Abstract
Backround. Operative treatment of traumatic rotator cuff ruptures, i.e. ruptures with a predisposing traumatic event, is reported to yield superior results compared to operative treatment of non-traumatic, degenerative ruptures.
Aim. The purpose of this study was to evaluate the difference of outcome, peroperative findings, and demographics after operative treatment of traumatic versus non-traumatic rotator cuff rupture.
Methods. A total of 306 consecutive shoulders with an operated rotator cuff rupture (124 traumatic and 182 non-traumatic) were followed up. Constant and Murley score, size of the rupture, and age of the patients were used as an outcome measure.
Results. A total of 112 traumatic and 167 non-traumatic rotator cuff rupture shoulders were available for 1-year follow-up (91%). Mean Constant and Murley score was preoperatively lower in the traumatic group (46 versus 52, P = 0.01). At 3 months postoperatively, Constant and Murley scores were 61 and 60 (P = 0.72) and at 1 year 73 and 77 (P = 0.03), respectively. Altogether 91% of the patients in the traumatic and 93% in the non-traumatic group were satisfied with the final outcome (P = 0.45). In 94% of traumatic and 95% of a non-traumatic cases the rupture involved the supraspinatus tendon. In the traumatic group the rupture was larger and involved more frequently the whole supraspinatus insertion area (41% versus 17%, P < 0.0001). Mean age of patients was 58 and 57 years, respectively.
Conclusion. Operative treatment of both traumatic and non-traumatic rotator cuff ruptures gives essentially good results. In our cohort, patients' recollection of predisposing trauma reflects the size of the rotator cuff rupture, but does not reflect the age of the patients.
Introduction
A rotator cuff rupture may result from a distinct extrinsic trauma, for example due to falling (Citation1), or it may also be purely degenerative without any recollection of trauma (Citation2). In the clinical setting the judgement of traumatic aetiology is based entirely on patient history, and the word “traumatic” is used to refer to patients' own perception of the onset of symptoms (www.websters-online-dictionary.org). If the patient does not recall any traumatic event relating to the onset of symptoms the condition is defined as non-traumatic.
The treatment of symptomatic rotator cuff rupture, despite aetiology, is usually operative since the tendon is unable to attach to bone spontaneously and furthermore the rupture may induce permanent atrophic muscle changes and enlarge by time (Citation3). Therefore, operative reinsertion of the torn tendon and combined acromioplasty are often advocated. However, the healing potential of large and degenerative rotator cuff ruptures may be compromised (Citation4). It is therefore unclear whether operative treatment of degenerative, non-traumatic rotator cuff ruptures is beneficial (Citation5). Braune et al. reported significantly better results in the treatment of traumatic rotator cuff ruptures compared with non-traumatic ruptures (Citation1).
Ageing is strongly related to tendon degeneration and non-traumatic rotator cuff ruptures (Citation2,6). Tempelhof et al. reported a 13%-prevalence in asymptomatic patients aged 50–59 years, whereas the prevalence was 51% in patients over 80 years (Citation7). Accordingly, Braune et al. reported that traumatic rotator cuff rupture patients are younger than non-traumatic patients (Citation1).
The aim of this registry study was to explore the differences in outcome, peroperative findings, and demographics after operative treatment of traumatic versus non-traumatic rotator cuff ruptures. Based on previous reports, the hypothesis was that operative treatment of traumatic rotator cuff rupture patients leads to better results than operative treatment of non-traumatic patients, and that traumatic patients are younger in age.
