Abstract
Introduction and objective: Contrast-induced nephropathy (CIN) significantly increases the morbidity and mortality of patients. The aim of this study is to investigate and compare the protective effects of isotonic sodium chloride with sodium bicarbonate infusion and isotonic sodium chloride infusion with diltiazem, a calcium channel blocker, in preventing CIN. Materials and methods: Our study included patients who were administered 30–60 mL of iodinated contrast agent for percutaneous coronary angiography (PCAG), all with creatinine values between 1.1 and 3.1 mg/dL. Patients were divided into three groups and each group had 20 patients. The first group of patients was administered isotonic sodium chloride; the second group was administered a solution that of 5% dextrose and sodium bicarbonate, while the third group was administered isotonic sodium chloride before and after the contrast injection. The third group received an additional injection of diltiazem the day before and first 2 days after the contrast injection. All of the patients’ plasma blood urea nitrogen (BUN) and creatinine levels were measured on the second and seventh day after the administration of intravenous contrast material. Results: The basal creatinine levels were similar for all three groups (p > 0.05). Among a total of 60 patients included in the study, 16 patients developed acute renal failure (ARF) on the second day after contrast material was injected (26.6%). The number of patients who developed ARF on the second day after the injection in the first group was five (25%), in the second group was six (30%) and the third group was five (25%) (p > 0.05). Conclusion: There was no significant difference between isotonic sodium chloride, sodium bicarbonate and isotonic sodium chloride with diltiazem application in prevention of CIN.
Introduction
Contrast-induced nephropathy (CIN) is defined as development of acute renal failure (ARF) following the use of intravascular contrast medium when all other possible causes of renal failure have been ruled out.Citation1 The most common symptom of CIN is observed 48–72 h after exposure to the contrast medium, when there is a 25% or 0.5 mg/dL (44 micromol /L) increase in the level of basal serum creatinine.Citation2
The incidence of CIN varies depending on the presence or absence of risk factors, physical and chemical properties of the contrast agent used, volume and usage of protective measures such as hydration prior to the procedure. In patients with no significant risk factor, the incidence of CIN was around 3–5%, while in patients with risk factors it could rise to 100%.Citation3–5 CIN is the third leading cause of hospital-acquired ARF.Citation1
The risk factors of CIN are the following: pre-existing renal insufficiency, diabetes mellitus, advanced age, advanced stage congestive heart failure, hypovolemia, anemia, symptomatic hypotension, hypertension, acute myocardial infarction, peripheral vascular disease, high-dose use of contrast material and the use of nephrotoxic drugs.Citation6–9
Currently, there is no specific cure for CIN. Isotonic sodium chloride, sodium bicarbonate, N-acetyl cysteine, furosemide, mannitol, calcium channel blockers except diltiazem, prostaglandin E1, adenosine antagonist, ascorbic acid, l-arginine, fenoldopam, dopamine, statin endothelin receptor antagonists, atrial natriuretic peptide are among many methods that have been used and investigated for prevention of CIN.Citation9–13
In the current literature, there are no studies investigating the effect of the combination therapy of diltiazem and isotonic sodium chloride in the prevention of nephropathy in high-risk patients undergoing percutaneous coronary angiography (PCAG). For this reason, the aim of our study was to investigate and compare the preventive effects of isotonic sodium chloride, sodium bicarbonate and isotonic sodium chloride with diltiazem applications on CIN development in patients who had to receive contrast agent, despite the borderline high serum creatinine values (1.1–3.1 mg/dL). There are many studies focusing of prevention of CIN development. However, to our knowledge, there has not been a study comparing these three methods at the same time.
Materials and methods
Our study included patients who were administered 30–60 mL of iodinated contrast agent for PCAG, with serum creatinine values between 1.1 and 3.1 mg/dL (normal range: adult female: 0.66–1.09 mg/dL, male: <50 years: 0.84–1.25 mg/dL, and >50 y: 0.81–1.44 mg/dL. Intravenously injected contrast agent was 30–60 mL low-osmolar nonionic monomer iohexol (Omnipaque 300 mg– 50-ml vial, Opakim Medical Products Ltd. Co., Istanbul). Sixty patients were equally divided into three groups.
