Abstract
Blood pressure treatment has shown great efficacy in reducing cardiovascular events in randomized controlled trials. If this is effective in reducing cardiovascular disease in the general population, is less studied. Between 2001 and 2009 we performed an intervention to improve blood pressure control in the county of Västerbotten, using Södermanland County as a control. The intervention was directed towards primary care physicians and included lectures on blood pressure treatment, a computerized decision support system with treatment recommendations, and yearly feed back on hypertension control. Each county had approximately 255 000 inhabitants. Differences in age and incidence of cardiovascular disease were small. During follow-up, more than 400 000 patients had their blood pressure recorded. The mean number of measurements was eight per patient, yielding a total of 3.4 million blood pressure recordings. The effect of the intervention will be estimated combining the blood pressure data collected from the electronic medical records, with data on stroke, myocardial infarction and mortality from Swedish health registers. Additional variables, from health registers and Statistics Sweden, will be collected to address for confounders. The blood pressure data collected within this study will be an important asset for future epidemiological studies within the field of hypertension.
Introduction
Cardiovascular disease is the major cause of death worldwide.[Citation1,Citation2] Elevated blood pressure (BP) is the most important risk factor for cardiovascular disease, contributing to approximately 50% of excess strokes and myocardial infarctions, and 7% of total deaths.[Citation3,Citation4] From meta-analyses of randomized controlled trials of antihypertensive agents, it is established that a BP reduction of 10/5 mmHg reduces the risk of stroke by around 40%, and the risk of myocardial infarction by around 20%, independent of age, gender, ethnicity and associated diseases.[Citation5] However, the setting of randomized controlled trials differs in many ways from that of clinical practice. For example, the sample of patients included in randomized controlled trials are often highly selected in terms of age and comorbidities, the patients are encouraged to take their medications more actively and BP is measured in a highly standardized way on a regular basis.[Citation6,Citation7] On the other hand, usual care often struggles with patient non-adherence and suboptimum treatment, owing to a lack of knowledge or defensive treatment attitudes among physicians.[Citation8,Citation9] To our knowledge, the external validity of antihypertensive trials, i.e. whether a BP reduction in a usual care setting converts into a reduced incidence of stroke, has never been tested on a population basis. Hence, we initiated the Swedish Stroke Prevention Study (SSPS), with the aim of testing whether education and feedback to primary care physicians in one county would (i) reduce BP, and (ii) reduce the incidence of stroke, compared to a similar county not undergoing the intervention.
The introduction of electronic medical records confers a historically unique possibility to collect large amounts of data from whole populations.[Citation10] Hence, a secondary objective was to create a database of all BPs measured in primary care in the intervention and control counties. First, this was essential to be able to evaluate our intervention. Secondly, a database of all BP recordings, from two independent counties, would in itself be a valuable resource for future research.
Materials and methods
Study design
The SSPS was a non-randomized intervention study, comparing the effects of education and feedback to primary care physicians in one county, with no intervention in another county. The intervention took place from 2001 to 2009. Primary outcomes were BP, measured in primary care, and incidence of stroke, measured through the Swedish Hospital Discharge Register (SHDR) and the Swedish Cause of Death Register (SCDR). Secondary outcomes were myocardial infarction and mortality, measured through the same registers, and prescribed antihypertensive agents, collected from the state-owned pharmacy company (Apoteket AB) and the National Board of Health and Welfare.
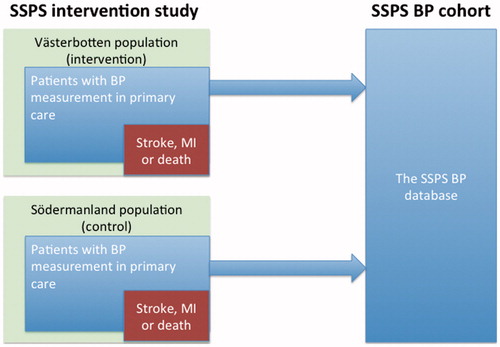
In addition to the intervention study, a BP database was created, including all BP recordings since the introduction of electronic medical records in 1992/1993, until the end of December 2011. The patients with BPs recorded in the database thus constitute an observational open cohort, referred to as the SSPS BP cohort (). Thus, the BPs recorded in the studies are all BPs measured in routine clinical practice and are the BPs that the clinicians have used for decision making.
