Abstract
Background: The 2013 ACC/AHA cholesterol treatment guidelines have introduced a new cardiovascular risk assessment approach (PCE) and have revisited the threshold for prescribing statins. This study aims to compare the ex ante application of the ACC/AHA and the ATP-III guideline models by using a multiethnic case-control study. Methods: ATP-III-FRS and PCE were assessed in 739 patients with first STEMI and 739 age- and gender-matched controls; the proportion of cases and controls that would have been eligible for statin as primary prevention therapy and the discriminatory ability of both models were evaluated. Results: The application of the ACC/AHA compared to the ATP-III model, resulted in an increase in sensitivity [94% (95%CI: 91%–95%) vs. 65% (61%–68%), p< 0.0001], a reduction in specificity [19% (15%–22%) vs. 55% (51%–59%), p< 0.0001] with similar global accuracy [0.56 (0.53–0.59) vs.0.59 (0.57–0.63), p ns]. When stratifying for ethnicity, the accuracy of the ACC/AHA model was higher in Europeans than in Chinese (p = 0.003) and to identified premature STEMI patients within Europeans much better compared to the ATP-III model (p = 0.0289). Conclusion: The application of the ACC/AHA model resulted in a significant reduction of first STEMI patients who would have escaped from preventive treatment. Age and ethnicity affected the accuracy of the ACC/AHA model improving the identification of premature STEMI among Europeans only.
According to the ATP-III guideline model, about one-third of patients with STEMI would not be eligible for primary preventive treatment before STEMI.
The application of the new ACC/AHA cholesterol treatment guideline model leads to a significant reduction of the percentage of patients with STEMI who would have been considered at lower risk before the STEMI.
The global accuracy of the new ACC/AHA model is higher in the Europeans than in the Chinese and, moreover, among the Europeans, the application of the new ACC/AHA guideline model also improved identification of premature STEMI patients.
Key messages
Introduction
Cardiovascular disease (CVD) is the leading cause of mortality worldwide(Citation1,Citation2). Furthermore, both the incidence of CVD and the prevalence of CV risk factors are increasing in low-income countries, such as in China(Citation3,Citation4).
In order to apply effective CVD prevention strategies, the accurate identification of individuals at high risk is mandatory. A large meta-analysis, showed that a large proportion of Coronary Heart Disease (CHD) patients had at least one conventional risk factor (Citation5) but identifying high risk patients based on the simple sum of risk factors, is limited. Conversely, a global CV risk approach using risk estimation models, is recommended by all major prevention guidelines, improving the accuracy of CVD risk profiling and the cost-effectiveness even in resource constrained settings(Citation6).
A joint task force for the American College of Cardiology and the American Heart Association (ACC/AHA) published new guidelines in 2013 for treating blood cholesterol to reduce the risk of CVD in adults (Citation7). This document represents a major shift in the approach and management of plasma cholesterol as compared to the Adult Treatment Panel III (ATP-III) recommendations (Citation8). Together, a new risk estimation system, the Pooled Cohort Equations (PCE), was introduced, adding stroke as an endpoint and lowering the risk threshold for statin treatment in asymptomatic individuals (Citation9).
On the wake of the strong debate aroused after this novel approach (Citation10–17), several investigations addressed the potential implications of applying the new ACC/AHA guidelines in the population (Citation18–22). In particular, the resulting potential increase in the number of eligible individuals for primary preventive therapy with statins had raised several concerns.
The purpose of the present study is to compare ex ante the applicability of the ACC/AHA and the ATP-III guideline models in a clinical setting through a multi-ethnic multicenter case-control study (First Acute Myocardial Infarction (FAMI) Study) that included European and Chinese individuals with ST-Elevation Myocardial Infarction (STEMI) as their first clinical CHD manifestation.
Furthermore, we sought to investigate whether ethnicity might have an effect on the ability of the new guideline model for guiding the initiation of statin therapy. Finally, we compared two ethnic groups, European and Chinese, with known different cardiovascular risk for whom the risk assessment scoring has not been specifically developed, in order to test the applicability of the widespread use of both guideline models in a clinical setting.