Patients with the following conditions were excluded from the study: serum creatinine values outside the specified range, previously diagnosed multiple myeloma, distinctive heart failure, uncontrolled hypertension (systolic > 160 mmHg, diastolic > 100 mmHg), patients who received the contrast agent within the last 3 days, known allergic reaction to the contrast agent, received N-acetyl cysteine, dopamine or mannitol during the month prior to the study and pregnant women. The patients using β-blockers were excluded from the group that received diltiazem.
The study was designed as a single-center, prospective study. We recorded patients’ age, concomitant diseases and current medications. Prior to the procedure, serum metabolic panel, complete blood count, complete urine analysis and urine microprotein and creatinine levels were simultaneously measured. Patients’ creatinine clearance was calculated by the MDRD formula.
[GFR = 186 × (Scrr)−1.154 × (age)−0.203 × (0.742 if female)].Citation14 The presence of echocardiographic left ventricular ejection fraction, valve pathology or wall motion abnormality was investigated.
The first group received 3 mL/kg isotonic sodium chloride for 1 h prior to the injection of iohexol. All patients received iohexol injection for the purpose of PCAG in the first and second hours after the start of infusion. After the iohexol injection, patients were administered a 1 mL/kg/h dose isotonic sodium chloride for 6 h.
The second group of patients received 850 mL of 5% dextrose solution with 150 mEq sodium bicarbonate (10 ml 8.4% molar sodium bicarbonate, Biosel Pharmaceutical Industry, Istanbul) at a dose of 3 mL/kg for 1 h before injection of iohexol. The iohexol was administered to all patients for the purpose of PCAG between the first and second hours after the start of infusion. After the iohexol injection, 1 mL/kg/h of sodium bicarbonate solution was administered for 6 h.
As in the first group, the patients in the third group received 3 mL/kg dose of isotonic sodium chloride for the duration of 1 h before administration of iohexol. After the start of infusion, iohexol was injected between the first and second hours for the purpose of PCAG. After the procedure, 1 mL/kg/h dose of isotonic sodium chloride was given for 6 h. In addition, patients in this group also received diltiazem 2 × 60 mg orally, one day prior to the iohexol injection and for two days after the injection (at 10:00 and at 22:00). Heart rate of patients was follow up for the complication of bradycardia. The amount of contrast agent used was similar in all three groups. On the second and seventh day after the intravenous injection of contrast material, plasma blood urea nitrogen (BUN) and creatinine levels were measured in all patients.
Statistical analysis
Statistical Package for the Social Sciences, version 9.0 (SPSS Inc., Chicago, IL) was used for statistical analysis. The quantitative data was defined as the mean and standard deviation. In variables that were analyzed for normality, the “One-way ANOVA” test was done to compare the groups. The “Scheffe” procedure was used to determine which group was different. The "Repeated Analysis of Variance" was used for the comparison of values between the basal levels and other times and the "Bonferroni" test was used to determine which time was different. The distribution in qualitative data was expressed as a percentage. The “chi-square” (χ2) test of statistical significance was used for suitable data. A p value of 0.05 was considered significant.
Results
The study included a total of 60 patients: 33 men (55%) and 27 women. Mean age was 62.65 ± 11.04 (range: 29–80 years). The basal creatinine levels were determined as 1.44 ± 0.33 mg/dL (1.1–3.1 mg/dL). Basal mean creatinine clearance was 48.44 ± 14.45 mL/min (23.70–94.00 mL/min). Each group consisted of 20 patients. The first group included 13 men (21.7%) and 7 women (11.7%), the second group had 9 men (15%), 11 women (18.3%), and the third group had 11 men (18.3%) and 9 women (15%). The mean age in the first group was 60.8 ± 12 (29–75), in the second group 62.7 ± 10.5 years (range 42–80) and in the third group was 62.6 ± 11.8 (29–80) years. There was no significant difference between the groups in terms of serum albumin levels. In addition, all groups had similar basal electrolyte values. Moreover, basal urine microprotein/creatinine ratio and hemoglobin values were similar in all three groups. The number of smoking patients was also similar. The ejection fraction values measured echocardiographically were similar in all groups. Bradycardia was not seen in diltiazem group.
