Abstract
There has never been a home hemodialysis (HHD) program or self-care hemodialysis (SC-HD) program in Mainland China, and it may be plausible starting from an SC-HD program. This study describes the systems for, and the initial results of, starting an SC-HD program. A program for SC-HD was instituted at the Peking University Third Hospital. A working group had designed the patient education program and water quality assurance. The patient’s education program was established, which consisted of a handbook and a video for training. In May 2009, two patients were recruited and trained for HD. They were adequately dialyzed with satisfactory Kt/V, both the patients could perform all of the self-care procedures after training for 12 weeks. More difficult procedures, such as the self-cannulation, were successfully handled. Significant improvement was found in six of the eight short form (SF)-36 health scales after 6 months for SC-HD treatment. For the past year, there were no severe complications resulting from SC-HD. In summary, our first SC-HD program in Mainland China is feasible and safe. It promotes rehabilitation, increases self-esteem, and improves health-related quality of life. It is also a first attempt for starting an HHD program.
INTRODUCTION
Patients suffering from end-stage renal disease (ESRD) require dialysis to support their lives. Dialysis can be in the form of either hemodialysis (HD) or peritoneal dialysis. In China, there are around 290,000 ESRD patients on dialysis according to 2011 China Dialysis RegistryCitation1; 90% (250,000 patients) of them are on in-center HD and 10% (29,000 patients) of them are on peritoneal dialysis. Cost analysis from some data showed that continuous ambulatory peritoneal dialysis is the more economic form of dialysis therapy.Citation2 On the other hand, self-care HD (SC-HD) with less attending medical and nursing staffs very likely may provide an alternative mode of dialysis therapy to the ESRD patients.Citation3 Moreover, studies have shown that self-care patients have greater potential for rehabilitation, independence, and a better quality of life (QOL).Citation4,5,6 Home HD (HHD) has been used only in a minority of patients in past years around the world, although it may offer significant advantages over other renal replacement therapies. There has never been a HHD program or SC-HD program in Mainland China, and it may be plausible starting from an SC-HD program. This study aims to investigate the feasibility of the first SC-HD program in our hospital.
PATIENTS AND METHODS
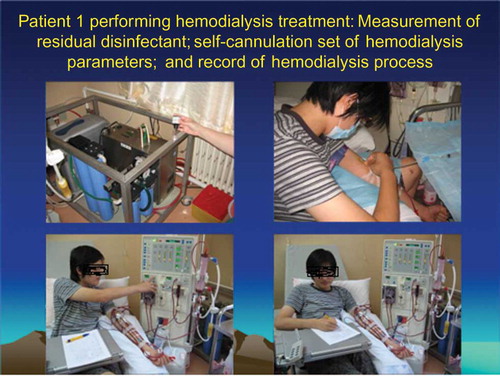
Two patients were enrolled in this study. Written informed consent was obtained from both the patients. The Peking University Ethics Committee approved this study protocol. A working group (including nephrologists, nurses, technicians, and patients; see ) designed the patient education program and water quality assurance. The patient’s education program was established, which consisted of a handbook and a video for training. The patients were trained for SC-HD procedures that included weighing, blood pressure, pulse and temperature checking, trolley preparation, priming of dialyzers, postpriming testing, testing for residual disinfectant, bloodline and dialyzer setting up, conductivity setting, heparin dosage and heparin syringe setting up, ultrafiltration volume adjustment, and stop bleeding over venipuncture site by compression after HD. Both the patients used the Fresenius 2008 B hemodialysis machines (Fresenius Medical Care, Bad Homburg, Germany). Patient 1 was a university student. He is an incident HD patient and he chose two times a week, and 5 h per session. Patient 2 is a housewife. She had done in-center HD for 2 years, and she chose three times a week, and 6 h per session. SC-HD treatment surplus (including HD machine, tube and dialyzers, dialysis concentrates, and water treatment machine) were donated by Fresenius Medical Care (Shanghai) Co., Ltd. (Shanghai, China) Patients’ blood flow was set at 200 mL/min and dialysate flow was set at 500 mL/min. Before performing in-center SC-HD, the registered nurse and the patient care technicians would teach and assist patients in becoming competent on how to perform dialysis. After the patients had mastered their skills, they would perform the skill on their own, and because they were in a dialysis center there will always be nurses and patient care technicians nearby. The health care professionals will always be there to support them by answering their questions and lend a helping hand if they need one. All finished procedures were checked. Training and supervision took about 12 weeks. Then, every patient had continued to do SC-HD for 1 year.
Short Form 36 Questionnaires
The short form (SF)-36 questionnaires were the main tool to assess the QOL in dialysis patients.Citation4,5 The SF-36 was finally evaluated in eight domains: physical functioning (PF, 10 items), role-physical (RP, 4 items), body pain (BP, 2 items), general health (GH, 5 items), role-emotional (RE, 3 items), social functioning (SF, 2 items), vitality (VT, 4 items), and mental health (MH, 5 items). The score for each domain ranges from 0 to 100, and dialysis patients with the higher scores indicate better QOL.
RESULTS
Both the patients were adequately dialyzed with satisfactory Kt/V ( and ) and could achieve the standard of interdialytic weight gain of less than 1 kg/day. Moreover, our patients’ anemia status and blood pressure control have been improved and patient 2 had stopped to some prescription drug use (such as erythropoietin and antihypertensive medication) after 6 months of the SC-HD.
Table 1. The parameters for baseline and follow-up of the patient 1 treated with SC-HD.
Table 2. The parameters for baseline and follow-up of the patient 2 treated with SC-HD.