Materials and methods
A registry (ArtuX, BCB Medical, Turku, Finland) for all patients undergoing shoulder surgery was established in 2007 at Turku University Hospital. The institution serves as a tertiary hospital in a district of 463,000 inhabitants, and shoulder patients are sent to the institution from the local health care providers. Preoperative, peroperative, and postoperative information of 1143 patients had been gathered into the registry by the end of year 2010. The indication for operative treatment of rotator cuff tear at our institution was a clinical suspicion of a rotator cuff tear of patients with typical symptoms of pain and clinically detected functional weakness. Contraindications included cuff tear arthropathy, severe osteoarthritis with clearly visible osteophytes, drug abuse, severe internal disease disallowing general anaesthesia, and patient's denial. X-ray investigation was performed in all patients but MRI in only clinically challenging situations. A total of 306 consecutively operated patients with arthroscopically, peroperatively documented infraspinatus and/or supraspinatus and/or subscapularis tears (years 2007–2009) with at least 1 year follow-up were included in this registry study. The patients were carefully interviewed for the symptoms and examined by an independent physiotherapist. The classification of aetiology of rotator cuff rupture (traumatic versus non-traumatic) was based entirely on the patient history and mechanism of injury. In case of a clear trauma at the onset of symptoms, the rupture was regarded as traumatic and the mechanism was recorded. If the patient could not recall any traumatic event relating to the onset of symptoms, the rotator cuff rupture was regarded as non-traumatic. The range of motion and strength of the affected shoulder were measured, and Constant and Murley score was calculated (Citation8).
All operations were performed arthroscopically by one of three experienced shoulder surgeons. The rotator cuff tendon involvement and the size of the rupture, together with other pathologic findings of the shoulder joint and subacromial space, were structurally recorded. Cuff ruptures were reinserted anatomically, if possible with non-absorbable titanium anchors (Corkscrew®, Arthrex, Naples, Florida, USA). Additional acromioplasty was performed in all operations. Biceps tendon tenotomy or tenodesis was performed if the biceps tendon loading was painful preoperatively or if the tendon was noted to be ruptured or unstable during the operation. Patients were discharged from hospital on the first postoperative day. A supporting sling was used for 2 weeks postoperatively. At 2 weeks postoperatively patients were called in for a physiotherapist's guidance for passive movement exercises, and at 6 weeks active overhead motion exercises were begun. Strength exercises were begun at 10 weeks after the operation. The range of motion and strength of the affected shoulder were measured, and Constant score was calculated again at 3 months and 1 year postoperatively. Absolute Constant score, size of the rupture, and age of the patient were used as the outcome measures. The follow-up time was 1 year.
Statistical methods
The differences in categorical variables between groups were tested with chi-square test or Fisher's exact test. Two-sample t test was used to test group differences in continuous variables. The difference in postoperative Constant score between the traumatic and the non-traumatic group was also analysed by adjusting for confounding factors using a linear model. P values less than 0.05 were considered statistically significant. Results are given as means ± S.D. The statistical analyses were made using SAS System for Windows, release 9.2 (SAS Institute, Inc., Cary, NC, USA).
Results
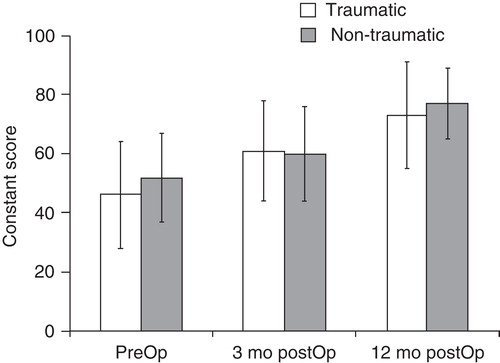
Altogether 112 traumatic and 167 non-traumatic rotator cuff rupture shoulders were available for 1-year follow-up. One patient died of other causes, one patient moved to another district, and 25 patients could not be reached for 1-year follow-up, making the drop-out rate 8.8% (9.7% versus 8.2%). In the traumatic group preoperative mean Constant score was lower than in the non-traumatic group (46 versus 52, P = 0.01) (). The postoperative Constant scores behaved similarly in both traumatic and non-traumatic patient groups. Absolute increase of Constant scores was 27 and 25 points at 1 year after the operation, respectively (P = 0.64). At 3 months Constant scores were 61 and 60 (P = 0.72) and at 1 year 73 and 77 (P = 0.03) (). After adjustment for preoperative Constant score, gender, and size of rupture, the difference at 1 year Constant score between the traumatic and the non-traumatic group was not significant (adjusted means 74 and 75, P = 0.46). Although Constant scores were lower in women than in men, there was no significant difference in Constant score changes between genders at 1 year follow-up (P = 0.86). Altogether 80% versus 83% of patients were free from pain (VAS 0, P = 0.50); 91% of the patients in the traumatic and 93% in the non-traumatic group were satisfied with treatment result at 1-year follow-up and felt their shoulder to be significantly better than preoperatively (P = 0.45).