Figure 1. Overview of the SSPS project. To the left, the SSPS intervention study. All patients with registered BP (white) respectively stroke, myocardial infarction or death (black) are extracted for each county separately. To the right, the SSPS BP cohort. All BP measurements from both counties, collected during an extended time period, will be merged into a large database. BP = blood pressure, MI = myocardial infarction.
Participants and settings
In the intervention county of Västerbotten, all doctors at the 33 public health centres present at the start of the intervention, with positions for about 125 general practitioners and 50 residents, participated. There were less than 5% doctors in private practice in that county, and their patients’ BP data were not included. In the control county of Södermanland, data from all 29 public health centres present at the start of the intervention, with around 130 positions for general practitioners and 30 for residents, were included. There were less than 10% doctors in private practice in the control county, and their patients’ BP data were not included. During the study period some health centres have closed, and new ones have opened. Also, some health centres have merged. All patients who had ever had their BP recorded, by a doctor or any other staff category, in any of the included health centres during the study period, were included in the cohort.
Intervention
The intervention started in 2001 with the implementation of a computerized decision support system (DSS) for selecting and combining antihypertensive drugs according to the current hypertension guidelines at the time.[Citation11] This support system was installed in all doctors’ computers, in all public health centres in the intervention county of Västerbotten, but not in the control county (Södermanland), and was updated regularly. Moreover, in the intervention county, all health centres were visited by the research group in 2004, and given a description of the project followed by lectures and discussion about principles for drug treatment of hypertension, including treatment goals. The key messages in these lectures were:
Establish a BP goal together with the patient. This emphasizes the patient’s own responsibility for treatment success. A treatment goal of < 140/90 mmHg (and < 130/80 mmHg for patients with diabetes) was encouraged.
At the first consultation, inform the patient that he/she eventually is expected to need on average three different antihypertensive drugs to reach the BP goal.
Add an additional antihypertensive agent every time the BP is above the goal level.
If BP is still above the goal at the next visit, the next action should already have been documented in the medical record at the first visit.
Shorten the time lag between measuring a BP above the treatment goal and adding another antihypertensive drug.
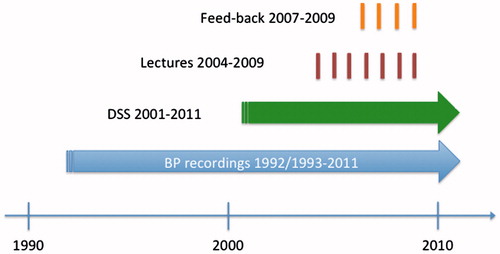
Most primary care doctors and nurses in the intervention county attended these meetings. Centres in the intervention area also received annual feedback, from 2007 onwards, on their proportion of well-controlled patients, overall and by gender and age, in comparison with the average for the whole county. During the study period there were follow-up lectures on the global cardiovascular risk, but with a specific focus on high BP management. The intervention programme continued until 2009 ().
Figure 2. Time line. The bottom arrow shows the period of blood pressure data collection in the SSPS BP cohort. The next arrow shows the period during which DSS has been available for general practitioners. The lines show the time of the follow-up lectures, and the time when the health care centers received feed-back on their performance. BP = blood pressure, DSS = decision support system.
Data extraction
We created a script extracting all BPs in the medical record data system (SysTeamCross) in primary care, in Västerbotten and Södermanland counties. The first BP recordings were from 1993 in Västerbotten County and 1992 in Södermanland County. The electronic medical record system was installed at the different public health centres at different times, leading to constantly increasing numbers of measurements recorded in the database per year, from a couple of thousand recordings during the first year to more than 120,000 recordings in each county during 2011. For each BP measurement, several variables were extracted from the database ().
