Abstract
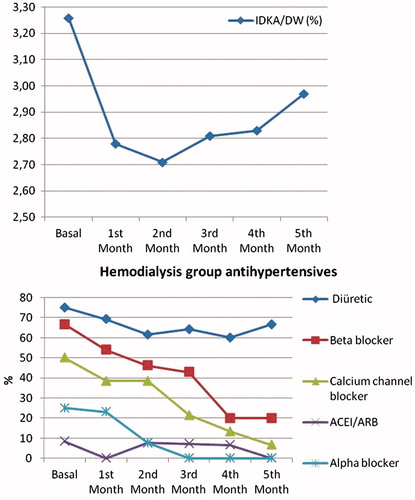
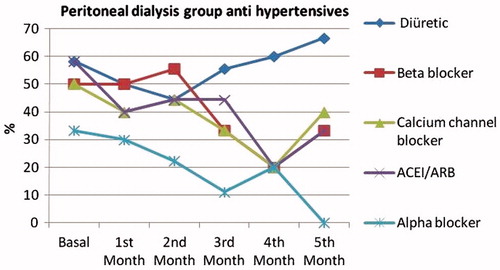
Introduction: Overhydration is the main contributory factor of left ventricular hypertrophy and closely associated with cardiovascular events in end stage renal disease (ESRD) patients. The aim of this prospective-study was to investigate the impact of strict salt and volume control on hypertension and cardiac condition in ESRD patients. Methods: A total of 12 peritoneal dialysis (PD) and 15 prevalent hemodialysis (HD) patients were enrolled. All patients either PD or HD were allocated to intervention of strict salt restriction according to basal hydration state of empty abdomen in PD and midweek predialysis HD which were estimated by body composition monitor (BCM) and echocardiography. Results: Mean ages were 48.3 ± 16.7 years for PD, and 48.8 ± 18 for HD patients. Extracellular water/height was 10.04 ± 2.70 and 10.39 ± 1.53 L/m in PD and HD groups. Systolic blood pressures decreased in PD and HD from 133.1 ± 28 and 147.3 ± 28.5 to 114.8 ± 16.5 and 119.3 ± 12.1 mmHg, respectively, (p < 0.00). IDKA/DW were decreased from 3.26 ± 1.6 to 2.97 ± 1.63 % in HD group (p > 0.05). LVMI and LAI were not increased in both groups. Conclusion: Strict salt and volume control in ESRD patients after assessment of hydration status with either using BCM or echocardiography provides better management of volume control leading to more precise cardiovascular protection.
Introduction
Reduced capacity to excrete excess water by the kidneys in end-stage renal disease (ESRD) may cause volume overload and increase in the patient weight.Citation1 Overhydration is complicated by hypertension and left ventricular hypertrophy (LVH). The hemodynamic overload is characterized by an enlargement of the left ventricular cavity.Citation2,Citation3 A strict volume control strategy decreases blood pressure without anti hypertensive medication and consequently leads the regression of LVH.Citation4,Citation5 Increasing left ventricular mass is related to worsening of cardiovascular condition in peritoneal dialysis (PD) patients.Citation6 Currently, determining fluid overload is measured by body composition monitor (BCM) which is non-invasive and practical tool used in hemodialysis (HD) and PD patients.Citation7 Determining the real dry weight is necessary for minimizing interdialytic weight gain and reduction of volume overload with ultrafiltration achieved by strict salt control.Citation1
Methods
All patients either PD or HD were allocated to intervention of strict salt restriction according to basal hydration state of empty abdomen in PD and midweek predialysis HD which were estimated by body composition monitor (BCM) and echocardiography.
Study outcomes
Study was performed prospectively for 5 months, primary outcomes were prevention of progression of left ventricular mass index (LVMI) and left atrium index (LAI), secondary outcomes were frequency of anti hypertensive drug usage and interdialytic weight gain/dry weight (IDKA/DW) decrease during the follow-up.
Patient selection
A total of 12 PD and 15 prevalent HD patients were enrolled from the same institution. Patients were recruited among patients on maintenance HD and PD treated in the Departments of Nephrology Bulent Ecevit University in Zonguldak. Patients who were willing to participate in the study with written informed consent, older than 18-years and on maintenance bicarbonate HD scheduled thrice weekly (12 h/week) with a Kt/V of at least 1.2 were included among HD patients. Exclusion criteria for HD and PD groups were the presence of pacemaker or defibrillator, artificial joints, pin or amputation, permanent or temporary catheters, being scheduled for living donor renal transplantation, presence of serious life-limiting co-morbid situations (e.g. malignancy), uncontrollable infection, end-stage cardiac, pulmonary, or hepatic disease, pregnancy or lactating. The study was conducted in accordance with ethical principles of the Declaration of Helsinki and in compliance with the Good Clinical Practice Guidelines.