Methods
Study population
The analysis was performed using the framework of the FAMI study, a multiethnic, multicenter, observational, prospective study. The FAMI study enrolled individuals with STEMI occurring as their first manifestation of coronary artery and age- and sex-matched apparently healthy controls from urban areas of Italy, Scotland and China. The rationale and design of the FAMI study have been described elsewhere (Citation23).
All patients, irrespective of age, who arrived in hospital within 6 h of symptom onset of STEMI, were screened and the patients with electrocardiographic evidence of STEMI, no previous history of CHD, and symptom onset of <6 h were enrolled in the study. One control subject matched for age (up to 5 years older or younger), sex, and environment (enrolled from the same city) was recruited for each index case. Inclusion criteria for control subjects included no previous diagnosis of coronary disease or history of exertional chest pain.
A total of 2190 subjects (both patients and controls) were enrolled between October 2002 and April 2007. After thorough checking for inclusion criteria, completeness of data and availability of properly prepared and stored blood samples, 739 patients and 739 accurately matched control subjects were finally included in this analysis.
Of the 739 patients and respective controls, 272 were Italian, 157 came from Scotland and 310 from China. In order to compare guideline application in the different ethnic populations, we grouped Italians and Scottish individuals as representative of the European population. Both Italy and United Kingdom are considered countries at low risk for the European risk charts with an updated closer risk of CHD and, indeed, in the FAMI study, the prevalence and distribution of risk factors of the STEMI patients, as well as the controls, were similar between Italians and Scottish.
We also focused the analysis on a younger cohort of individuals with premature STEMI, defined as men age ≤55 years and women age ≤65 years with STEMI, following the criteria of premature CHD as applied to the definition of the family history for CHD.
The FAMI Study was approved by appropriate regulatory and ethics committees in all participating centres, and in all three countries. All participants provided informed consent before taking part in the study.
Variables description and risk assessment
At admission, a standardized structured questionnaire was administered, and physical examinations were undertaken in the same manner in cases and control subjects. Information about personal or family history of CHD, self-reported traditional cardiovascular risk factors (smoking, diabetes, dyslipidaemia, and hypertension) and therapy was obtained.
The blood pressure used for estimation of risk was measured in a stable phase, after recovery from the acute phase or just before hospital discharge.
Non-fasting blood samples (50 ml) were collected before reperfusion strategies within 6 h from symptoms onset in order to minimize acute event-related changes in plasma lipid profile. After separation, microaliquots of serum, sodium-citrate plasma, heparin plasma, and whole blood were frozen immediately at −80 °C. Fasting blood samples were drawn from each control subject and processed similarly. Serum samples from all countries were analysed at the Università Vita-Salute San Raffaele Core laboratory for total cholesterol, low-density lipoprotein (LDL) cholesterol, high-density lipoprotein (HDL) cholesterol, triglycerides, ApoB-lipoprotein and ApoA1-lipoprotein. We considered dyslipidaemic, all patients with total cholesterol levels higher than 200 mg/dl, since prevalence of dyslipidaemia based on self-reported information was largely underestimated.
Risk assessment
Using the continuous ATP-III risk prediction model based on age, systolic blood pressure, treatment of hypertension, total and HDL cholesterol levels, and current smoking, we calculated the 10-year risk of hard CHD. The risk thresholds used for categorization were 10% and 20%, corresponding to the cut-off points for defining the intermediate- and high-risk categories by the ATP-III guideline.
Individuals with diabetes mellitus or other clinical forms of atherosclerotic disease (peripheral arterial disease and symptomatic carotid artery disease) were automatically considered to carry a risk for major coronary events equal to that of established CHD, i.e., >20% per 10 years.
We also calculated the 10-year risk of events related to arteriosclerotic CVD (ASCVD) for each individual based on age, systolic blood pressure, treatment of hypertension, total and HDL cholesterol levels, current smoking, and history of diabetes mellitus, using the sex-specific parameters from the ACC/AHA PCE. We used the recommended 5% and 7.5% risk thresholds for categorization of the two respective categories of “treatment considered” and “treatment recommended.” To comply with the ACC/AHA guidelines, the risk estimation for hard ASCVD was calculated among individuals with CVD at baseline and had LDL cholesterol levels below 190 mg/dL.