Table 1. List of extracted variables.
The incidences of stroke and myocardial infarction, and mortality, are collected for both counties from the SHDR and the SCDR. The SHDR is maintained by the National Board of Health and Welfare and covers all inpatient care in Sweden since 1987. All patients discharged after a first ever, recurrent or fatal stroke are collected from the SHDR and the SCDR, using the following main diagnoses: 430*, 431*, 434* and 436* [International Classification of Diseases 9 (ICD-9)], I60*, I61*, I63* and I64* (ICD-10). All patients discharged after, or dead due to, a myocardial infarction are collected with the following main diagnosis: 410* (ICD-9) and I21* (ICD-10). The variables extracted from each register are shown in .
Data on prescribed and collected antihypertensive and lipid-lowering drugs in the two counties are collected on a pharmacy-level basis from 1996 to 2006, through the state-owned pharmacy company (Apoteket AB), and on an individual patient level from 2006 onwards, through the Swedish National Board of Health and Welfare.
All citizens in Sweden carry a unique civic number. In our study we use this number to link BP data from the SysTeamCross database with outcome data from the SHDR and SCDR and drug prescription data from the National Board of Health and Welfare. This data linkage makes it possible to associate mean levels, time trends and variations in the BP with distribution and time trends for stroke and myocardial infarction, as well as drugs prescribed, for each patient separately.
Ethical approval
The project has been approved by the Regional Ethical Board at Umeå University (Dnr: 05-060M, 2010-313-32M, 2013-58-32M). Written approval of the study has been received from all health centres in the two counties.
Results
Validation of data extraction
BP values from patients with a diagnosis of hypertension were extracted manually from the electronic medical record system (SYSteam Cross), in the intervention and control counties, by searching fields dedicated to BP recordings. The aim of the validation was to confirm the extracted BP data and to ensure that an adequate number of all recorded BPs was retrieved, i.e. that the script managed to identify all BP measurements in the electronic medical record. In the intervention county, which had a more structured database, 87 patient files (1287 BP measurements) were scrutinized in detail to ensure that most BP measurements were included in our database. The underestimation of number of BP measurements for these patients was 7%. After an update of the script (search algorithm), the underestimation was <5%. In the control county, which had a less structured database, 13,000 BP values were scrutinized with the aim of identifying additional text fields occasionally used for recordings of BP values. In all, 11 additional text fields were identified, and the new search algorithm added in total 150,000 new BP measurements in that county. After this, new databases were extracted from each county for statistical analysis.
The SHDR has been validated in several studies, for many different outcomes. For stroke and myocardial infarction the positive predictive value is generally estimated as high (97–100%), whereas the sensitivity is generally lower (84–98% for stroke and 77–91% for myocardial infarction).[Citation12] One high-quality validation study of the combination of SHDR and SCDR, in the context of stroke, found the sensitivity to be 88% and the specificity to be 92%.[Citation13] Another validation study, against the World Health Organization (WHO) MONICA register in the intervention county of Västerbotten, resulted in a similar estimate.[Citation14]
Baseline data: intervention study
SSPS was an intervention study directed towards primary care doctors, aiming to decrease the BP in the population. Although, in one sense, all inhabitants in Västerbotten and Södermanland counties participate in the study, the intervention probably only affects those who have their BP measured, and mostly those with high BP. Based on the above, both population data ( and characteristics of patients who had their BP measured () are presented for the year before the intervention started (year 2000), for both counties separately. The counties were quite similar with respect to total population, age and gender distribution, but differed slightly in number of recorded events, with Västerbotten having more strokes (1192 vs 1066) and fewer myocardial infarctions (1030 vs 1137) than Södermanland. The patients with recorded BPs were on average 20 years older, and to a larger extent female than the total population (58% vs 51%). The number of measurements in Västerbotten was only 60%% of those in Södermanland during the year 2000, partly reflecting a slower transition to the electronic medical record system.