There were eight diabetic patients in the first group (13.3%), four in the second group (6.7%) and nine in the third group was (15%). There was no statistically significant difference between the groups in terms of patients with diabetes. The number of hypertensive patients in the first group was 12 (20%), in the second group 11 (18.3%) and in the third group 13 (21.7%). The demographic characteristics of patients are shown in . Medications, except for the β-blockers, were similar between the groups. None of the patients in the third group were taking β-blockers.
Table 1. Demographic characteristics, creatinine clearances and basal plasma creatinine levels of patients.
The basal creatinine level in the first group was 1.37 ± 0.21 mg/dL baseline (1.2–2), in the second group 1.39 ± 0.16 mg/dL (1.2–1.9), and in the third group 1.56 ± 0.49 mg/dL (1.2–3.1) (p > 0.05). Patients’ creatinine clearance and basal creatinine levels before the contrast agent injection are shown in .
In all patient groups, the number of patients who developed ARF two days after the administration of contrast agent was 16 (26.6%). The number of patients who developed ARF 2 days after the administration of contrast agent in the first group that received isotonic sodium chloride was five (25%), in the second group that received sodium bicarbonate was six (30%) and in the third group that was treated with diltiazem and isotonic sodium chloride was five (25%) (p > 0.05).
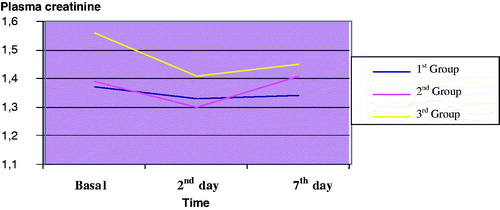
Seven days after the injection of contrast agent, the total number of patients who developed ARF increased to 17. Thus, on the seventh day, the observed incidence of ARF was 28.3%. Seven days after the administration of contrast agent, the number of patients who developed ARF was five (25%) in the isotonic sodium chloride group, six (30%) in sodium bicarbonate group and six (30%) in the group treated with isotonic sodium chloride and diltiazem (p > 0.05). The difference in the number of patients with ARF in the isotonic sodium chloride group was not significant. Patients’ plasma creatinine levels before and after the contrast agent injections are shown in .
Table 2. Plasma creatinine levels before and after the contrast injection.
The change in the plasma creatinine levels in patients after the injection of contrast agent is depicted in .
Discussion
CIN is a problem that is frequently encountered in clinical practice. In recent years, as a result of the increasing use of contrast agents in diagnostic and interventional radiological procedures, CIN has become the third leading common cause of hospital-acquired ARF. CIN significantly increases the length of hospital stay, morbidity and mortality.Citation8 Therefore, it is important to manage the patients with CIN and to take preventive measures for CIN, especially in patients with high risks.
In our study, from a total of 60 patients, 16 developed ARF on the second day after the injection of contrast agent and one patient developed ARF on the seventh day.
