Abstract
Several studies have shown that mineral metabolism disorders play a major role in determining a higher mortality rate for end-stage renal disease patients. Vitamin D deficiency is associated with cardiovascular events in hemodialysis patients. Recently, an association between vitamin D insufficiency and cardiovascular or renal events has been found, in patients with chronic renal failure who have not started renal replacement therapy yet. To further investigate this issue, we evaluated the relationship between blood levels of 25-hydroxyvitamin D (25-OH D; > or ≤30 ng/mL) and mortality or dialysis dependence in 104 incident consecutive patients with chronic kidney disease stages 3–5, over a period of 17 months, with a follow-up of 2 years in a cross-sectional analysis. The correlation between different levels of vitamin D and the risk of events has been estimated by using a probit model. Explanatory variables employed concerned age, sex, blood pressure, BMI, and number of co-morbid factors. The average 25-OH D concentration was of 30.13 ng/mL. During follow-up (>16 months), each patient experienced an average of 1.28 events. Vitamin D has been shown to reduce the probability of cardiovascular or renal events. Vitamin D intake for more than 12 months can reduce the probability of such events by 11.42%. Each co-morbid factor, instead, raises the probability of events by 29%. Lower probabilities of experiencing an adverse cardiovascular event might depend on higher levels of vitamin D. The influence of 25-OH D on survival in chronic kidney disease patients may be related to unrecognized factors that need to be further explored.
INTRODUCTION
It is well known that mortality risk for cardiovascular disorders is higher in patients on hemodialysis compared to general population. Several studies have shown that disorders of mineral metabolism appear to be the most important contributors to the high cardiovascular mortality rate in end-stage renal disease patients. Indeed, prevalence of vascular calcification and cardiovascular mortality is nearly the same, with about 50% affected patient population.
Low levels of 25-hydroxyvitamin D (25-OH D), the principal circulating storage form of vitamin D, has been reported in approximately 36% up to 57% of general medicine inpatients in the United States and in more than one-third to one-half of otherwise healthy middle-aged to elderly adults in Europe.Citation1
The principal causes of vitamin D inadequacy are low sunlight exposure, age-related decreases in cutaneous synthesis, and diets low in vitamin D.Citation2
Both epidemiologic and clinical studies suggested that patients with reduced vitamin D intake are at risk of hypertension and diabetes mellitus.Citation3–5 In hypertensive adults exposed to simulated sunlight three times a week for 3 months resulted in an increase in their 25-OH D levels by more than 150% and a significant (6 mmHg) reduction in both systolic and diastolic blood pressure.Citation6
Recent studies have shown other extra-skeletal consequences of vitamin D deficiency. Indeed, it increases the risk of colon, prostate, breast, ovary, esophagus, and several other tissues cancer.Citation1 In particular, it has been suggested that maintenance of a 25-OH D level greater than 20 mg/mL reduces risk of colon, prostate, breast, and ovarian cancer by as much as 30–50%.Citation7 Moreover, vitamin D deficiency is also implicated in autoimmune disorders, such as multiple sclerosis.Citation8
Recently, clinical studies have examined the role of vitamin D levels and its contribution to outcomes in end-stage renal disease patients. In a cross-sectional analysis of 825 consecutive patients, low vitamin D levels were associated with increased mortality. Moreover, untreated 25D- or 1,25D-deficient patients were at significantly increased risk for early mortality, when compared to patients with the highest vitamin D levels who received therapy.Citation9
A 25D serum level of 30 ng/mL or greater is considered to be the optimal level for a better health outcome;Citation10 moreover, this value is considered as the threshold for vitamin D normal status and insufficiency.Citation11
All these reasons led us to examine the association between different vitamin D levels (<30 mg/mL and >30 ng/mL) and mortality in patients with chronic kidney disease (CKD) who had not started hemodialysis yet. We also observed the association between vitamin D deficiency and cardiovascular events, renal death, and hospitalization.
METHODS
Study Sample and Clinical Evaluation
Between September 2006 and January 2008, 104 patients who had been hospitalized at the Policlinico Universitario in Messina underwent measurements of their 25-OH D3 levels. Other records were made during medical visits; clinical events were recorded during the follow-up every 3 months. Such events included cardiovascular events, such as myocardial infarction and stroke, renal death, and hospitalization. Renal death included the need for renal replacement therapy both by means of dialysis and transplant.
Moreover, data on baseline characteristics included diagnosis of renal disease causes, co-morbid conditions such as coronary artery disease, heart failure, peripheral and cerebral vascular disease, hyperlipidemia, malignancy, and chronic obstructive pulmonary disease.