Table 2. Demographics and cardiovascular burden in the intervention and control counties at baseline (2000).
Table 3. Characteristics of patients with a recorded blood pressure (BP) during the year 2000, baseline before intervention started.
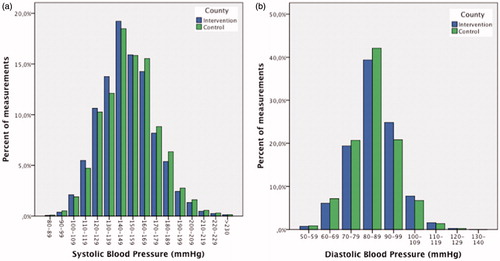
The distributions of systolic and diastolic BPs in both counties are presented in , showing a fair normal distribution, with slight additional preference for the systolic BP interval 140–149 mmHg.
Descriptive data: Swedish Stroke Prevention Study blood pressure cohort
The SSPS BP cohort database comprises all BPs measured in primary care, in Västerbotten and Södermanland, during the electronic medical record era. Detailed data, for both counties separately, are presented in . In total, the database contains approximately 3.4 million BPs for 417,000 patients. The median number of measurements for each patient was 3 in each county, ranging from 1 to 695 with a positive skew distribution. Mean age, gender distribution and the prevalence of diabetes and hypertension showed few differences between the counties. More BPs were measured by doctors in the control area than in the intervention area.
Table 4. Swedish Stroke Prevention Study (SSPS) blood pressure (BP) cohort database (1992/1993–2011).
Discussion
To our knowledge, SSPS is the first controlled study carried out on a population basis to estimate the effectiveness of improved BP control in routine clinical practice, with stroke as the primary outcome variable. It is, in our opinion, a crucial step in evidence-based medicine to establish whether efficacy in trials can be translated into effectiveness in clinical practice.[Citation15] Traditionally, efficacy is tested in trials focusing on optimal internal validity. This inherently limits the general applicability of the results, and demands that treatments proven to be efficacious are later tested in a broader population closer to the usual care setting,[Citation16] The SSPS takes this even further, also addressing communication of evidence and feedback on performance to general practitioners, and the implementation of guidelines in actual clinical practice. It can thus be regarded as one of the first, and definitely the largest, phase V trial in the field of hypertension.[Citation17]
The strength of this study, comparing the intervention in one population with no intervention in another population, is also its major weakness. First, the populations in Västerbotten and Södermanland were not completely equal at baseline. People in Västerbotten suffered from more strokes, and in Södermanland there were slightly more myocardial infarctions, for reasons that cannot be explained solely by differences in age, gender, diabetes or hypertension. Secondly, some geographical differences exist. Västerbotten covers an area about 10 times larger than Södermanland, making it very thinly populated. Also, there is a difference in latitude between the counties, conferring Västerbotten a colder climate. Both urban–rural distribution and climate influence mortality and the incidence of cardiovascular disease.[Citation18,Citation19] Thirdly, on a sociopolitical level, the structural organization of healthcare in Sweden, based on independent county councils, could give rise to differences in healthcare policies. This, in turn, could have an impact on preferred treatments and patterns of referral and admission. Fourthly, in primary healthcare, a public health programme, called the Västerbotten Intervention Programme (VIP), has been running in Västerbotten since 1990.[Citation20] The aim of this programme is to promote a healthy lifestyle among the middle-aged population. We cannot, therefore, exclude the possibility of interactions between our intervention and VIP.
Taking the above into account, SSPS will be important for two reasons. First, it will investigate whether the intervention (DSS, education, data feedback) improves BP control on a population basis. If this is the case, the same model could be applied in other healthcare systems as well. Secondly, if BP control increases, it will provide further insight if this is proven to be efficacious in phase III trials and effective in phase IV trials, and also reduces the incidence of stroke and myocardial infarction in a population setting.