Figure 1. Preoperatively the mean Constant score (with SD whiskers) of the traumatic group was slightly lower than in non-traumatic group (46 vs. 52, P = 0.01). The postoperative Constant scores behaved similarly in traumatic and non-traumatic patient groups. At three months Constant scores were 61 and 60 (P = 0.72) and at one year 73 and 77 (P = 0.03) respectively.
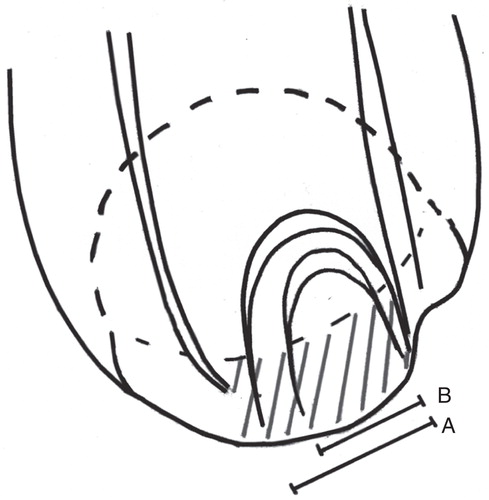
Peroperatively the rotator cuff rupture was detected in all patients. The rupture occurred in the supraspinatus tendon in 94% of traumatic versus 95% of non-traumatic patients. In the traumatic group the penetrating ruptures were larger in size (24.2 mm versus 17.5 mm, P = 0.0002) and involved more often the whole insertion of the supraspinatus tendon (41% versus 17%, P < 0.0001, ). Subscapularis tendon rupture was more prevalent in conjunction with traumatic supraspinatus ruptures (20% versus 11%, P = 0.049). Irreparable rotator cuff rupture was detected in 2.8% versus 5.2% of the cases. The traumatic and non-traumatic groups differed in the amount of biceps pathologies and procedures (P = 0.02). The biceps tendon was noted to be irritated and/or frayed in 44% versus 32% of the shoulders. The intra-articular biceps tendon was missing in 8% of both the traumatic and non-traumatic shoulders. Biceps tenodesis was performed in 16% versus 12% and tenotomy in 24% versus 13% of the patients in the traumatic and the non-traumatic groups, respectively.
Figure 2. Peroperatively the rotator cuff rupture was seen in supraspinatus tendon in 94% versus 95% of patients. There was a significant difference in the size of the tendon rupture between the groups (P < 0.0001). The mean size (AP dimension) of penetrating tears was 24.2 mm (A) in the traumatic group and 17.5 mm (B) in the non-traumatic group. In the traumatic group the rupture involved more often the whole insertion area of supraspinatus tendon (41% versus 17%) (shaded area).
The mean age of patients was 58 years in the traumatic group and 57 in the non-traumatic group (range 26–80 (SD 11 years) and range 29–79 (SD 10 years), respectively, P = 0.63). In the traumatic group there were fewer women than in the non-traumatic group, 36% versus 47% (P = 0.06). A total of 54% of patients in the traumatic and 81% of patients in the non-traumatic group suffered from shoulder pain and disability for more than 1 year before operative treatment. The delay between the onset of symptoms and the operation was 12.4 months in the traumatic and 18.8 months in the non-traumatic shoulders (P < 0.0001). The delay did not statistically significantly affect the final Constant score in either group (P = 0.14 and P = 0.85) ().