Data were collected as soon as the patients were referred to nephrologists and they were determined by looking at the International Classification of Diseases, Ninth Revision. All patients were in stable clinical conditions at the time of enrollment. Blood samples for vitamin 25-OH D levels were collected at the first referral.
Laboratory
Blood samples were taken in the morning, after an overnight fasting. Selected variables were measured after the samples had been frozen and stored at −80°C. Serum calcium, phosphate, albumin, cholesterol, hemoglobin, and creatinine (Scr) were analyzed in an onsite biochemistry laboratory by using standard auto‐analyzer techniques (Roche Diagnostics Modular IIP, Milan, Italy). Serum-intact parathyroid hormone (iPTH 1–84) levels were determined by using radioimmunoassay (RIA) kit (Radim, Pomezia, Italy). Reference value was 10-59 pg/mL. Serum samples were obtained in the morning. Serum 25-OH D3 levels were measured by isocratic HPLC kit by using a reverse-phase cartridge according to manufacturer's instructions (BioRad, Munchen, Germany).
Glomerular filtration rate was estimated (eGFR) by using the four-variable modification of diet in renal disease formula.
Statistical Analysis
Data have then been used to perform an econometric analysis, whose objective was to look at the correlation between different levels of vitamin D and the risk of events like cardiovascular events and renal death (as mentioned above) that were more likely to occur in patients.
The probability of such events has been estimated by applying probit analysis. Probit models are commonly used when the dependent variable is not observed. In this case the value of such variable is “latent” and a dummy yi can be observed instead.
It is defined by
The observed yi are realizations of a binomial process with probabilities varying from trial to trial and depending on the regressors xij.
The likelihood function can be written as
In the present case, the dependent variable assumes the value 1 if more than one event (cardiovascular event, etc.) occurs and 0 if any event occurs.
The independent variables concern, first of all, different levels of vitamin D (from 0 to 30 and over 30 ng/mL: vitamin D intake for more than 12 months was taken into account); other variables are patients' age, sex, blood pressure, BMI, number of co-morbidities (and some of the most common co-morbid factors, such as coronary artery disease and peripheral vascular disease).
The following is the estimated equation:
Age is the patients' age.
Sex is a dummy variable assuming the value of 1 if the patient is male and of 0 if the patient is female.
Blood pressure has been reported as the median value of the last three measurements.
BMI is the body mass index.
Coronary artery disease and peripheral vascular disease are dummy variables assuming the value of 1 if such co-morbid factors are present and 0 if they are not.
Vitamin D equals to vitamin D levels over 30 ng/mL when it is administered to patients for more than 12 months.
Estimates were checked to test their robustness.
RESULTS
The characteristics of the 104 participants are shown in A and .
Table 1A. Baseline characteristics of the 104 sample patients
Table 1B. Number and type of events
The study population had an average age of 74 ± 13 years and there was a slight prevalence of males (51% vs. 49%). All subjects were Caucasian. Hypertension (48.08%) and diabetes mellitus (34.62%) were among the main reasons for renal failure. Laboratory test included calcium, phosphorus, PTH, albumin, eGFR, and hemoglobin. Liver function was normal for all patients.
The average PTH level was 140.67 (±144.62) and for this reason the majority of patients were started on 1,25D treatment.
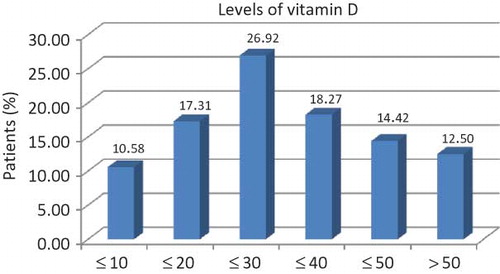
The average serum 25-OH D concentration was of 30.13 ng/mL. The greatest concentration of 25-OH is below 30 ng/mL, with 10.58% of patients presenting with 25-OH D <10 ng/mL (see ).
During a mean follow-up of 16 months, each patient experienced an average of 1.28 events including 12 fatal coronary heart disease events (myocardial infarction, angina, or coronary insufficiency), 2 nonfatal cerebrovascular events (transient ischemic attack), and 16 renal deaths.
Ninety-nine patients were hospitalized and 14 patients died.
First of all, to appreciate the effects of vitamin D administration on patients, the sample was split into two subgroups, according to vitamin D levels (> or <30 ng/mL) (). This subdivision was performed after considering that in the general population the optimal level of 25D is 30 ng/mL or greater, for better health outcomes,Citation10 and it represents the threshold level for vitamin D normal status and insufficiency.Citation11 The two subgroups are homogenous. The t-test is significantly different for some co-morbid factors and for levels of PTH.