Based on each guideline, we formed three categories of treatment:
treatment recommended, including all individuals for whom pharmacological intervention is indicated with a strong level of evidence;
treatment considered, composed by those for whom the decision to prescribe statins is remitted to the physician on the basis of additional factors that can be evaluated;
no treatment, including all the remaining subjects who did not deserve pharmacological therapy, even if they may benefit from lifestyle interventions.
Statistical analysis
Continuous variables are presented as mean with standard deviation (±SD) or as median with interquartile (IRQ) range (25°–75°) if more appropriate (non-normal distribution).
Continuous variables, which are normally distributed, were compared using the Student t test for independent samples. When the variable distribution was not normal, Mann–Whitney U test for independent samples was used.
The proportion of the categorical variables was compared using a Chi-square analysis or Fisher’s exact test, as appropriate. A p value <0.05 was considered statistically significant. Estimated odds ratios and accompanying 95% confidence intervals (95%CI) are presented for each class of the variables that resulted significant at the univariate analysis.
We assessed the sensitivity, specificity and the discrimination of each risk prediction model in our population. Sensitivity measures the proportion of actual patients that are correctly identified as such. Specificity measures the proportion of controls that are correctly identified as such. Discrimination refers to the ability of the model to assign a higher risk to individuals who develop the outcome of interest compared with those who remain free of disease. The discriminative performance of each risk-scoring model was assessed using the AUC (area under the ROC curve).
Statistical analysis and graphics were produced with JMP (version 11, SAS Institute Inc. 2013 Cary, NC) and MedCalc (version 12.2, MedCalc Software, Ostend, Belgium).
Results
Baseline characteristics
shows detailed baseline characteristics of the whole study population and each ethnic group. Due to accurate matching, ages and gender were similar between patients and controls. Each ethnic group had the same age and gender distribution.
Table 1. Baseline characteristics of patients and controls, overall and for each ethnic groups.
The prevalence of risk factors was significantly higher in patients than in controls. Both European and Chinese patients with STEMI showed similar prevalence of number of risk factors (RF) with the majority having two RF while patients with 0–1 RFs were 38% in Europe and 36% in China (Supplementary Figure 1).
Risk assessment and discriminatory ability analysis
The 10-year risk was assessed according to the two different risk assessment scores (ATP-III-FRS and PCE). The mean risk score was significantly higher in STEMI patients than in controls, regardless the method used to estimate it (Supplementary Table S1).
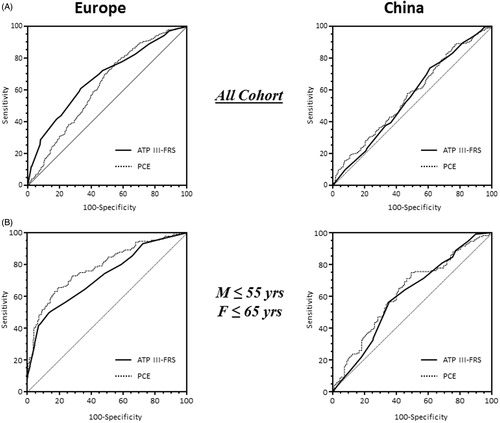
As shown in and detailed in Supplementary Table S2, the discriminatory ability of the ATP-III scoring was higher than the PCE [AUC (95%CI): 0.67 (0.64–0.71) vs 0.63 (0.59–0.66); p = 0.0004, respectively] in the European population, whereas there was no difference between the ATP-III and the PCE in the Chinese [AUC (95%CI): 0.55 (0.51–0.59) vs 0.57 (0.53–0.61); p = 0.3, respectively].
Figure 1. Receiver-operator characteristic curves. Receiver-operator characteristic (ROC) curves of ATP-III-FRS and PCE based risk score in the whole study population (Panel A) and in patients with premature STEMI and controls (Panel B) according to ethnicity (Europe and China). M: males; F: females; ATP-III-FRS: adult treatment panel III-Framingham Risk Score; PCE: Pooled Cohort Equations.
