Abstract
Dignity is a key value within healthcare. Technology is also recognized as being a fundamental part of healthcare delivery, but also a potential cause of dehumanization of the patient. Therefore, understanding how medical devices can be designed to help deliver dignity is important. This paper explores the role of empathy tools as a way of engendering empathy in engineers and designers to enable them to design for dignity. A framework is proposed that makes the link between empathy tools and outcomes of feelings of dignity. It represents a broad systems view that provides a structure for reviewing the evidence for the efficacy of empathy tools and also how dignity can be systematically understood for particular medical devices.
1. Introduction
The paramount importance of patient dignity has been recognized in healthcare [Citation1]. However, there is a lack of research for how medical device designers can facilitate patient dignity. Generating empathy within designers aids them in creating products to meet the needs of their users [Citation2] and could also assist in the design of medical devices to help patients maintain their dignity. Empathy tools are recognized as helpful; however, there is a lack of research linking the effects on patient dignity from the use of empathy tools in medical device design. This paper presents a conceptual framework with reference to evidence to address this gap in the literature.
1.1. Background and definitions
Dignity has long been recognized as a fundamental human right [Citation3]. It is particularly important in healthcare, for example in the UK, this is embodied in the National Health Service (NHS) Constitution, which states that dignity ‘should be at the core of how patients and staff are treated’ [Citation4] (p. 3). In this case it is derived from the rights conferred by the European Convention on Human Rights [Citation5]. It is recognized that illness and hospitalization can severely compromise a person’s dignity [Citation6]. Technology and medical devices play a fundamental role in the delivery of modern healthcare and as such can have a big impact on a patient’s dignity. Some argue that technology can have a serious dehumanizing effect generally, but specifically in the healthcare context [Citation7–9].
Many attempts have been made to try and define the concept of dignity in various settings, particularly in healthcare, in order to discuss it in an academic context. The Oxford English Dictionary defines dignity as ‘the quality of being worthy or honourable; worthiness, worth, nobleness, excellence’ [Citation10], but, within healthcare it has been debated as to whether dignity is even a useful concept to acknowledge, due to the difficulty of defining its meaning [Citation11,Citation12]. However, Matiti and Trorey [Citation13] conclude that the best way to define it is through the themes that maintain dignity. They suggest that in healthcare the following factors contribute to dignity: privacy; confidentiality; communication and the need for information; choice, control and the involvement in care; respect; and decency and forms of address. Cass et al. [Citation14] propose this definition: ‘Dignity in care means the kind of care, in any setting, which supports and promotes, and does not undermine, a person’s self-respect’ (p. 6). They offer dignity factors of: choice and control; communication; eating and nutritional care; pain management; personal hygiene; practical assistance; and privacy and social inclusion.
Martin et al. [Citation15] explain that, to allow patients to maintain their dignity, all medical devices must meet the requirements of its users and to do this it needs to be designed with the user in mind.
The Oxford English Dictionary defines empathy as ‘the ability to understand and appreciate another person’s feelings, experience, etc.’ [Citation10]. Kouprie and Visser [Citation2] discuss the affective and the cognitive aspects of empathy, put forward by Baron-Cohen and Wheelwright [Citation16], but within the context of design, p, 164. They explain that the affective aspect is ‘the automatic response to another’s emotional state’. The cognitive aspect is a person’s understanding of another’s feelings and this can be conveyed through the empathizer hearing about the situation that the empathizee is in: ‘It is concerned with intellectually taking the role or perspective of another person’. To put this in a design context, Mattelmäki and Battarbee [Citation17] state ‘design empathy means that people are seen and understood from where they stand, not as test subjects but as persons with feelings’ (p. 266).
The literature recognizes that it is important that designers have empathy with their users [Citation18]. Empathic design is described as the process by which ‘designers attempt to get closer to the lives and experiences of (putative, potential or future) users, in order to increase the likelihood that the product or service designed meets the user’s needs’ [Citation2] (p. 437).