Table 2. Characteristics of the two subgroups (25-OH D < or >30 mg/mL)
Evidence suggested looking for the correlations between a set of variables, especially vitamin D and laboratory test results both for the first and the second subgroup; eGFR was not included in such correlations ( and ).
Table 3A. Correlations between vitamin D and laboratory test results (25-OH D levels <30 mg/mL – 57 observations)
Table 3B. Correlations between vitamin D and laboratory test results (25-OH D levels >30 mg/mL – 47 observations)
At baseline, in patients with 25-OH serum levels <30 ng/mL, vitamin D correlates directly with calcium, phosphorus, PTH, albumin, eGFR, and hemoglobin. The correlation between calcium and phosphorus is different in the two subgroups. Indeed, PTH and hemoglobin values increase dramatically in the second group (25-OH serum levels >30 ng/mL).
The different correlation between vitamin D and other variables strengthens the influence of the above-mentioned vitamin D threshold. Indeed, in patients with vitamin D insufficiency (<30 mg/mL), all the evaluated parameters show a different correlation when compared to patients with vitamin D normal status (>30 ng/mL).
Probit model was estimated throughout the whole sample and results can be observed in . An inverse relationship exists between levels of vitamin D after 12 months of administration and the probability that adverse events occur.
Table 4. Estimation results (probit model)
However, as the estimated coefficients cannot be easily interpreted as simply being the values that maximize the likelihood function, while the marginal effects are easier to interpret, they have been computed and can be observed in .
Table 5. Marginal effects
The estimated probability that more than one event may occur in the observed sample is 13.20%. High blood pressure shows a positive relationship (although estimated marginal effect is not significant) with the dependent variable. On the contrary, a negative relationship is associated to BMI (when BMI decreases there is an increased probability that more than one event occurs).
Vitamin D has been shown to reduce the probability of cardiovascular and renal events. Indeed, vitamin D intake for more than 12 months can reduce the probability of such events by 11.42%. Each co-morbid factor, instead, increases by 29%Footnote1 the probability of such events to occur.
Table 6. Estimation results for the first subgroup (probit model)
Table 7. Marginal effects for the first subgroup
DISCUSSION
The results of this prospective cohort study suggest that vitamin D deficiency is associated with increased cardiovascular risk and that vitamin D supplementation significantly reduces the incidence of developing any of the above-mentioned events.
Moreover, our data show that increased cardiovascular risk is present at 25-OH D levels (<30 ng/mL) at least compatible with vitamin D insufficiency and that such risk is reduced with vitamin D supplementation. The choice to evaluate the cut-off value of 30 ng/mL comes from medical literature which estimates the value of 30 ng/mL or greater as the optimal level for a better health outcome.Citation10
The reason why vitamin D, whose action to regulate mineral homeostasis, may be responsible for other functions, such as the cardiovascular system, is debated. A possible explanation of this effect is related to the ubiquitous presence of vitamin D receptor.Citation12 Moreover, it acts on the cardiovascular system and inhibits arteries' calcification, both by stimulating the production of proteins that are inhibitors of arterial calcificationCitation13 and by inhibiting the production of cytokines that are involved in calcification.Citation14
CKD is typically associated with vitamin D insufficiency or deficiency.Citation15 In a study, it was observed that 25-OH D values were at the lower limit of normal in the majority of patients with CKD.Citation16 Lower vitamin D levels were observed in patients with proteinuria as well as in those with secondary hyperparathyroidism and, in the course of CKD, 25-OH D values were <30 mg/mL.
The association between oral calcitriol use and survival was shown in a cohort of 1418 patients with CKD (stages 3–4). The authors found, after a follow-up of 1.9 years, a 26% lower risk for death and a 20% lower risk for death or dialysis after adjustment for several factors including co-morbidities, renal status, and parameters of mineral metabolism such as PTH, calcium, and phosphorus levels.Citation17 Similar findings were reported by Kovesdy et al. in a male outpatient population with CKD stages 3–5: treatment with low doses of oral vitamin D was associated with significantly better survival and this effect was independent from pretreatment PTH, calcium, and phosphorus levels.Citation18 Moreover, patients treated with vitamin D had more co-morbidities characterized by older age, lower diastolic blood pressure, higher PTH, lower creatinine clearance, and increased serum phosphorus levels; furthermore, mortality rates were lower when compared to patients without oral vitamin D treatment.