Echocardiography
All patients underwent echocardiographic evaluation at baseline and at the end of 5th month on a midweek interdialytic day for HD group and with empty abdomen for PD group with a GE Vingmed Vivid Five Echocardiography Device (GE Medical System, Hortan, Norway). The echocardiograms were read one independent cardiologist. Measurements included assessment of left atrial volume, left ventricular systolic and diastolic functions and left ventricular mass, LVM.Citation8 LVMI was calculated by the equation described by Devereux and ReichekCitation9 and indexed for body surface area.Citation10
Bioimpedance analysis
Fluid overload was measured using BCM-Body Composition Monitor (Fresenius Medical Care, Deutschland GmbH, Bad Homburg, Germany), which is increasingly used technique for determining fluid overload and body composition in HD and PD patients. The measurements were performed before the scheduled dialysis session, after the short interdialytic interval, in a supine position for HD and with empty abdomen for PD patients. The extracellular water (ECW), intracellular water (ICW) and total body water (TBW) were determined by the BCM using the electrical principles described previously.Citation11
Laboratory measurements
In both groups, laboratory parameters were measured monthly using standard automated techniques (Architect C 8000 auto-analyzer and Axsyme third generation immunoassay system, Abbott, IL). Blood samples were obtained under fasting conditions in PD and immediately before the scheduled dialysis sessions for HD patients.
Statistical considerations
Statistical analyses were performed using SPSS, version 13 (Chicago, IL). All parameters were expressed as mean ± standard deviation. Intra-group comparisons were performed with a paired t-test or Wilcoxon signed ranks test if the data was not normally distributed. Intergroup comparisons between two groups were assessed by independent sample t test. p Value < 0.05 was considered as statistically significant. Differences in proportion on repeated evaluations were compared using the McNemar’s tests.
Results
Mean ages were 48.3 ± 16.7 for PD, and 48.8 ± 18 years for HD patients. Baseline characteristics, hydration status in case of clinical and echocardiography parameters were similar in two groups. Extracellular water/height was 10.04 ± 2.70 and 10.39 ± 1.53 L/m in PD and HD groups. Systolic blood pressures decreased in PD and HD from 133.1 ± 28 and 147.3 ± 28.5 to 114.8 ± 16.5 and 119.3 ± 12.1 mmHg respectively (p < 0.00). Frequency of diuretic drugs increased in PD (), beta blockers and calcium channel blocker drugs decreased in HD group significantly (). The usage of erythrocyte stimulating agent at baseline and at the end of the study 33.3% and 26.7% for HD, 33% and 25% in PD groups (p > 0.005). IDKA/DW were decreased from 3.26 ± 1.6% to 2.97 ± 1.63% in HD group (p > 0.05). LVMI and LAI were not increased in both groups (). Both serum albumin and hemoglobin levels were not changed in both groups during intervention period. Laboratory results were not different baseline and were not changed finally in both PD and HD groups ().
Table 1. Hydration status.
Table 2. Laboratory results.
Discussion
Hypervolemia is a devastating problem in ESRD patients. Decreased residual renal functions in PD and HD patients especially have prone to hypervolemia. This situation usually evident in patients who could not be successful in salt restriction and having inadequate dialysis treatment. Edema, hypertension and uncontrolled interdialytic weight gain may be seen as major signs of hypervolemia. Increase of the cardiothoracic index should be noticed in telecardiography. Detection of hypervolemia by using either echocardiography or especially BCM has been getting popularity.Citation12 Hypervolemia is an important cardiovascular risk factor and ultrafiltration treatment in PD and HD patients is mandatory. Diuretics may be useful for the correction of hypervolemia especially in PD patients if residual renal functions preserved. In HD patients for achieving the dry weight accompanied by normotension needs appropriate ultrafiltration. Euvolemia is an important issue for HD patients and it has been previously shown that the strict salt control normalizes blood pressure and increases the life expectancy. Strict salt control has an important effect on volume overload and on LV dysfunction.Citation13 Hur et al. showed that hypervolemia appears to be widely prevalent in PD patients and fluid overload had a major effect on both blood pressure and LVH. For the detection of hypervolemia BCM was shown as a useful tool for defining overhydration with regard to echocardiography.Citation12,Citation14 Ozkahya et al. investigated the effect of salt restriction and volume control on blood pressure and they found that decreased LVMI accompanied by saline control.Citation15 Present study has shown that a strict volume control lead the decrease of blood pressure and the improvement in cardiac parameters in PD and HD patients by preventing LVH progression. Kayikcioglu et al. showed that fluid overload of dialysis patients leads to hypertension and increased left ventricular mass index.Citation16 Present study was shown a decrease of IDKA/DW in HD group but the difference couldn’t reach the statistical significance and decreasing the blood pressures also decreasing the need of anti hypertensive drugs indicating the successful salt and volume control both HD and PD groups. At the end of the study, final echocardiographic measurements revealed that there were not increase in LVMI and LAI in both PD and HD groups. More recently Hur et al. conducted a prospective randomized controlled study using strict volume control strategy with the help of bioimpedance measurements. They showed LVMI reduction of 12% after a 12 months follow-up period.Citation14 Asci et al. was achieved the regression of LVH in PD patients with salt restriction and strict volume control methods.Citation13 In the present study we prevented the progression of LVH both in PD and HD groups. This may be due to short follow up period of the study.