In addition to the intervention study, the SSPS project has generated a unique database, the SSPS BP cohort, including all BPs measured in Västerbotten and Södermanland counties since the introduction of electronic medical records until the end of December 2011. This will be a valuable source of information for epidemiological studies of BP and cardiovascular disease, including time trends and variability measures. Also, because of the unique civic number carried by each individual, these data can be linked to health registers other than the ones mentioned above. It would also be possible to link these data to data from the VIP, including more cardiovascular risk factors such as cholesterol levels, smoking and drinking status, and anthropometric data.[Citation20]
Declaration of interest
No potential conflict of interest was reported by the authors.
Funding information
This project is supported by the Swedish Research Council [K2007-70X-20515-01-3] and the Research Foundation of Västerbotten County Council.
References
- World Health Organization. The global burden of disease. 2004 update. Geneva: WHO; 2008.
- Lozano R, Naghavi M, Foreman K, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2095–2128.
- Lawes CMM, Vander Hoorn S, Rodgers A, International Society of Hypertension. Global burden of blood-pressure-related disease, 2001. Lancet. 2008;371:1513–1518.
- Lim SS, Vos T, Flaxman AD, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2224–2260.
- Law MR, Morris JK, Wald NJ. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomized trials in the context of expectations from prospective epidemiological studies. BMJ. 2009;338:34–52.
- Leber PD, Davis CS. Threats to the validity of clinical trials employing enrichment strategies for sample selection. Control Clin Trials. 1998;19:178–187.
- Rothwell PM. Treating individuals 1 – external validity of randomized controlled trials: “To whom do the results of this trial apply?” Lancet. 2005;365:82–93.
- Caro JJ, Salas M, Speckman JL, et al. Persistence with treatment for hypertension in actual practice. CMAJ. 1999;160:31–37.
- Persson M, Carlberg B, Tavelin B, Lindholm LH. Doctors’ estimation of cardiovascular risk and willingness to give drug treatment in hypertension: fair risk assessment but defensive treatment policy. J Hypertens. 2004;22:65–71.
- Shortliffe EH. The evolution of electronic medical records. Acad Med. 1999;74:414–419.
- Persson M, Bohlin J, Eklund P. Development and maintenance of guideline-based decision support for pharmacological treatment of hypertension. Comput Methods Programs Biomed. 2000;61:209–219.
- Ludvigsson JF, Andersson E, Ekbom A, et al. External review and validation of the Swedish national inpatient register. BMC Public Health. 2011;11:450.
- Appelros P, Terent A. Validation of the Swedish inpatient and cause-of-death registers in the context of stroke. Acta Neurol Scand. 2011;123:289–293.
- Koster M, Asplund K, Johansson A, Stegmayr B. Refinement of Swedish administrative registers to monitor stroke events on the national level. Neuroepidemiology. 2013;40:240–246.
- Glasgow RE, Lichtenstein E, Marcus AC. Why don’t we see more translation of health promotion research to practice? Rethinking the efficacy-to-effectiveness transition. Am J Public Health. 2003;93:1261–1267.
- Flay BR. Efficacy and effectiveness trials (and other phases of research) in the development of health promotion programs. Prev Med. 1986;15:451–474.
- Greenwald P, Cullen JW. The new emphasis in cancer control. J Natl Cancer Inst. 1985;74:543–551.
- Thelin N, Holmberg S, Nettelbladt P, Thelin A. Mortality and morbidity among farmers, nonfarming rural men, and urban referents a prospective population-based study. Int J Occup Environ Health. 2009;15:21–28.
- Gyllerup S, Lanke J, Lindholm LH, Schersten B. High coronary mortality in cold regions of Sweden. J Intern Med. 1991;230:479–485.
- Norberg M, Wall S, Boman K, Weinehall L. The Vasterbotten Intervention Programme: background, design and implications. Global Health Action. 2010;3:4643. doi: 10.3402/gha.v3i0.4643.