Supplementary Table S3 describes the criteria used by the ATP-III and ACC/AHA guidelines, respectively, to stratify both patients and controls in different risk categories in order to address the ex ante potential primary preventive intervention.
As shown in Supplementary Table S4, in the overall population, the ATP-III guideline model included 57.9% of patients and 38.6% of controls in the “treatment recommended” group, 10.7% of patients and 14.9% of controls in the “treatment considered” group. 31.4% of patients and 46.5% of controls were categorized in the “no treatment” group.
Instead, according to the ACC/AHA guideline model, 78.6% of patients and 63.1% of controls were included in the “treatment recommended” category, while the “treatment considered” group comprised 16.0% of patients and 22.6% of controls. Only 5.4% of patients and 14.3% of controls were assigned to the “no treatment” category.
Overall (Supplementary Figure 2a) and within each ethnic group (), the new ACC/AHA guideline model significantly reduced the number of patients with STEMI that would have escaped from potential primary preventive strategy, in spite of a significant increase in the proportion of matching controls for whom pharmacological treatment would have been recommended.
Figure 2. Histograms represent the distribution of categories of attributable treatment recommendations according to ATP-III and ACC/AHA guidelines in STEMI patients (Panels A and C) and controls (Panels B and D) divided by each ethnic group. White, light grey and dark grey bars denote the ‘treatment recommended’, ‘treatment considered’, and ‘no treatment’ categories, respectively. Histograms of all-ages STEMI and premature STEMI who would not be eligible for statin therapy are highlighted and percentages are nearby reported in panel A and panel C, respectively. Histograms of all-ages population controls and younger controls who would be eligible for statin treatment are highlighted and percentages are nearby reported in panel B and panel D, respectively. ATP-III: adult treatment panel III model; ACC/AHA: American College of Cardiology/American Heart Association guidelines model.
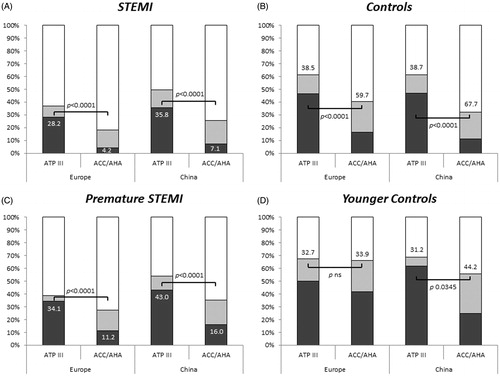
Therefore, sensitivity, specificity and the discrimination ability of each model were also assessed. As shown in , both in the overall population and in the different ethnic groups, sensitivity was significantly higher in the ATP-III than in the ACC/AHA guideline model; whereas the opposite trend was observed for specificity. The discrimination ability of the two models was similar in the whole population and within the ethnic groups while the ACC/AHA guideline model had a better accuracy in the European group than in Chinese one [AUC (95%CI): 0.58 (0.55–0.62) vs 0.53 (0.48–0.57); p = 0.003, respectively] ().
Table 2. Sensitivity and specificity of each guidelines model.
Table 3. Comparison of discrimination ability for each guidelines model.
Patients with premature STEMI
We conducted the same analyses in patients with premature STEMI, defined as men age ≤55 years and women age ≤65 years, composed of 298 (40.3%) cases (161 Europeans and 137 Chinese), and of 306 (41.4%) controls (168 Europeans and 138 Chinese). Premature STEMI patients and their controls had similar mean age and gender distribution: 49.0 ± 6.7 vs 49.3 ± 6.6 years and 79.2% vs 79.1% males, respectively. No differences in age and gender distribution were observed between patients and controls belonging to different ethnic subgroups.
In this younger population, both in the whole cohort and within the ethnic groups, the mean risk was significantly higher in patients than in controls, regardless the assessment tool used (Supplementary Table S1).