Both the patients could perform all of the self-care procedures (see and ) after training for 12 weeks. More difficult procedures such as the heparin dosage preparation, adjustment of ultrafiltration volume, and self-cannulation were successfully handled. Significant improvement was found in six of the eight SF-36 health scale after 6 months for SC-HD treatment such as PF, RP, GH, RE, VT, and MH (see ). For the past year, there was no severe complication resulting from the SC-HD treatment in our study (see ) and only minor mistakes were made or suffering from mild complications in a total of 240 person-time SC-HD treatment.
Table 3. Patients’ performances in SC-HD procedures (n = 2).
Table 4. Comparison of SF-36 scores in two patients between baseline and follow-up.
Table 5. Summary of complications for a total of 240 person-time SC-HD treatment.
DISCUSSION
HHD, once a valid, viable dialysis choice, faded as facility-based care was preferentially funded and supported by the 1970s and 1980s.Citation7 The renaissance of HHD began in Canada when home-based nocturnal dialysis emerged in the 1990s.Citation8 Home patients soon appreciated the self-determination and reemployment opportunities that overnight dialysis delivered, the now-expanding potential of home and nocturnal HD in regions as diverse as North America,Citation8 Australia and New Zealand,Citation7 Japan,Citation9 the United Kingdom,Citation7 and Finland.Citation10 On the other hand, HHD program developed recently might result from SC-HD serving as an important “platform” for which the HHD program was built later.Citation10
With the economic development and social and medical insurance support in China, there have been an increasing number of ESRD patients on dialysis. Nowadays, patients are mainly recruited to the dialysis program of the public hospitals irrespective of age and comorbid conditions and the majority (90%) of patients are on in-center HD, whereas only 10% of patients are on peritoneal dialysis. HD is the first renal replacement therapy because it is the most mature mode of dialysis and it is an effective form of treatment. However, hospital in-center HD is expensive and should be reserved for acute and chronically ill patients. HHD is the cheapest mode of dialysis in Western countries.Citation2 However, there has never been an HHD program in Mainland China. First, it is because of the expensive HD machine and reverse osmosis unit hindering the development of the HHD program; second, there has been no policy about medical management and insurance coverage in HHD. But in fact, patients may need diversified dialysis modalities. So, it may be a good attempt starting from SC-HD in hospital as the first step of HHD program.
Our study was the first SC-HD program because all of the HD patients in China received full nursing support during HD treatment in a hospital. Our results showed that this is a full self-care program because our patients could do all of the procedures including self-cannulation of fistula, rinse-back and dismantling of the dialyzer, and bloodline at the end of HD. Both the patients had the courage to cannulate themselves. But, we thought that if more patients were included, some patients might not have courage to do self-cannulation of fistula. Other Western country people might have the same problem.Citation3 Our results verified that intelligence did not appear to be a major obstacle in learning, where motivation and the learning environment were more important. In particular, our patients’ health-related QOLs have been improved in SF-36 questionnaire such as PF, RP, GH, RE, VT, and MH. This means that SC-HD promotes rehabilitation and improves health-related QOL. Moreover, our patients’ dialysis adequacy, anemia status, and blood pressure control have been improved, whereas some prescription drug uses (such as erythropoietin and antihypertensive medication) have been reduced or even stopped.
The cost of running a dialysis unit depends on a large number of factors, which include staff salaries, drugs, consumables, operating cost, and overhead. However, the major factor is the staff cost. By reducing the number of attending staff in a self-care model, the cost of running a dialysis unit can be decreased. An economic study was performed by the Goeree’s group.Citation2 But our current study cannot calculate the staff cost of SC-HD with only two patients recruited because of our space limitation.
We have demonstrated that SC-HD is safe and without severe complications except that patients made minor mistakes or suffered from mild complications (such as occasional loss of minor blood and failure of self-cannulation) in a total of 240 person–time SC-HD treatment.
In summary, our first SC-HD program in Mainland China is feasible and safe. It promotes rehabilitation and improves health-related QOL. It is also the first step of an HHD program. But there has been no policy for medical management and health insurance reimbursement in SC-HD or HHD in Mainland China.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
This study was supported by National Natural Science Foundation (Grant No. 81170706).
REFERENCES
- China Dialysis Registry data. 2011.
- Goeree R, Manalich J, Grootendorst P, Beecroft ML, Churchill DN. Cost analysis of dialysis treatments for end-stage renal disease (ESRD). Clin Invest Med. 1995;18(6):455–464.
- Wauters JP, Hunziker A, Brunner HR. Regionalized self-care hemodialysis: a solution to the increasing cost. JAMA. 1983;27(1):59–62.
- Evans RW, Manninen DL, Garrison LP Jr. The quality of life of patients with end-stage renal disease. N Engl J Med. 1985; 312:553–559.
- Bremer BA, McCauley CR, Wrona RM. Quality of life in end stage renal disease: a reexamination. Am J Kidney Dis. 1989; 13:200–209.
- Meers C, Singer MA, Toffelmire EB, Self-delivery of hemodialysis care: a therapy in itself. Am J Kidney Dis. 1996;27(6):677–700.
- Agar JW. International variations and trends in home hemodialysis. Adv Chronic Kidney Dis. 2009;16(3):205–214
- Komenda P, Copland M, Er L, Djurdjev O, Levin A. Outcomes of a provincial home hemodialysis programme—a two-year experience: establishing benchmarks for programme evaluation. Nephrol Dial Transplant. 2008;23:2647–2652.
- Kobin T. Practice of home hemodialysis in dialysis clinic. Contrib Nephrol. 2012;177:143–150.
- Honkanen EO, Rauta VM. What happened in Finland to increase home hemodialysis? Hemodial Int. 2008;12:S11–S15.