Abstract
We studied paraphenylenediamine (PPD)-related acute kidney injury (AKI) in 81 patients and also in albino rats experimentally. In the patients’ group AKI was found in 32.7%. Of them, 81.4% needed dialysis support. The overall mortality was 25.9%. In experimental rats the renal lesions were noted in all and they were glomerular congestion, intertubular (interstitial) hemorrhages, acute tubular necrosis, mesangial proliferation, and intratubular casts. The severity of renal injury appears to be dose dependent.
INTRODUCTION
Hair dye and its constituent paraphenylenediamine (PPD) have been reported as accidental and intentional causes of poisoning from developing countries such as Africa, Middle East Asia, and Indian subcontinent.Citation1 PPD is a derivative of paranitroaniline, which is widely used as an oxidizable hair dye, in dyeing furs, in photochemical, and in tyre-vulcanizing industries. PPD is commonly mixed with henna (leaves of Lawsonia alba), which is traditionally applied to color palms, soles, and feet, and to dye hair to a dark red shade.Citation2 PPD is a good hydrogen donor and is metabolized by electron oxidation to an active radical by cytochrome P450 peroxidase to form a reactive Benzoquinone diamine. This is further oxidized to form a trimer known as Brandowaski’s base, a compound that is an allergen, mutagenic, and highly toxic.Citation3
Acute poisoning accidental or intentional by ingestion of PPD causes severe edema of face and neck, frequently requiring emergency tracheostomy. This is followed by rhabdomyolysis and acute kidney injury (AKI) culminating in death if not treated aggressively. This hair dye poisoning is gaining public health importance in view of its easy availability and as an important cause of intentional harm in the developing world.
Majority of the studies on PPD poisoning were clinical with a mention on some details of the histology from postmortem and antemortem studies. As a result the information on evolution and severity of the renal histopathological injury was sparse.
Keeping this in view, we studied separately the clinical and experimental aspects in patients and in albino rats, respectively.
Our aims were to study (1) the AKI management and outcome of hospitalized patients for systemic PPD intoxication and (2) experimentally the PPD-related AKI in rats.
SUBJECTS AND METHODS
Our study comprised two groups: (1) clinical group and (2) experimental group.
Clinical Group
During the period of January 2007 to August 2011, 81 patients of AKI following hair dye ingestion who were admitted to Sri Venkateswara Institute of Medical Sciences, Tirupati, were studied. The following were analyzed: (1) demographic profile, (2) clinical profile, (3) morbidity and mortality pattern, and (4) management and the outcome.
Experimental Group
Most of the studies of PPD-related AKI were clinical and the renal histopathology reported in these studies was variable. Experimental data were sparse. In order to study the renal histopathology in detail, the experimental group was taken up.
This study was conducted from July 2010 to August 2010, in the Department of Biochemistry, Sri Venkateswara University, Tirupati. The animals were maintained in accordance with NIH guidelines for care and use of laboratory animals and experiment protocol was approved by the Institutional Animal Ethics Committee, Sri Venkateswara University. Eighteen Wistar albino male rats weighing 210–250 g were taken for this study. The animals were housed in cages provided with rice husk as bedding material under ambient temperature of 21 ± 3°C. The animals were acclimatized to the laboratory conditions for 1 week at the commencement of treatment protocol. The animals were randomly divided into six groups (control and five test groups) each comprising three rats. On the basis of the route of administration of the hair dye containing PPD, the test groups of rats were divided into two batches as follows:
Batch I (Groups 1–3)—PPD administered orally and
Batch II (Groups 4 and 5)—PPD administered intraperitoneally.
The toxicity was tested at different doses of the PPD. The lethal oral dose of PPD for rats was determined as 80 mg/kg body weightCitation4 and lethal intraperitoneal dose was determined as 37 mg/kg body weight.Citation5 Hence, we tested the toxicity of PPD at lethal and various sublethal doses through different routes. The treatment protocol was as follows:
Batch-I
Group 1: Received PPD at a dose of 80 mg/kg b.w. as single dose and were killed after 3 h.