As shown in and in Supplementary Table S2, the discriminatory ability of both the ATP-III FRS and the PCE was higher in the Europeans than in the Chinese. Unlike what was observed in the overall population, in the European group the discriminatory ability of the PCE to identify premature STEMI patients resulted significantly higher than the ATP-III scoring [AUC (95%CI): 0.79 (0.74–0.83) vs 0.72 (0.67–0.77); p = 0.0001, respectively].
In the premature STEMI population, according to the ATP-III guidelines, the “treatment recommended” group included 54.4% of patients and 32.0% of controls, the “treatment considered” group included 7.4% of patients and 12.8% of controls while 38.2% of patients and 55.2% of controls were categorized in the “no treatment” group (Supplementary Table S5 and Supplementary Table S6). Compared to the whole population there was only a slight increase in the percentage of subjects who would be excluded from treatment.
As a comparison, using the ACC/AHA guideline model, 69.1% of STEMI patients and 38.6% of controls were categorized in the “treatment recommended” group and the “treatment considered” group included 17.5% of patients and 27.4% of controls. The “no treatment” category included the remaining 13.4% STEMI patients and 34.0% controls.
Similarly to what was observed in the previous analysis considering the entire cohort, even in this younger cohort, the proportion of patients with premature STEMI who would be excluded from treatment decreased significantly, from 114 (38.2%) with the ATP-III guidelines to 40 (13.4%) with the ACC/AHA guidelines (p< 0.0001). However, unlike the entire population, in this group, the number of controls that would be eligible for treatment according to both guideline models was comparable [ATP-III: 98 (32.0%) vs ACC/AHA guidelines 118 (38.6%), p = 0.1079, respectively] (Supplementary Table S6, Supplementary Figure 2b).
The application of the ACC/AHA guideline model significantly increased sensitivity compared to the ATP-III model in the overall population, the younger one and in both ethnic groups. Of note, however, in the younger European group, the increase in sensitivity with the application of the ACC/AHA model was not associated with a significant reduction in specificity, which, on the contrary, was observed in all the other groups ().
Consequently, in the younger European population, the discriminatory ability of the ACC/AHA guideline model to identify patients with premature STEMI, in addition to being higher than in the younger Chinese group [AUC (95%CI): 0.71 (0.66–0.76) vs 0.58 (0.52–0.64); p = 0.0017, respectively], was better than the ATP-III model [AUC (95%CI): 0.71 (0.66–0.76) vs 0.62 (0.57–0.68); p = 0.0289, respectively] ().
Discussion
The ex ante application of the new ACC/AHA guideline model in a multi-ethnic, case-control study population showed a different clinical impact of the PCE compared to the ATP-III ranking model regarding the performance characteristics and discrimination ability to identify subjects who would be eligible for primary preventive therapy with statins; this effect was significantly affected by ethnicity and age. The design of the FAMI study, which enrolled patients with blood samples obtained before reperfusion strategies within 6 h from symptoms onset, minimizes the possibility of acute changes in plasma lipid profile (Citation24) and allows a careful and unique analysis of the pre-STEMI CVD risk.
The application of the ACC/AHA model would lead to a significant reduction of the percentage of patients with STEMI who would have been considered at lower risk before the STEMI and, therefore, for whom primary preventive treatment would not have been recommended. According to the ATP-III guidelines, non-eligible patients were 234 (31.4%) [121 European (28.2%) and 111 Chinese (35.9%)] while, using the ACC/AHA guideline model, the number decreased to only 40 STEMI patients (5.4%) [18 European (4.2%) and 22 Chinese (7.1%)]. This gain resulted in an observed significant increase in sensitivity from the ATP-III to the ACC/AHA model in both ethnic groups. However, the application of the ACC/AHA guidelines compared to the ATP-III guidelines led to a twofold increase of the overall proportion of controls eligible for statin treatment, while the amount of STEMI patients, which were not eligible ex ante, decreased by six-fold.
This gain, however, as a consequence, brings a significant loss in specificity with the ACC/AHA model in both ethnic groups.
