm H20 vs. 83 ± 35.4 cm H20, p < 0.05).
Similarly the MSP in the radiotherapy group was also within the normal range (normal range 179–317 cm H20) but was significantly lower compared to the non-radiotherapy group (189.6 ± 94.5 cm H20 vs. 245.8 ± 74.7 cm H20, p < 0.05). However, when the radiotherapy group was compared to age-matched non-radiotherapy patients, no differences were found between mean resting pressures (55 ± 29 cm H20 vs. 63.2 ± 26.3 cm H20, p = NS) or MSPs (189.6 ± 94.5 cm H20 vs. 223.8 ± 70.1 cm H20, p = NS).
In the 10 post-radiotherapy patients with absent pudendal nerve responses both mean resting pressure and MSP were below the normal range but were not significantly different from pressures in post-radiotherapy patients with delayed or normal PNTML ().
Table IV. MSP and MRP in the radiotherapy group subdivided by PNTML. p = NS. * below normal range.
Rectal capacity and recto-anal inhibitory reflex
There was no difference in the volume to stimulate the recto-anal inhibitory reflex between the radiotherapy and non-radiotherapy groups. There was no significant difference in either rectal capacity (maximum tolerated rectal volume) or rectal sensitivity (volume to first perception) between radiotherapy and the non-radiotherapy groups ().
Table V. Recto-anal inhibitory index (RAIR), volume to first rectal sensation and maximum tolerated rectal volume in the radiotherapy and non-radiotherapy groups. p = NS.
Actual and simulated radiation dose distributions
Despite the higher dose to the prostate, the mean radiation doses to the OARs were lower in the patients treated with 3D conformal radiotherapy compared with the 2D technique (Table Ia and b). Interestingly, as shown in and , the mean dose to the pudendal nerve closely parallels the mean dose to the anal canal and the mean anal dose for these 2D and 3D patients based on the modeled treatment plans was well below the 40 Gy suggested as a dose constraint by Alsadius et al. [Citation14]. In contrast, both the suggested dose constraint for the anal canal and the generally accepted pudendal nerve tolerance (mean and maximum) dose were approached based on the actual dose distributions of the patient treated for recurrent disease after radical prostatectomy (). This patient had FI and abnormalities of pudendal nerve function.
Discussion
The study data show that men with FI following radiotherapy for carcinoma of the prostate have a far higher incidence of pudendal nerve dysfunction (manifest as absent or significantly delayed PNTML) than men with FI from other causes. The data also show an increased severity of FI in the post-EBRT patients. While post-radiation patients had lower resting and squeeze pressures, these were still within the normal range and when compared to age matched non-radiotherapy patients no differences were observed. This suggests the reduction in resting and squeeze pressures is likely to be an age-related phenomenon [Citation15,Citation16]. There were also no differences in rectal sensation or the recto-anal inhibitory reflex between the groups.
The major new finding in the current study is the demonstration of severe pudendal nerve injury in patients after radiotherapy. In fact, the majority of patients in the radiotherapy group had no pudendal nerve response to stimulation, i.e. there was a stimulus artifact but no muscle contraction. This suggests that the nerve is still intact, as a stimulus artifact is recorded, and resting and squeeze pressures though below the normal range for these 10 patients were not significantly different from the pressures in the radiotherapy sub-group with delayed or normal PNTML. However, as the EMG cannot be recorded together with the attenuation of both the resulting resting and squeeze pressures indicates a significant impairment of neural function. Acute pudendal nerve injury after radiotherapy has been reported after combined chemo-radiotherapy for rectal carcinoma where the bowel wall is directly targeted. In this study, PNTML tested before and four weeks after completion of chemo-radiation treatment showed a significant increase in the number of patients with delayed PNTML associated with new onset incontinence and reduction in maximal squeeze but not resting sphincter pressures [Citation10]. However, this has not been previously been demonstrated after radiotherapy for prostate cancer.