Group 2: Received PPD at a dose of 40 mg/kg b.w. as single dose and were killed after 3 days.
Group 3: Received PPD at a dose of 20 mg/kg b.w. as single dose and were killed after 6 days.
Batch-II
Group 4: Received PPD at a dose of 37 mg/kg b.w. as single dose and were killed after 3 h.
Group 5: Received PPD at a dose of 18 mg/kg b.w. as single dose and were killed after 3 days.
Control group of animals received placebo.
Immediately after killing of the animals, the kidneys were collected in 4% formalin and were studied for histopathological abnormalities.
STATISTICAL ANALYSIS
Student’s t-test was applied to continuous variables and chi-square test was applied to categorical variables. p-Value ≤0.01 was considered significant.
RESULTS
The results of clinical and experimental groups are discussed separately.
Clinical Group
During a period of 4.5 years, 247 patients of hair dye poisoning were treated in our institute. Of them, AKI was detected in 81 patients (32.7%). The demographic and clinical profiles of the patients of AKI were tabulated ().
Table 1. Distribution of patients of AKI according to age and sex.
Table 2. Distribution according to clinical features in patients of AKI requiring and not requiring RRT.
Table 3. Showing the differences of parameters between the two groups of AKI.
Experimental Group
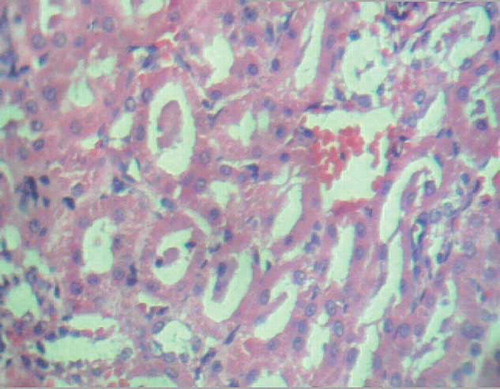
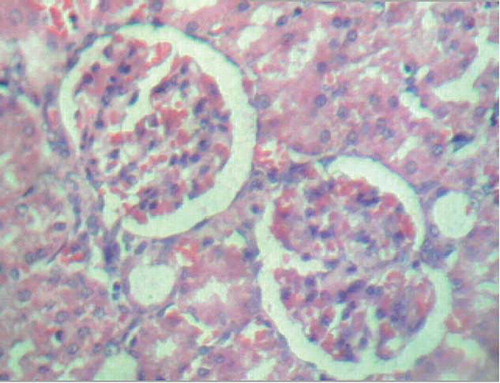
Histopathological examination of experimental group was presented in .
Table 4. Histopathological examination of experimental group.
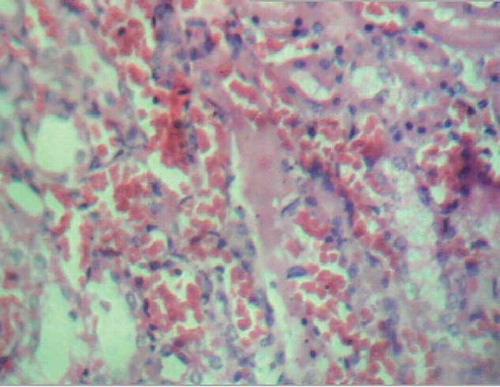
Figure 1. Severe glomerular congestion, mild glomerular edema, and mild intertubular hemorrhage (H&E staining, ×280).