The discriminatory ability of the two models was similar within each ethnic group but the application of the ACC/AHA model was more accurate in the European population. These findings suggest that the implementation of the new ACC/AHA guidelines, compared to the ATP-III ones, might improve sensitivity without affecting the global accuracy. This net result might still be useful as an optimal screening tool that should provide the highest possible sensitivity whilst specificity can be improved subsequently through complementary more specific strategies to avoid overtreatment of controls.
Among the premature STEMI population, application of the ACC/AHA model compared to the ATP-III also resulted in a similar significant increase in sensitivity for both ethnic groups, but the reduction in specificity was only observed in the Chinese population. This leads to a significant improvement in the accuracy of the ACC/AHA model compared with the ATP-III in identifying premature STEMI patients within the European population. This higher discrimination ability of the ACC/AHA guidelines supports the usefulness of this model in younger individuals and, likewise, confirms the limits of the application of the ACC/AHA guideline model in the elderly population, as recently suggested (Citation18,Citation19).
Our study, by testing the discrimination ability of the guidelines in a case-control study, does not allow to fully assess the calibration of the risk prediction models. However, it provides a picture frame of the real world, and indeed reflects the expected findings from the application of the ACC/AHA guidelines on CV prevention in population-based studies (Citation18–22). Our study provides complementary insights to those observations adding comprehensive data regarding the potential discriminating performance of the models in individuals with premature STEMI as well as in different ethnic populations. Others’ works previously tested the applicability of the ACC/AHA guidelines with a main focus on sensitivity but not specificity. The potential selection bias of the control population might limit the assessment of the absolute specificity value of each model in our study. However, relative changes in specificity between the two models and the impact of age and ethnicity can be assessed and these findings provide new information regarding the clinical applicability of the ACC/AHA guideline model in the real world.
Pencina et al. (Citation18) estimated in 12.8 million the number of US individuals who would be eligible for statin therapy according to the ACC/AHA guidelines in a cohort from the US National Health and Nutrition Examination Surveys. Compared to the expected event rates predicted by the ATP-III, the authors reported that the application of the new guidelines resulted in higher sensitivity, increasing the number of adults who would be eligible for statin therapy among those expected to have future cardiovascular events, but decreased in specificity, raising the number of adults receiving therapy who are not expected to have events. The increase of statin eligibility seen in this cohort mostly occurred among older adults without CVD who would be eligible for statin only on the basis of a 10-year risk of more than 7.5% assessed by the PCE.
Previously, Mortensen and Falk (Citation20) evaluated the performance of US and European primary prevention guidelines, as a “reality check” in a European cohort of non-diabetic patients with first myocardial infarction. Moreover, this study confirmed the higher number of patients who would have been eligible for primary prevention with statins by following the ACC/AHA compared to the ESC guidelines, but the analysis was only limited to the detection rate (sensitivity) of risk-based potential eligibility recommended by the guidelines, not including specificity, and the thus the risk of overtreatment.
A similar work was done by Kavousi et al. (Citation19) who compared the application of the ACC/AHA, the ATP-III, and the ESC guidelines in a cohort of Dutch individuals aged 55 years or older. The authors found that the ACC/AHA guidelines would recommend statins for nearly all men and two-thirds of women, proportions exceeding those with the ATP-III or ESC guidelines.
In contrast to the studies mentioned above, we could not apply the ESC guidelines assessment because the SCORE system estimates the 10-year risk of a first fatal atherosclerotic event while the FAMI study encompasses patients with non-fatal STEMI and therefore fits better with ATP-III and PCE endpoint assessment.
More recently, DeFilippis et al. (Citation22) analysed 4227 non-diabetic patients included in the contemporary cohort of Multi-Ethnic Study of Atherosclerosis comparing the observed event rates, during 10-year follow-up, with the expected estimation event rate based on 5 risk scores assessment. PCE and 3 Framingham-based risk scores overestimated cardiovascular events. Among several potential reasons, the inclusion of Chinese Americans and Hispanic Americans in the analysed cohort might have contributed to the observed overestimation since the PCE has been developed using data provided from five longitudinal, population-based cohorts of African American and white-Americans, as the Framingham risk score was done.
Consistent with this hypothesis, our results showed that the ACC/AHA guideline model was more accurate in the Europeans than in the Chinese.