Table I. Patient demographics and preoperative characteristics.
Discussion
In our study both the traumatic and non-traumatic group improved similarly in terms of Constant score after operative treatment of rotator cuff rupture. Preoperative Constant scores were lower in the traumatic group. This difference may be due to larger rupture size in the traumatic group, as the groups were similar in age. This small difference persisted throughout the follow-up. It is unclear whether this small difference in Constant scores has any clinical importance.
In our study cohort the traumatic ruptures were significantly larger in size and involved more often the subscapularis and biceps tendon. It is generally accepted that a rotator cuff rupture is most often a combination of both traumatic and degenerative changes, so-called acute on chronic situation. The results of our study reflect this degenerative nature of rotator cuff ruptures. Based on similar demographics it may be that in our study also the traumatic ruptures are in fact degenerative, but the sudden traumatic event enlarged the rupture. In basic research it has been shown that the mechanically weakest point of bone–tendon–muscle continuity is the musculotendinous junction (MTJ) and not the tendon–bone interface (Citation9,10). Therefore, the tendon must be degenerated and compromised in all cases, in order to become torn from the bone before the MTJ fails.
In literature there are only few earlier studies comparing traumatic and non-traumatic rotator cuff ruptures. Braune et al. reported in a retrospective set-up significantly better results with traumatic rotator cuff ruptures compared with non-traumatic ruptures (Constant score 94 versus 75) (Citation1). In their material, patients assigned to the traumatic group were significantly younger than those with a non-traumatic rupture (34 versus 54 years). In our registry study, both groups were similar also with respect to the age of the patients.
The lack of preoperative and postoperative MRI investigation and a relatively long time between the onset of symptoms and operative treatment are clear limitations of our study. Only systematic radiographs were obtained preoperatively. MRI investigation can detect secondary traumatic changes such as haemorrhage and oedema, which could further be compared with patient history. However, as the patients had to wait for a considerable time before the clinical and imaging investigations, it is likely that the possible acute traumatic changes seen in MRI would have diminished or disappeared. The follow-up time in our study was only 1 year; however, it was the same for all patients, and it has been previously reported that after arthroscopic rotator cuff repair the Constant score significantly improves until 1 year, after which it is stabilized (Citation11). It has been previously reported that there is a high risk of re-rupture in operative treatment of rotator cuff ruptures (Citation12-15). Furthermore this risk increases in the presence of tendon degeneration. Due to lack of MRI investigation we have not studied the postoperative tendon integrity, nor the difference of integrity between the groups. However, it seems that in our cohort operative treatment of also degenerated rotator cuff ruptures yields good results despite probable re-ruptures. It should also be pointed out that recently there was a report in this journal on factors related to the successful outcome of conservative treatment for rotator cuff tears (Citation16).
In clinical practice we are generally dependent on the information given by the patient. In our study the definition of traumatic is used to refer to the patients' own perception of the onset of symptoms. The patient's memory may be questionable, and the assignment of patients to either traumatic or non-traumatic may be influenced by the patients' motives or memory. However, this assignment represents clinical practice, in which the results of this study are applicale. It is important to acknowledge that the aetiologic definition of rotator cuff rupture is different from the definition by duration of symptoms, acute versus chronic. In our study the mean delay between the onset of symptoms and treatment was quite long in both groups. The delay of surgical treatment was due to a long referral process and relatively long queues at our institution. The delay may have influenced the selection of the patients, and we have no data of patients who possibly were treated elsewhere. However, in our study the waiting time did not statistically significantly affect the treatment outcome, nor the age of the patients.