A recent meta-analysis on vitamin D compounds in people with CKD showed that vitamin D compounds do not reduce the risk for death and the beneficial effects on cardiovascular outcomes in people with CKD are unproven.Citation19
Another point of interest in our study was the relation between baseline 25-OH D levels and clinical events. Patients were divided into groups according to 25-OH D levels. We used 25-OH D levels instead of 1,25-OH D, because although the latter is the most biologically active hormonal form of vitamin D, serum 25-OH D is considered to be the best indicator of vitamin D status: it is the substrate for the renal and non-renal production of 1,25-OH D, it has a longer biological half-life than 1,25-OH D, and it circulates in much higher concentrations.Citation20 Moreover, serum 25-OH D reflects the total production of vitamin D from both endogenous and exogenous sources, including exposure to ultraviolet-B radiation and intake of various dietary forms, such as fortified foods and fish. Our findings regarding the role of vitamin D level as a predictor for future cardiovascular events have already been shown in previous studies both in patients on dialysis and in patients with CKD. Activated vitamin D deficiency was found to be associated with higher all-cause and cardiovascular mortality in a large cohort of hemodialysis patients,Citation9 whereas increased coronary calcification was associated with lower 1,25-dihydroxyvitamin D3 levels,Citation21 also suggesting a direct link between vitamin D levels and survival, which may be independent from PTH involvement.
In a study on 168 incident outpatients, with stages 2–5 CKD, plasma 25-OH D was shown to be an independent inverse predictor of the disease.Citation22 Patients' median age was 70 years, 26% were diabetic patients, and 58% presented with previous cardiovascular events. The first follow-up was carried out after 2 years and then patients were followed up for 6 years. The same effect was confirmed by a multivariate analysis as well.
Of great interest is the optimal serum 25-OH D level. According to several authors, the optimal level of 25-OH D has been suggested to be 30 ng/mL or even higher.Citation10
However, approximately 41% of men and 53% of women from the Third National Health and Nutrition Examination Survey (NHANES III) had a serum level below 28 ng/mL.Citation23 Moreover, NHANES III data showed in a cross-sectional study an important association between hypovitaminosis D and mortality (26% increased rate of all-cause mortality), especially for the lowest quartile of 25-OH D level (<17.8 ng/mL).Citation24 The same results were found in patients with CKD from the NHANES III: a statistically significant, negative effect on survival was found in patients with levels <15 ng/mL, whereas it was not found in those with levels between 15 and 30 ng/mL.Citation25
CONCLUSIONS
During the past years, several studies have been performed supporting the assumption that vitamin D can play a major role in the general population as well as in chronic disease.Citation9 In patients with renal disease, vitamin 25-OH D is lower, and its level does not seem to depend on the severity of CKD, but, on the contrary, it seems to be associated with proteinuria, even in non-nephrotic range.Citation13 However, reduced activity of 1-alpha-hydroxylase in any stage of CKD may induce hypovitaminosis D, when compared to another patient with the same 25-OH D deficiency, but with normal renal function and consequently with normal 1-alpha-hydroxylase enzyme levels.
Moreover, vitamin 25-OH D levels are not modified by adequate intake levels of vitamin D and do not appear to influence, according to some studies, the degree of secondary hyperparathyroidism.Citation13 Finally, patients depleted of 25-OH D die before non-depleted ones.14–15
Although there is not a clear association between vitamin D serum levels and CKD, we observed that vitamin D deficiency can play a major role in increasing mortality in patients with renal disease.
Up to now, we are not able to demonstrate that the tendency toward increased mortality can be reversed by vitamin D precursors treatment. We need, therefore, to carry out a study that provides, regardless of PTH levels, a correction of vitamin 25-OH D above 30 mg/mL and we also need to observe its influence on survival. Later, it will be interesting to observe whether this effect has a direct action or it is mediated by 25-OH D multiple effects on the different organ systems.
Acknowledgment
We thank Prof. Maria Amalia Santoro for the English revision of the manuscript.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Notes
1The same model has been estimated again for the first subgroup, considering the main co-morbid factors ( and ): what should be remarked is the positive correlation with the vitamin D level and the probability of events. The level of vitamin D is too low to act as a preventive factor.
REFERENCES
- Holick MF. High prevalence of vitamin D inadequacy and implications for health. Mayo Clin Proc. 2006;81:353–373.
- Nesby-O'Dell S, Scanlon KS, Cogswell ME, Hypovitaminosis D prevalence and determinants among African American and white women of reproductive age: Third National Health and Nutrition Examination Survey, 1988–1994. Am J Clin Nutr. 2002;76:187–192.
- Lind L, Hanni A, Lithell H, Hvarfner A, Sorensen OH, Ljunghall S. Vitamin D is related to blood pressure and other cardiovascular risk factors in middle-aged men. Am J Hypertens. 1995;8:894–901.