This finding is of high relevance because of the evidence of the increased rate of hospital admissions for STEMI and for the increased risk factor prevalence in China during the past decade (Citation4). The implication of this observation is that specific primary preventive strategies need to be developed taking into account the ethnic-specific models rather than simply translating the western model.
More importantly, when the analysis is focused on premature STEMI, our data indicate that the application of the ATP-III model in younger adults, compared to the overall population, did not show significant differences in sensitivity and discriminatory ability while Akosah et al. (Citation25) reported that the ATP-III guidelines underappreciate CV risk in young adults. These findings strengthen the clinical value of the application of the ACC/AHA model to improve the discriminatory ability for the detection of patients with premature STEMI that we observed within the European population.
Conclusions
Our analysis indicate that: (1) the application of the 2013 ACC/AHA guidelines on CVD prevention would result in a significant reduction in the proportion of patients with STEMI who would have escaped from a preventive strategy accompanied by a potential overtreatment of healthy subjects, (2) the discriminatory ability of the ACC/AHA model is significantly affected by age and ethnicity, (3) despite these aspects, the new ACC/AHA guidelines were more accurate than the ATP-III model to identify patients with premature STEMI among European individuals, further supporting a clinical benefit.
Lowering the treatment threshold, in spite of similar accuracy, potentially results in the overtreatment of healthy subjects and this remains a point of discussion (Citation18,Citation19,Citation26–28). However, the new ACC/AHA guidelines perform better in identifying patients with premature STEMI representing a key population who will definitely benefit by primary prevention strategy.
In a period of restriction of healthcare resources, the results of our study suggest that the new ACC/AHA model on CVD prevention might be a simple as well as a cost-effective first-line tool for a more accurate identification of patients at higher risk of STEMI only when applied in appropriate populations, such as younger and Western individuals. Whereas, the widespread application of the model, following the “one size fits all” paradigm, might be inaccurate thus causing overtreatment and decreased cost-effective prevention.
Acknowledgements
We are grateful for the expert technical assistance of Dr. Marina Celada (SAS Institute, Milan, Italy).
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article.
References
- Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Blaha MJ, et al. Executive summary: heart disease and stroke statistics—2014 update: a report from the American Heart Association. Circulation. 2014;129:399–410.
- Roger VL, Go AS, Lloyd-Jones DM, Adams RJ, Berry JD, Brown TM, et al. Heart disease and stroke statistics-2011 update: a report from the American Heart Association. Circulation. 2011;123:e18–209.
- Yang Z-J, Liu J, Ge J-P, Chen L, Zhao Z-G, Yang W-Y. Prevalence of cardiovascular disease risk factor in the Chinese population: the 2007–2008 China National Diabetes and Metabolic Disorders Study. Eur Heart J. 2012;33:213–20.
- Li J, Li X, Wang Q, Hu S, Wang Y, Masoudi FA, et al. China PEACE Collaborative Group. ST-segment elevation myocardial infarction in China from 2001 to 2011 (the China PEACE-Retrospective Acute Myocardial Infarction Study): a retrospective analysis of hospital data. Lancet. 2014;2011:1–11.
- Khot UN, Khot MB, Bajzer CT, Sapp SK, Ohman EM, Brener SJ, et al. Prevalence of conventional risk factors in patients with coronary heart disease. JAMA. 2003;290:898–904.
- Mendis S, Lindholm LH, Anderson SG, Alwan A, Koju R, Onwubere BJ, et al. Total cardiovascular risk approach to improve efficiency of cardiovascular prevention in resource constrain settings. J Clin Epidemiol. 2011;64:1451–62.
- Stone NJ, Robinson JG, Lichtenstein AH, Bairey Merz CN, Blum CB, Eckel RH, et al. American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129:S1–45.
- Executive Summary of the Third Report (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA. 2001;285:2486–97.
- Goff DC, Jr, Lloyd-Jones DM, Bennett G, Coady S, D'Agostino RB, Gibbons R, et al. American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129:S49–73.
- Ridker PM, Cook NR. Statins: new American guidelines for prevention of cardiovascular disease. Lancet. 2013;382:1762–5.