McGinley and Dong [Citation19] state there is a need to go beyond written data ‘into the realm of human understanding and empathy is crucial for effective design outcomes, as considering individuals as merely numbers and measurements is limited, no matter how thoroughly it is carried out’. There are several pieces of research into the ways in which we can encourage empathy in various areas of design [Citation20], as well as specific methods such as empathy probes [Citation17], empathic lead users [Citation21], capability loss simulation [Citation22], critical user forums [Citation23] and a suggested framework on how the designer can step into the users life in order to generate empathy with that user [Citation2]. However, these authors don’t specifically discuss these methods in the context of the design of medical devices.
There is extensive literature that covers usability and consideration of the user, in medical device design. For example Martin et al. [Citation15] discuss the ways that ergonomics can assist the designer in considering the user in the design and development of medical devices. Other authors comment on specific techniques for considering the user when designing medical devices, such as Vincent and Blandford [Citation24], who discuss the use of personas in medical device design. However, this literature does not comment specifically on encouraging empathy within medical device design.
The focus of this paper is on designers; however, the role of empathy in healthcare professionals has long been considered and Stepien and Baernstein [Citation25] provide a useful review of this in their paper on ‘Educating for Empathy’. This paper acknowledges the problems of definition and measurement, but does provide evidence for the opportunity to influence empathy positively.
This work refers specifically to the existing evidence of the effect that empathy tools have on a product developer’s empathy for their users, how this impacts on medical device design and, consequently, the dignity of the user. This is done through a review of the literature, case studies and a study of medical device designers in industry. The evidence is discussed in reference to a framework presented later in the paper.
1.2. Description of empathy tools and their use
There are a number of techniques for encouraging empathy in designers. Kouprie and Visser [Citation2] divide these into three areas: research; communication; and ideation. Although this division helps us to recognize the differences between different empathy tools and techniques, they are not orthogonal. For this reason the techniques will be discussed in terms of those that are based on direct contact with potential users and those that describe or simulate users. These are discussed in more detail below.
1.2.1. Direct contact
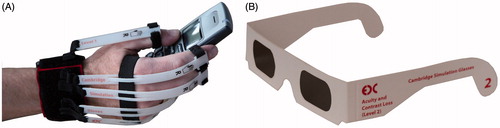
Kouprie and Visser [Citation2] highlight that direct contact with users should be included where possible (p. 439). They suggest that ‘most authors recommend having designers conduct observation studies, e.g. to follow the user in his context’. Furthermore, Dong et al. [Citation26] explain that direct contact is the best way of generating empathy and understanding in designers. There are several ways that real people can be used directly to encourage empathy in designers. These include observations, user trials and focus groups, amongst other things. presents some example methods.
Table 1. Example methods of generating empathy, based on direct contact.
1.2.2. Indirect contact
Kouprie and Visser [Citation2] explain that communication techniques should be used if the designer cannot have direct contact with potential users. They add that, to increase the designer’s empathic understanding of the user, they should (where possible) use raw data directly from the user, such as photos of them in their homes, or original handwriting. These methods of indirect contact have been divided into 'representing' and ‘simulating’ users. Examples of these are outlined in and respectively.
Table 2. Example methods of generating empathy, by representing users.
Table 3. Example methods of generating empathy, by simulating users.
2. Method
So far we have presented the importance of dignity in healthcare, the central and potentially dehumanizing role that medical devices play, linked to the potential use of empathy tools for developing an understanding of user needs in developers. What is lacking is a conceptualization of how empathy tools potentially link to feelings of dignity in the patient and what evidence there is for the efficacy of such tools. In this section a conceptual framework in three levels of increasing detail is proposed based on 10 years of experience of developing, testing, manufacturing and using empathy tools in an engineering design research centre in a UK university [Citation32,Citation33]. Part of the work was focused on the fidelity of the simulation, the usability of the simulators by the person using them and their use in usability assessment of devices as a substitute for testing with real users. The tools were also used for inclusive design training of a range of people from large multi-national companies. In addition, vision and dexterity simulators were integrated into a set of schools resources to bring inclusive design into the classroom [Citation34]. Recent work has included systematic interviews of designers to understand their attitudes to simulators [Citation35].