DISCUSSION
In literature review, it is stated that hair dye poisoning is emerging as an important public health problem in the developing world as a cause of intentional or accidental poisoning. PPD, a derivative of paranitroaniline, when ingested, in a dose-dependent manner, results in severe cervico-facial inflammatory edema, rhabdomyolysis, renal failure, and cardiac toxicity.Citation1,3,6–9 Rhabdomyolysis is explained by the leakage of calcium ions from the smooth endoplasmic reticulum, which results in prolonged muscle contraction and irreversible changes in muscle structure.Citation1,10,11 Elevated levels of creatine phosphokinase in plasma are found due to rhabdomyolysis. AKI is explained through the mechanisms of direct toxic effect, hemoglobinuria, myoglobinuria, hypovolemia, and hypotension. Lipid peroxidation was considered as a mechanism of cellular injury. The described renal histology changes were variable: normal histology, acute tubular necrosis, and acute interstitial nephritis.Citation3,7,11,12 Mortality is mainly attributed to acute respiratory distress, myocarditis, cardiac arrhythmias, and shock.Citation7,9 AKI predicts poor prognosis. There is no specific antidote for PPD and treatment is mainly supportive,Citation3,10,11 which includes gastric lavage, intravenous fluids, vasopressors, correction of metabolic acidosis, and respiratory and dialysis supports. Though the toxin is not dialyzable dialysis helps in the overall management in the presence of AKI. Hemodialysis (HD) is found to be superior to peritoneal dialysis in some of the studies.Citation3
In our study, we found cervicofacial edema in 50 (61.7%) patients, dysphagia in 43 (53%) patients, chocolate brown urine in 41 (50.6%) patients, pain and/or rigidity of swollen limbs in 30 (37%) patients, and ventilatory requirement in 37 (45.6%) patients. The findings were comparable with other studies.Citation3,9
In our study, AKI was observed in 81 (32.7%) patients. It was predominantly oligoanuric in type in 76.5%. Of the total 81patients, 66 (81.4%) patients needed dialysis supports and 45 (68.2%) of them became dialysis independent and were discharged. Twenty-one (31.8%) died among patients who required dialysis. All patients recovered among the group that did not require dialysis. The type of dialysis support received by patients was intermittent hemodialysis (IHD) using biocompatible polysulfone membrane with bicarbonate dialysate. The reported incidence of renal failure is variable at 25.8–60% in various studies.Citation3,11 In the reported literature mortality varied between 22.5% and 31.6%.Citation3,7,9 We observed systolic and diastolic blood pressures (BPs) were more in patients of RRT group compared with non-RRT group and it was statistically significant [p-value 0.008 for systolic blood pressure (SBP) and 0.01 for diastolic blood pressure (DBP)]. We also observed statistically significant relationship between serum creatinine at presentation and duration of hospitalization (by Karl Pearson’s correlation coefficient p-value 0.001).
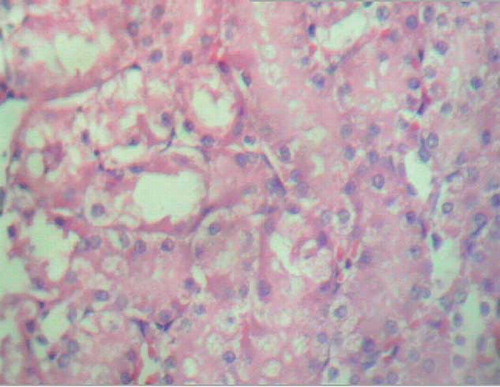
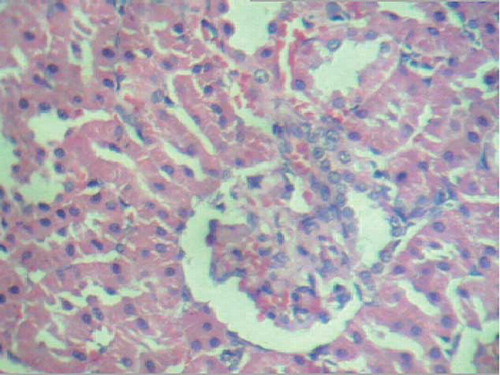
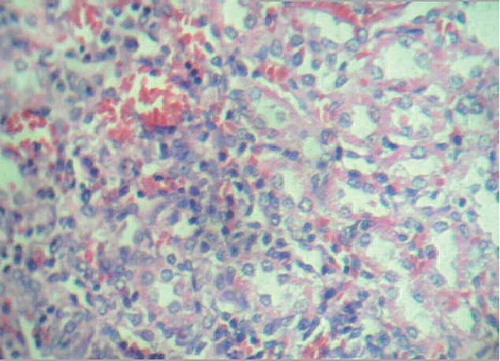
In our study, the renal histology was studied experimentally in rats. In rats the lesions of renal injury observed were glomerular congestion, intertubular (interstitial) hemorrhages, acute tubular necrosis, mesangial proliferation, and intratubular casts.