- Keaney JF, Curfman GD, Jarcho JA. A pragmatic view of the new cholesterol treatment guidelines. N Engl J Med. 2014;370:275–8.
- Downs J, Good C. New cholesterol guidelines: has Godot finally arrived? Ann Intern Med. 2014;160:354–5.
- Martin SS, Blumenthal RS. Concepts and controversies: The 2013 American College of Cardiology/American Heart Association Risk Assessment and Cholesterol Treatment Guidelines. Ann Intern Med. 2014;160:356–8.
- Guallar E, Laine C. Controversy over clinical guidelines: listen to the evidence, not the noise. Ann Intern Med. 2014;160:361–2.
- Psaty BM, Weiss NS. 2013 Acc/Aha guideline on the treatment of blood cholesterol: a fresh interpretation of old evidence. JAMA. 2014;311:461–2.
- Ioannidis JA. More than a billion people taking statins? Potential implications of the new cardiovascular guidelines. JAMA. 2014;311:463–4.
- Montori VM, Brito JP, Ting HH. Patient-centered and practical application of new high cholesterol guidelines to prevent cardiovascular disease. JAMA. 2014;311:465–6.
- Pencina MJ, Navar-Boggan AM, D'Agostino RB, Sr, Williams K, Neely B, Sniderman AD, et al. Application of new cholesterol guidelines to a population-based sample. N Engl J Med. 2014;370:1422–31.
- Kavousi M, Leening MJ, Nanchen D, Greenland P, Graham IM, Steyerberg EW, et al. Comparison of application of the ACC/AHA guidelines, Adult Treatment Panel III Guidelines, and European Society of Cardiology Guidelines for cardiovascular disease prevention in a European cohort. JAMA. 2014;311:1416–23.
- Mortensen MB, Falk E. Real-life evaluation of European and American high-risk strategies for primary prevention of cardiovascular disease in patients with first myocardial infarction. BMJ Open. 2014;4:e005991.
- Ray KK, Kastelein JJ, Boekholdt SM, Nicholls SJ, Khaw KT, Ballantyne CM, et al. The ACC/AHA 2013 guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular disease risk in adults: the good the bad and the uncertain: a comparison with ESC/EAS guidelines for the management of dyslipidaemias 2011. Eur Heart J. 2014;35:960–8.
- DeFilippis AP, Young R, Carrubba CJ, McEvoy JW, Budoff MJ, Blumenthal RS, et al. An analysis of calibration and discrimination among multiple cardiovascular risk scores in a modern multiethnic cohort. Ann Intern Med. 2015;162:266–75.
- Cristell N, Cianflone D, Durante A, Ammirati E, Vanuzzo D, Banfi M, et al. FAMI Study Investigators. High-sensitivity C-reactive protein is within normal levels at the very onset of first ST-segment elevation acute myocardial infarction in 41% of cases. J Am Coll Cardiol. 2011;58:2654–61.
- Pitt B, Loscalzo J, Ycas J, Raichlen JS. Lipid levels after acute coronary syndromes. J Am Coll Cardiol. 2008;51:1440–5.
- Akosah KO, Schaper A, Cogbill C, Schoenfeld P. Preventing myocardial infarction in the young adult in the first place: how do the national cholesterol education panel III guidelines perform? J Am Coll Cardiol. 2003;41:1475–9.
- Blaha MJ, Blumenthal RS. Risk factors: new risk-assessment guidelines-more or less personalized? Nat Rev Cardiol. 2014;11:136–7.
- Amin NP, Martin SS, Blaha MJ, Nasir K, Blumenthal RS, Michos ED. Headed in the right direction but at risk for miscalculation: a critical appraisal of the 2013 ACC/AHA risk assessment guidelines. J Am Coll Cardiol. 2014;63:2789–94.
- Navar-Boggan AM, Peterson ED, D'Agostino RB, Sr, Pencina MJ, Sniderman AD. Using age- and sex-specific risk thresholds to guide statin therapy: one size may not fit all. J Am Coll Cardiol. 2015;65:1633–9.