2.1. Framework
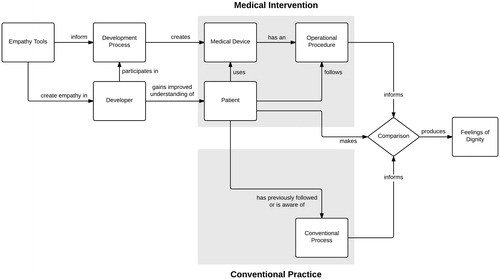
Designing technology that enables dignity is a complex and multifaceted problem. The work of Kouprie and Visser [Citation2] provides a specific framework that addresses the stages that a designer goes through in developing empathy with the end user. It is derived from a psychological understanding of empathy. However, this paper considers a broader view that is looking at a potential causal link between empathy tools and patient dignity in the context of medical device use. This is shown in , where Empathy Tools are used to inform the Development Process that creates a new Medical Device. This has an Operational Procedure that is followed by the patient, who consequently experiences Feelings of Dignity.
expands this core process to include the Developer and Patient and how the Empathy Tools help improve the developer’s understanding of the patient. The singular form is used to describe the stakeholders, but applies equally to a range of patients or developers. Developers cover a range of stakeholders involved in the development process that includes but is not limited to engineers, industrial designers and ergonomists. This figure also introduces the notion of how Feelings of Dignity are derived by the Patient making a Comparison of the experience of the Medical Device with experience of the Conventional Process. A simple example is where a patient has had a colostomy and as a result the patient has to use a colostomy bag. Here the comparison would be with using a conventional toilet (Conventional Process). The user would consider the differences between the two. In practice there may be a distinction between the Patient and a healthcare professional or carer using the device with or on them. This would, however, add further complexity, with limited benefit in adding to the principles involved.
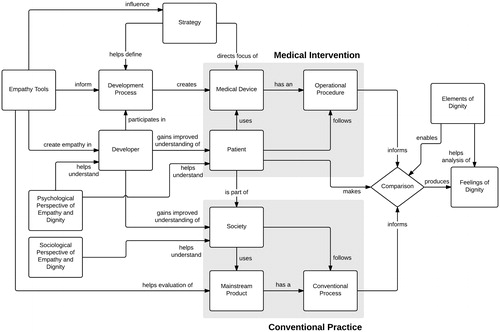
introduces a range of additional elements. First, it elaborates the Conventional Practice further by bringing a societal dimension (Society) that covers the development of cultural norms that the patient is likely to compare with. It also includes Mainstream Product that may perform part of, or be replaced by, the operation of the Medical Device. The conventional toilet in the colostomy bag example would be such a mainstream product.
Second, the full conceptual framework introduces Elements of Dignity, which are modified definitions drawn from Matiti and Trorey [Citation13].
Privacy, which includes the visual, auditory and olfactory presentation of the device in use.
Control, which relates to the level of independence that can be maintained by the patient.
Choice, which concerns whether the patient can continue to do the things that they have done previously or would like to do in the future.
Communication, which relates here specifically to the control the patient has over the disclosure of their condition and the use of a medical device. For example, a blind person with white stick may want to make others aware (disclose) their lack of vision.
Respect, which is specific to the feelings of being respected by the patient.
These definitions are by no means exhaustive and overlap; however, they represent a way of examining the development of Feelings of Dignity. In reality this comparison will be different for different people and may be a very visceral reaction. Nonetheless, the Developer can consider these elements of dignity for each step of the Operational Procedure compared to a benchmark of the Conventional Process. Again in the case of the colostomy bag, the comparison may be: does the user experience differences in visibility such as a bulge under their clothing? Do they experience unusual sounds or a smell from the bag? How does it impact on the control they have and the choices they can make about activities?
Third, the framework introduces Strategy, which can be influenced by the Empathy Tools. The tools can have an impact on senior decision-makers by raising the awareness of the struggle that patients may face with existing solutions. This in turn can lead to changes in the Development Process to make it more patient-focused as well as providing greater focus on dignity for specific Medical Device development.
Finally, it is possible to view this process in terms of Psychological and Sociological theories that have the potential to provide insights into underlying mechanisms and in turn stimulate improvements to the Empathy Tools. Of particular note is E-S theory and the associated Empathizing and Systemizing Quotients (EQ & SQ) devised by Baron-Cohen and Wheelwright [Citation16]. These quotients have been used to show variation between different cohorts such as males and females and technical and non-technical cohorts. This enables a quantitative measure of a developer’s empathy levels and also opens up the possibility of determining if the empathy tools impact a developer’s EQ level.