- Hyppönen E, Laara E, Reunanen A, Jarvelin MR, Virtanen SM. Intake of vitamin D and risk of type 1 diabetes: A birth-cohort study. Lancet. 2001;358:1500–1503.
- Chiu KC, Chu A, Go VL, Saad MF. Hypovitaminosis D is associated with insulin resistance and β cell dysfunction. Am J Clin Nutr. 2004;79:820–825.
- Krause R, Buhring M, Hopfenmuller W, Holick MF, Sharma AM. Ultraviolet B and blood pressure. Lancet. 1998; 352:709–710.
- Gorham ED, Garland CF, Garland FC, Vitamin D and prevention of colorectal cancer. J Steroid Biochem Mol Biol. 2005;97:179–194.
- Ponsonby AL, McMichael A, van der Mei I. Ultraviolet radiation and autoimmune disease: Insights from epidemiological research. Toxicology. 2002;181–182:71–78.
- Wolf M, Shah A, Gutierrez O, Vitamin D levels and early mortality among incident hemodialysis patients. Kidney Int. 2007;72(8):1004–1013.
- Bischoff-Ferrari HA, Giovannucci E, Willett WC, Dietrich T, Dawson-Hughes B. Estimation of optimal serum concentrations of 25-hydroxyvitamin D for multiple health outcomes. Am J Clin Nutr. 2006;84(1):18–28.
- National Kidney Foundation. K/DOQI clinical practice guidelines for bone metabolism and disease in chronic kidney disease. Am J Kidney Dis. 2003;42:S1–S201.
- De Luca HF. Overview of general physiologic features and functions of vitamin D. Am J Clin Nutr. 2004;80(Suppl.): 1689S–1696S.
- Bellows CG, Reimers SM, Heersche JN. Expression of mRNAs for type-I collagen, bone sialoprotein, osteocalcin, and osteopontin at different stages of osteoblastic differentiation and their regulation by 1,25 dihydroxyvitamin D3. Cell Tissue Res. 1999;297(2):249–259.
- Panichi V, De PS, Andreini B, Calcitriol modulates in vivo and in vitro cytokine production: A role for intracellular calcium. Kidney Int. 1998;54(5):1463–1469.
- LaClair RE, Hellman RN, Karp SL, Prevalence of calcidiol deficiency in CKD: A cross-sectional study across latitudes in the United States. Am J Kidney Dis. 2005;45: 1026–1033.
- Gonzalez EA, Sachdeva A, Oliver DA, Martin KJ. Vitamin D insufficiency and deficiency in chronic kidney disease: A single center observational study. Am J Nephrol. 2004; 24:503–510.
- Shoben AB, Rudser KD, de Boer IH, Young B, Kestenbaum B. Association of oral calcitriol with improved survival in nondialyzed CKD. J Am Soc Nephrol. 2008;19(8):1613–1619.
- Kovesdy CP, Ahmadzadeh S, Anderson JE, Kalantar-Zadeh K. Association of activated vitamin D treatment and mortality in chronic kidney disease. Arch Intern Med. 2008;168(4):397–403.
- Palmer SC, McGregor DO, Craig JC, Elder G, Macaskill P, Strippoli GF. Vitamin D compounds for people with chronic kidney disease not requiring dialysis. Cochrane Database Syst Rev. 2009;(4):CD008175.
- Cantorna MT, Zhu Y, Froicu M, Wittke A. Vitamin D status, 1,25-dihydroxyvitamin D3, and the immune system. Am J Clin Nutr. 2004;80(Suppl.):1717S–1720S.
- Watson KE, Abrolat ML, Malone LL, Active serum vitamin D levels are inversely correlated with coronary calcification. Circulation. 1997;96(6):1755–1760.
- Ravani P, Malberti F, Tripepi G, Vitamin D levels and patient outcome in chronic kidney disease. Kidney Int. 2009;75(1):88–95.
- Zadshir A, Tareen N, Pan D, Norris K, Martins D. The prevalence of hypovitaminosis D among US adults: Data from the NHANES III. Ethn Dis. 2005;15(4 Suppl. 5):S5-97–S5-101.
- Melamed ML, Michos ED, Post W, Astor B. 25-hydroxyvitamin D levels and the risk of mortality in the general population. Arch Intern Med. 2008 Aug 11;168(15):1629–1637.
- Mehrotra R, Kermah DA, Salusky IB, Chronic kidney disease, hypovitaminosis D, and mortality in the United States. Kidney Int. 2009;76(9):977–983.