Earlier studies have shown both acute and chronic compromise of anorectal function after EBRT [Citation17,Citation18]. In this study we were unable to show a significant effect of EBRT on anal sphincter pressures. Thus there appears little correlation between anal sphincter function and FI severity in our study. A previous study has shown that 44% of men with FI had normal anal sphincter resting and squeeze pressures [Citation15]. Another study demonstrated that there was no correlation between incontinence severity and sphincter pressures in men; all incontinent males had normal resting and squeeze pressures [Citation19].
Previously studies after EBRT have also described abnormal sensory function, with reduced compliance and hypersensitivity to rectal distension in addition to lower anal sphincter pressures [Citation8,Citation18,Citation20]. However, we were unable to demonstrate this in the current study. These differences may be related to small sample size in the radiotherapy group and methodological factors. This and a previously reported study [Citation18] measured sensation and compliance using an air-filled balloon in comparison to an electronic barosat in another previously reported study [Citation8].
To date the mechanisms underlying decreased sphincter pressures after radiotherapy remains unknown [Citation7,Citation17,Citation20]. Although direct radiation- induced damage to the internal and EAS has been proposed as a mechanism, endo-anal ultrasound suggests the morphology of these structures is maintained after EBRT [Citation20]. While the current data indicates pudendal nerve injury after EBRT this did not seen to significantly correlate with anorectal dysfunction. The reasons for this discrepancy are unclear.
The level at which the pudendal nerve injury might occur is also not evident from the current study as the nerve could be damaged anywhere along its path including the neuro-muscular terminals. The course of the pudendal nerve lies outside the targeted field of radiation [top and bottom left and top right DRRs, ] except for the patient who received 45 Gy in 25 fractions treating 5×/week to the lesser pelvis nodes (bottom right DRR, ) as part treatment of local recurrence after radical prostatectomy. This dose fractionation is the same as the study reporting delayed PNTL after chemoradiation for rectal carcinoma [Citation15] and approaches radiation tolerance for peripheral nerves.
The process of defecation is complex and involves both anorectal and colonic mechanisms. The involvement of sigmoid colon motility patterns in the maintenance of continence has been recently reported [Citation21] and colonic dysmotility has been implicated in the pathogenesis of incontinence after EBRT [Citation22]. It is therefore possible that the nerve damage is manifest in other regions of the distal colon.
There are several limitations in this study. The small sample size may have contributed to the lack of difference in sensation between the groups. However, this was a secondary aim as the major focus of the study was to assess the PNTML in these patients. Furthermore, the study was retrospective and patients did not undergo anorectal physiology testing prior to radiotherapy. Thus future prospective studies are required to confirm these findings and are planned to include endoscopy to assess for radiation proctitis, endoluminal ultrasound, anorectal physiology and PNTML as well as colonic motility studies. The mean time delay of eight years to presentation is evidence of the need for such studies to have prolonged follow-up.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Baade PD, Youlden DR, Cramb SM, Dunn J, Gardiner RA. Epidemiology of prostate cancer in the Asia-Pacific region. Prostate Int 2013;1:47–58.
- Widmark A, Klepp O, Solberg A, Damber JE, Angelsen A, Fransson P, et al. Endocrine treatment, with or without radiotherapy, in locally advanced prostate cancer (SPCG-7/SFUO-3): An open randomised phase III trial. Lancet 2009; 373:301–8.
- Zlotecki RA. External-beam radiotherapy in the management of carcinoma of the prostate. Cancer Control 2001; 8:503–10.
- al-Abany M, Helgason AR, Cronqvist AK, Svensson C, Wersall P, Steineck G. Long-term symptoms after external beam radiation therapy for prostate cancer with three or four fields. Acta Oncol 2002;41:532–42.
- Heemsbergen WD, Hoogeman MS, Hart GA, Lebesque JV, Koper PC. Gastrointestinal toxicity and its relation to dose distributions in the anorectal region of prostate cancer patients treated with radiotherapy. Int J Radiat Oncol Biol Phys 2005;61:1011–8.