It is also worth noting that the Empathy Tools can be used in a variety of contexts that include training the Developers and the evaluation of solutions in the Development Process. In addition, Empathy Tools have been used to raise awareness and understanding amongst carers, relatives, local authorities and schools and in conjunction with the World Health Organization, the RNIB and Guide Dogs for the Blind [Citation36] and, thus, impact wider ‘Society’. Note, this relationship is not shown to avoid additional complexity to the diagram. The users’ feelings regarding dignity are likely to be influenced by the wider societal context that they sit in, for example how people view incontinence. Empathy Tools can be used with and by Developers to develop insight and empathy about patients. This should not only drive motivation, but also provide insight into the user requirements for the design of the Medical Device.
The framework highlights two practical things in enabling dignified outcomes for patients. The first is the role of Empathy Tools in influencing the process at multiple levels across different stakeholders. The second is the notion of comparison between a benchmark of the Conventional Process and the new Operational Procedure of the Medical Device. The developer can systematically compare the two step-by-step for the user journey [Citation28,Citation36].
This analysis is performed by breaking the use of the Medical Device into steps. This is essentially the Operational Procedure, but is broader than a narrow standard operating procedure as it includes all necessary steps to successfully gauge the benefit of the intervention. For example, in the case of an auto-injector (a patient activated spring loaded syringe delivering a single drug dose) it should include issues such as carrying, storage and the task of opening and using the sterilizing alcohol wipe for cleaning the injection site. In the exclusion audit [Citation28] each step is analysed in terms of the sensory, cognitive and motor demands. Each step represents a metaphorical hurdle that users have to get over. The greater the demand on the user’s sensory, cognitive and motor skills the harder the task is to complete. Where the demand is greater than the user’s capability, they are excluded. The aim in the design process is to lower these hurdles to reduce exclusion and make the device easier to use. We are proposing to extend the exclusion analysis criteria to include Elements of Dignity. For each step it is possible to perform a better–same–worse comparison with the Conventional Process. Although there is unlikely to be an exact mapping of task steps between the two processes, a judgement can be made. For example, if a task step is not required at all in the Conventional Process, then it is reasonable to say with the new medical device that the task is more difficult and may impact one or more Elements of Dignity. It is important when making the better–same–worse comparison to record both the result of the comparison, but also the underlying reason for the judgement, because the reason will inform potential improvements to the design. The grid can be formed with physical cards and/or recorded in a spreadsheet [Citation28]. With the auto-injector example it would highlight both the usability and the privacy problems associated with removing clothing to gain access to a suitable injection site (for example the thigh area).
Although the approach is methodical it is less about creating a measure and more about providing insights to the Developer to help them better understand the impact on the patients and enable them to make more informed decisions.
3. Discussion
When it comes to the use of empathy tools to drive dignity in relation to medical device use, there is no international, multi-centre randomized control trial that says it works. The framework proposed in this paper shows that such an approach would be unlikely to be successful for such a complex system problem. What is suggested is to use a range of methods to probe what happens when empathy tools are used.
This paper presents a range of qualitative evidence that empathy tools do have a significant impact on stakeholders in the development process. What is less clear is how this impacts the dignity afforded by actual products. In other words we have to be cautious about making the jump from an enthusiastic response from stakeholders about empathy tools to say that the design has changed for the better as a result. However, the examples from two global companies in Hosking et al. [Citation35] strongly indicated that the empathy had an impact on developers, the subsequent design of products and their usability.
What is harder to say is if these improvements also led to a maintenance or improvement in dignity, simply because it was not systematically probed. The framework does provide a way of systematically doing this and could be applied to future projects.
The framework encapsulates psychological and sociological theory regarding empathy and dignity such as E-S Theory [Citation16]. The variability in empathy between different types of people means that some will be inherently more empathic than others, for example staff engaged in technical aspects of design or engineering may be less empathic. This has an impact in terms of the make-up of the project team and also how the impact of the empathy tools may vary depending on a person’s underlying EQ. Further research is need to understand this and the availability of the Quotients makes this viable, i.e. the correlation between and EQ and response to the tools could be assessed.