Our registry study of 306 consecutively operated and prospectively evaluated shoulders demonstrates essentially similar outcome and essentially good results after operative treatment of traumatic and non-traumatic rotator cuff rupture patients. Peroperatively the traumatic rotator cuff ruptures were larger in size. In our cohort, patients' recollection of predisposing trauma reflects the size of the rotator cuff rupture but does not reflect the patients' age, nor the outcome of rotator cuff reconstruction. At 1 year postoperatively a Constant score level of 75, in both traumatic and non-traumatic rotator cuff ruptures, can be predicted. Further analyses are needed to study factors influencing the outcome in traumatic and non-traumatic patient groups.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Braune C, von Eisenhart-Rothe R, Welsch F, Teufel M, Jaeger A. Mid-term results and quantitative comparison of postoperative shoulder function in traumatic and non-traumatic rotator cuff tears. Arch Orthop Trauma Surg. 2003;123:419–24.
- Yamaguchi K, Ditsios K, Middleton WD, Hildebolt CF, Galatz LM, Teefey SA. The demographic and morphological features of rotator cuff disease. A comparison of asymptomatic and symptomatic shoulders. J Bone Joint Surg Am. 2006;88:1699–704.
- Mall NA, Kim HM, Keener JD, Steger-May K, Teefey SA, Middleton WD, Symptomatic progression of asymptomatic rotator cuff tears: a prospective study of clinical and sonographic variables. J Bone Joint Surg Am. 2010;92:2623–33.
- Matthews TJ, Hand GC, Rees JL, Athanasou NA, Carr AJ. Pathology of the torn rotator cuff tendon. Reduction in potential for repair as tear size increases. J Bone Joint Surg Br. 2006;88:489–95.
- Ejnisman B, Andreoli CV, Soares B, Peccin MS, Abdalla RJ, Faloppa F, WITHDRAWN: Interventions for tears of the rotator cuff in adults. Cochrane Database. Syst Rev. 2009;CD002758.
- Fehringer EV, Sun J, VanOeveren LS, Keller BK, Matsen FA 3rd. Full-thickness rotator cuff tear prevalence and correlation with function and co-morbidities in patients sixty-five years and older. J Shoulder Elbow Surg. 2008;17:881–5.
- Tempelhof S, Rupp S, Seil R. Age-related prevalence of rotator cuff tears in asymptomatic shoulders. J Shoulder Elbow Surg. 1999;8:296–9.
- Constant CR, Murley AHG. A clinical method for the functional assessment of the shoulder. Clin Orthop Relat Res. 1987;214:160–4.
- Noonan TJ, Best TM, Seaber AV, Garrett WE Jr. Identification of a threshold for skeletal muscle injury. Am J Sports Med. 1994;22:257–61.
- Tidball JG, Salem G, Zernicke R. Site and mechanical conditions for failure of skeletal muscle in experimental strain injuries. J Appl Physiol. 1993;74:1280–6.
- Charousset C, Grimberg J, Duranthon LD, Bellaiche L, Petrover D, Kalra K. The time for functional recovery after arthroscopic rotator cuff repair: correlation with tendon healing controlled by computed tomography arthrography. Arthroscopy. 2008;24:25–33.
- Gazielly DF, Gleyze P, Montagnon C. Functional and anatomical results after rotator cuff repair. Clin Orthop Relat Res. 1994;43–53.
- Harryman DT 2nd, Mack LA, Wang KY, Jackins SE, Richardson ML, Matsen FA 3rd. Repairs of the rotator cuff. Correlation of functional results with integrity of the cuff. J Bone Joint Surg Am. 1991;73:982–9.
- Jost B, Pfirrmann CW, Gerber C, Switzerland Z. Clinical outcome after structural failure of rotator cuff repairs. J Bone Joint Surg Am. 2000;82:304–14.
- Knudsen HB, Gelineck J, Sojbjerg JO, Olsen BS, Johannsen HV, Sneppen O. Functional and magnetic resonance imaging evaluation after single-tendon rotator cuff reconstruction. J Shoulder Elbow Surg. 1999;8:242–6.
- Tanaka M, Itoi E, Sato K, Hamada J, Hitachi S, Tojo Y, Factors related to successful outcome of conservative treatment for rotator cuff tears. Ups J Med Sci. 2010;115:193–200.