We observed more severe renal injury in the oral and intraperitoneal lethal dose groups in comparison to sublethal and minimal dose groups suggesting the severity of injury is dose related. We found regenerative changes in oral sublethal, oral minimal, and intraperitoneal sublethal dose groups suggesting the time-related effect.
Our study highlights the following: (1) clinical and experimental correlation in PPD-related AKI, (2) renal injury is dose dependent and there is evidence for recovery with time, and (3) suggestion to envisage the possibility of new experimental model for toxin-mediated AKI.
CONCLUSION
Hair dye poisoning, accidental or intentional, is becoming an important cause of AKI in developing countries. Presence of AKI testifies to the severity of intoxication and predicts poor prognosis. Our study confirms the observations in the clinical and experimental groups. Through our study, we reiterate the importance of public awareness regarding the potential lethality of this compound, need of display of toxicity warnings on hair dye labels, and control measures to prevent over-the-counter sale.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
REFERENCES
- Anugrah C, Anisa B, Anand Z. Hair dye poisoning – An emerging problem in the tropics: An experience from a tertiary care hospital in South India. Trop Doct. 2010;40:100–103.
- Ashar A. Acute angioedema in paraphenylenediamine poisoning. JPMA. 2003;53:3.
- Jain PK, Agarwal N, Kumar P, Sengar NS, Agarwal N, Akhtar A. Hair dye poisoning in Bundelkhand region (Prospective analysis of hair dye poisoning cases presented in Department of Medicine, MLB Medical College, Jhansi). JAPI. 2011;59:415–419.
- European Commission Health & Consumer Protection Directorate-General. Opinion on p-phenylenediamine, Scientific Committee on Consumer Products. SCCP/0989/06.
- Material Safety Data Sheet, para Phenylenediamine. Available at: http://www.ScienceLab.com. Accessed October 2005.
- Filali A, Semlali L, Ottaviano V, . A retrospective study of acute systemic poisoning of paraphenylene diamine in Morocco. African J. 2006;3:142–149.
- Sahay M, Vani R, Vali S. Hair dye ingestion – An uncommon cause of acute kidney injury. JAPI. 2009;57:743–744.
- Verma R, Tewari N, Jaiswal S, Rastogi V, Singh DK, Tiwari A. Fatal poisoning caused by oral ingestion of a hair dye. Internet J Emerg Intensive Care Med 2008;11(1). Available at: http://www.ispub.com/journal/the_internet_journal_of_emergency_and_intensive_care_medicine/volume_11_number_1_2/article/fatal_ poisoning_caused_by_oral_ingestion_of_a_hair_dye.html. Accessed March 2, 2010.
- Kallel H, Chelly H, Dammak H, . Clinical manifestations of systemic paraphenylene diamine intoxication. J Nephrol. 2005;18:308–311.
- Soni SS, Nagarik AP, Dinaker M, Adikey GK, Raman A. Systemic toxicity of paraphenylenediamine. Indian J Med Sci. 2009;63(4):164–166.
- Salma MS, Mirghani F, Mohamed EN. Poisoning with hair dye containing paraphenylene diamine: Ten years experience. Saudi J Kidney Dis Transpl. 1995;6(3):286–289.
- Ram R, Swarnalatha G, Prasad N, Dakshinamurty KV. Paraphenylene diamine ingestion: An uncommon cause of acute kidney injury. J Post Grad Med. 2007;53:181–182.