Another aspect of the framework that is worth elaborating on is the notion of Elements of Dignity these help analyse the Feelings of Dignity that the Patient experiences. These can be methodically considered for each task step in the use of the medical device. The framework does not include specific properties of the device such as aesthetics that could potentially be mapped to the Elements of Dignity. For example, the device may have an aesthetic appearance that makes it discreet and, therefore, helps maintain privacy. The problem with this is that devising a comprehensive and indeed comprehensible set of properties is problematic due to the complexity of product form and function. Something such as Gero’s [Citation37] Function–Behaviour–Structure Framework could be considered, but should only be included if it adds useful insights.
4. Conclusions
Dignity is a fundamental principle in healthcare and technology has a fundamental role in the delivery of healthcare. However, technology can be dehumanizing and have a detrimental impact on dignity. Interventions to mitigate this occurring are, therefore, important. This paper shows that empathy tools can and are used to influence a range of stakeholders involved in the delivery of medical devices. In addition it is possible to systematically analyse the link from such tools to the patient maintaining dignity. There is emerging evidence that this works albeit predominantly from other fields. Finally, developers can methodically look at dignity in relation to their designs through an extension to tools such as the exclusion audit.
4.1. Future work
There is a need to increase the evidence base for the efficacy of empathy tools in improving outcomes. To do this, systematic end-to-end studies are required. This would not only increase confidence in the approach, but would help encourage uptake and importantly also help refine the approach used. Within such a study the use of the EQ/SQ instrument would be valuable in understanding the underlying empathy of participants and how this could be influenced. Finally, developing the exclusion audit approach to include dignity parameters would provide a practical tool for developers to understand the impact of their designs.
Acknowledgements
We would also like to extend our thanks to Dr Warren Kerley, Dr Nigel Ball, Dr Thomas Stone, Dr Nicola Heron, Dr Avril McCarthy and Sonya Sireau for their valuable advice.
Declaration of interest
This paper was authored through funding from the EPSRC-NIHR HTC Partnership Award: Promoting Real Independence through Design Expertise (ref: EP/M000273/1) and NIHR Collaboration for Leadership in Applied Health Research and Care East of England (CLAHRC EoE) at the Cambridge and Peterborough NHS Foundation Trust. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health.
References
- Jacobson, N., 2007, Dignity and health: A review. Social Science & Medicine, 64, 292–302
- Kouprie, M., and Visser, F.S., 2009, A framework for empathy in design: Stepping into and out of the user's life. Journal of Engineering Design, 20, 437–448
- UN General Assembly, 1948, Universal Declaration of Human Rights (UDHR), G.A. Res. 217A(III), U.N. GAOR, 3d Sess., U.N. Doc. A/810. Available online at: http://www.un.org/Overview/rights.html [last accessed 19 Nov 2014]
- London: Department of Health, 2013, The NHS Constitution
- London: Department of Health, 2013, The Handbook to the NHS Constitution (for England)
- Baillie, L., 2009, Patient dignity in an acute hospital setting: A case study. International Journal of Nursing Studies, 46, 23–37
- Bevan, M.T., 1998, Nursing in the dialysis unit: Technological enframing and a declining art, or an imperative for caring. Journal of Advanced Nursing, 27, 730–736
- Haslam, N., 2006, Dehumanization: An Integrative Review. Personality and Social Psychology Review, 10, 252–264
- Haslam, N., 2007, Humanising medical practice: The role of empathy. Medical Journal of Australia, 187, 381–382
- Oxford University Press, 2015, OED Online. Available online at: http://www.oed.com. [last accessed 26 Jan 2015]
- Mains, E.D., 1994, Concept clarification in professional practice: Dignity. Journal of Advanced Nursing, 19, 947–953
- Killmister, S., 2010, Dignity: Not such a useless concept. Journal of Medical Ethics, 36, 160–164