- Maeda Y, Hoyer M, Lundby L, Norton C. Faecal incontinence following radiotherapy for prostate cancer: A systematic review. Radiother Oncol 2011;98:145–53.
- Yeoh EK, Holloway RH, Fraser RJ, Botten RJ, Di Matteo AC, Butters J. Pathophysiology and natural history of anorectal sequelae following radiation therapy for carcinoma of the prostate. Int J Radiat Oncol Biol Phys 2012;84:e593–9.
- Krol R, Hopman WP, Smeenk RJ, Van Lin EN. Increased rectal wall stiffness after prostate radiotherapy: Relation with fecal urgency. Neurogastroenterol Motil 2012;24: 339–e166.
- Loganathan A, Schloithe AC, Hakendorf P, Liyanage CM, Costa M, Wattchow D. Prolonged pudendal nerve terminal motor latency is associated with decreased resting and squeeze pressures in the intact anal sphincter. Colorectal Dis 2013;15:1410–5.
- Lim JF, Tjandra JJ, Hiscock R, Chao MW, Gibbs P. Preoperative chemoradiation for rectal cancer causes prolonged pudendal nerve terminal motor latency. Dis Colon Rectum 2006;49:12–9.
- Vaizey CJ, Carapeti E, Cahill JA, Kamm MA. Prospective comparison of faecal incontinence grading systems. Gut 1999; 44:77–80.
- Bright T, Kapoor R, Voyvodich F, Schloithe A, Wattchow D. The use of a balloon catheter to improve evaluation in anorectal manometry. Colorectal Dis 2005;7:4–7.
- Voyvodic F, Rieger NA, Skinner S, Schloithe AC, Saccone GT, Sage MR, et al. Endosonographic imaging of anal sphincter injury: Does the size of the tear correlate with the degree of dysfunction? Dis Colon Rectum 2003;46:735–41.
- Alsadius D, Hedelin M, Lundstedt D, Pettersson N, Wilderang U, Steineck G. Mean absorbed dose to the anal-sphincter region and fecal leakage among irradiated prostate cancer survivors. Int J Radiat Oncol Biol Phys 2012;84: e181–5.
- McHugh SM, Diamant NE. Effect of age, gender, and parity on anal canal pressures. Contribution of impaired anal sphincter function to fecal incontinence. Dig Dis Sci 1987; 32:726–36.
- Gundling F, Seidl H, Scalercio N, Schmidt T, Schepp W, Pehl C. Influence of gender and age on anorectal function: Normal values from anorectal manometry in a large caucasian population. Digestion 2010;81:207–13.
- Yeoh EK, Russo A, Botten R, Fraser R, Roos D, Penniment M, et al. Acute effects of therapeutic irradiation for prostatic carcinoma on anorectal function. Gut 1998;43:123–7.
- Yeoh EE, Holloway RH, Fraser RJ, Botten RJ, Di Matteo AC, Moore JW, et al. Anorectal dysfunction increases with time following radiation therapy for carcinoma of the prostate. Am J Gastroenterol 2004;99:361–9.
- Paramor KA, Ibrahim QI, Sadowski DC. Clinical para-meters and symptom severity in males with fecal leakage and incontinence. Neurogastroenterol Motil 2014;26: 361–7.
- Yeoh EK, Holloway RH, Fraser RJ, Botten R, Di Matteo A, Moore JW, et al. Anorectal function after three- versus two-dimensional radiation therapy for carcinoma of the prostate. Int J Radiat Oncol Biol Phys 2009;73:46–52.
- Patton V, Wiklendt L, Arkwright JW, Lubowski DZ, Dinning PG. The effect of sacral nerve stimulation on distal colonic motility in patients with faecal incontinence. Br J Surg 2013;100:959–68.
- Yeoh EK, Bartholomeusz DL, Holloway RH, Fraser RJ, Botten R, Di Matteo A, et al. Disturbed colonic motility contributes to anorectal symptoms and dysfunction after radiotherapy for carcinoma of the prostate. Int J Radiat Oncol Biol Phys 2010;78:773–80.