We have shown a reduction of extracellular fluid volume in HD and PD patients achieved by salt and volume control and decreased the use of antihypertensive drugs in a relatively short follow up period. Strict salt control in ESRD patients after assessment of hydration status with either using BCM or echocardiography provides better management of volume control leading to more precise cardiovascular protection.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article.
References
- Stegmayr BG. Ultrafiltration and dry weight – what are the cardiovascular effects? Artif Organs. 2003;27:227–229
- Meeus F, Kourilsky O, Guerin AP, et al. Pathophysiology of cardiovascular disease in hemodialysis patients. Kidney Int Suppl. 2000;76:140–147
- Crepaldi C, Soni S, Chionh CY, et al. Application of body composition monitoring to peritoneal dialysis patients. Contrib Nephrol. 2009;163:1–6
- Ozkahya M, Ok E, Cirit M, et al. Regression of left ventricular hypertrophy in hemodialysis patients by ultrafiltration and reduced salt intake without antihypertensive drugs. Nephrol Dial Transplant. 1998;13:1489–1493
- Charra B, Chazot C. Volume control, blood pressure and cardiovascular function. Lessons from hemodialysis treatment. Nephron Physiol. 2003;93:94–101
- Wang X, Axelsson J, Lindholm B, et al. Volume status and blood pressure in continuous ambulatory peritoneal dialysis patients. Blood Purif. 2005;23:373–378
- Moissl UM, Wabel P, Chamney PW, et al. Body fluid volume determination via body composition spectroscopy in health and disease. Physiol Meas. 2006;27:921–933
- Lang RM, Bierig M, Devereux RB, et al.; Chamber Quantification Writing Group; American Society of Echocardiography's Guidelines and Standards Committee; European Association of Echocardiography. Recommendations for chamber quantification: a report from the American Society of Echocardiography's Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005;18:1440–1463
- Devereux RB, Reichek N. Echocardiographic determination of left ventricular mass in man: anatomic validation of method. Circulation. 1978;58:1072–1083
- Paoletti E, Bellino D, Casottana P, et al. Left ventricular hypertrophy in nondiabetic predialysis CKD. Am J Kidney Dis. 2005;46:320–327
- Moissl UM, Wabel P, Chamney PW, et al. Body fluid volume determination via body composition spectroscopy in health and disease. Physiol Meas. 2006;27:921–933
- Hur E, Gungor O, Musayev O, et al. Bioimpedance spectroscopy for the detection of hypervolemia in peritoneal dialysis patients. Adv Peritoneal Dial. 2011;27:1–6
- Asci G, Ozkahya M, Duman S, et al. Volume control associated with better cardiac function in longterm peritoneal dialysis patients. Perit Dial Int. 2006;26:85–88
- Hur E, Usta M, Toz H, et al. Effect of fluid management guided by bioimpedance spectroscopy on cardiovascular parameters in hemodialysis patients: a randomized controlled trial. Am J Kidney Dis. 2013;61:957–965
- Ozkahya M, Toz H, Ozerkan F, et al. Impact of volume control on left ventricular hypertrophy in dialysis patients. J Nephrol. 2002;15:655–660
- Kayikcioglu M, Tumuklu M, Ozkahya M, et al. The benefit of salt restriction in the treatment of end-stage renal disease by hemodialysis. Nephrol Dial Transplant. 2009;24:956–962