- Matiti, M.R., and Trorey, G.M., 2008, Patients’ expectations of the maintenance of their dignity. Journal of Clinical Nursing, 17.20, 2709–2717
- Cass, E., Robbins, D., and Richardson, A., 2006, Dignity in Care (London: Social Care Institute for Excellence)
- Martin, J.L., Norris, B.J., Murphy, E., and Crowe, J.A., 2008, Medical device development: The challenge for ergonomics. Applied Ergonomics, 39, 271–283
- Baron-Cohen, S., and Wheelwright, S., 2004, The Empathy Quotient: An Investigation of adults with Asperger Syndrome or High Functioning Autism, and normal sex differences. Journal of Autism and Developmental Disorders, 34, 163–175
- Mattelmäki, T., and Battarbee, K., 2002, Empathy probes (PDC). pp. 266–271
- Strickfaden, M., and Devlieger, P., 2011, Empathy through accumulating techne: Designing an accessible metro. The Design Journal, 14, 207–229
- McGinley, C., and Dong, H., 2011, Designing with information and empathy: Delivering human information to designers. The Design Journal, 14, 187–206
- Crossley, L., 2003, Building emotions in design. The Design Journal, 6, 35–45
- Lin, J. and Seepersad, C.C., 2007. Empathic Lead Users: The Effects of Extraordinary User Experiences on Customer Needs Analysis and Product Redesign. ASME 2007 International Design Engineering Technical Conferences and Computers and Information in Engineering Conference, pp. 289–296
- Goodman-Deane, J., Waller, S., and Clarkson, P.J., 2008, Simulating Impairment. Demonstration Presented at (re)Actor3/HCI
- Dong, H., Clarkson, P.J., Cassim, J., and Keates, S., 2005, Critical User Forums: An effective user research method for inclusive design. The Design Journal, 8, 49–59
- Vincent, C.J., and Blandford, A., 2014, The challenges of delivering validated personas for medical equipment design. Applied Ergonomics, 45, 1097–1105
- Stepien, K.A., and Baernstein, A., 2006, Educating for empathy. Journal of General Internal Medicine, 21, 524–530
- Dong, H., Nickpour, F., and McGinley, C., 2009, Designing Ergonomic Data Tools for Designers. DS 58-8: Proceedings of ICED 09, the 17th International Conference on Engineering Design, Design Information and Knowledge (California: Stanford University), 53–64
- Morgan, D.L., 1996, Focus groups. Annual Review of Sociology, 4, 129–152
- Waller, S., Bradley, M., Hosking, I., and Clarkson, P.J., (2015), Making the case for inclusive design. Applied Ergonomics, 46, 297–303
- Zitkus, E., Langdon, P., and Clarkson, P.J., (2012), How to support designers effectively with Knowledge about accessibility and inclusion. ICDHS 2012 - Design Frontiers: territories, concepts, technologies - 8th Conference of the International Committee for Design History and Design Studies, 1, 257–264
- Maguire, M., 2001, Methods to support human-centred design, International journal of human-computer studies, 55, 587–634
- Buchenau, M., and Suri, J.F., 2000, Experience prototyping. Proceedings of the 3rd Conference on Designing interactive systems: processes, practices, methods, and techniques Brooklyn, New York, 17th to 19th August 2000, 424–433
- Hosking, I., Waller, S., and Clarkson, P.J., 2010, It is normal to be different: Applying inclusive design in industry. Interacting with Computers, 22, 496–501
- Cardoso, C., and Clarkson, P.J., 2012, Simulation in user-centred design: Helping designers to empathise with atypical users. Journal of Engineering Design, 23, 1–22
- Nicholl, B., Hosking, I., Elton, E., Lee, Y., Bell, J., and Clarkson, P.J., 2012, Inclusive design in the Key Stage 3 classroom: An investigation of teachers’ understanding and implementation of user-centred design principles in design and technology. International Journal of Technology and Design Education, 4, 921–938
- Hosking, I., Cornish, K., Bradley, M., and Clarkson, P.J., 2015, Empathic Engineering: A framework for understanding the impact of empathy tools in design. Cambridge Engineering Department Report 2015 CUED/C-EDC/TR.164
- Clarke, Z., Judge, S., Heron, N., Langley, J., Hosking, I., and Hawley, M., 2011, User involvement in the early development of assistive technology devices. Everyday Technology for Independence and Care, Assistive Technology Research Series, 29, 362–373
- Gero, J.S., 1990, Design prototypes: A knowledge representation schema for design. AI Magazine, 11, 26