There are many studies related to the prevention of contrast nephropathy available in the literature. The studies not only underline the value of hydration, but also showed that adequate hydration may reduce the incidence of contrast agent-induced renal failure.Citation15 Taylor et al. showed that 1000 mL of oral fluid intake 12 h before the intravenous contrast injection and intravenous fluid injection at a rate of 100–150 mL/h 12 h after injection significantly reduced the development of CIN.Citation16 In another study, Mueller et al. had given isotonic sodium chloride and 0.45% sodium chloride to 1620 patients undergoing PCAG. They reported that 0.6% of patients administered isotonic sodium chloride and 2.7% of those administered 0.45% sodium chloride developed CIN (p = 0.002).Citation17 The data obtained up to this day confirms the idea that the volume expansion method is the most important method for reducing the risk of CIN.Citation13,Citation18
Merten et al., in a study of 119 patients with renal failure, administered sodium bicarbonate before and after injection of contrast agent to the first group of patients, while to the second group they gave sodium chloride. The incidence of CIN in the group that received sodium bicarbonate was 1.7%, while in the group that received sodium chloride it was 13.6%.Citation19 In another study, Hogan et al. evaluated the effectiveness of sodium bicarbonate-based hydration with saline-based hydration for the prevention of CIN. They reported that sodium bicarbonate-based hydration is more effective than saline-based hydration in terms of preventing CIN.Citation20 Several other studies also reported that sodium bicarbonate-based hydration is superior to saline solution in preventing CIN.Citation20–22 In our study, we did not observe a significant difference between saline infusion and bicarbonate infusion, which may be because of the small number of patients in our study.
The role of calcium channel blockers in preventing CIN has been investigated by using experimental animal models and clinical studies. The protective effects of calcium channel blockers on the kidney are provided by a variety of mechanisms. They have an effect of tubuloglomerular feedback and on tubular transport. In addition, calcium channel blockers inhibit the increase of intracellular calcium. They also reduce the formation of free radicals. Moreover, they maintain renal hemodynamics by providing a feedback mechanism for intrarenal vasoconstriction.Citation18,Citation23–25 Khoury et al. carried out a randomized study with 85 patients, where they compared administration of isotonic sodium chloride solution alone with isotonic sodium chloride + nifedipine prior to injection of contrast agent. As a result, they did not find a statistically significant difference between the two groups.Citation26 In a different study, by Russo et al., 30 patients were given sublingual nifedipine prior to injection of contrast agent while another group received placebo. In the group that was given a placebo there was a decrease in renal plasma flow and GFR, while in the group that received nifedipine there was an increase in renal plasma flow and GFR. Patients in this study did not receive isotonic sodium chloride.Citation27 Another study was done with 27 patients, in which two groups received either oral felodipine or placebo before contrast injection was compared. All of the patients received at least 2000 mL/24 h fluid the day before and the day after the injection of the contrast agent. In the group that was administered felodipine, there was an increase in the plasma creatinine levels after the injection of contrast agent compared to basal levels, while in the group that received placebo there was no increase.Citation28 In yet another study, 90 patients undergoing coronary angiography were divided into two groups. The first group received hydration along with amlodipine/valsartan, while the second group received hydration alone. In this article, it was reported that 17.8% patients from the first group and 6.7% patients from the second group developed CIN.Citation18
As can be seen from above cited literature, studies on the effectiveness of calcium channel blockers in the prevention of CIN are contradictory.
In our study, we compared the effects of isotonic sodium chloride, sodium bicarbonate and isotonic sodium chloride infusion along with a calcium channel blocker, diltiazem on prevention of CIN.
In our study, basal plasma creatinine levels in the first group were 1.37 ± 0.21 mg/dL, on the second day this value was 1.33 ± 0.49 mg/dL and on the seventh day it was 1.34 ± 0.30 mg/dL. In the second group, the basal plasma creatinine values were 1.39 ± 0.16 mg/dL, values on the second day and on the seventh day were 1.30 ± 0.20 mg/dL and 1.41 ± 0.35 mg/dL, respectively. In the third group, the basal plasma creatinine levels, creatinine levels on the second day and on the seventh day were as followings: 1.56 ± 0.49 mg/dL, 1.41 ± 0.40 mg/dL and 1.45 ± 0.50 mg/dL, respectively.
Among 60 patients who received the contrast agent, 16 developed ARF on the second day after the injection of contrast agent (26.6%). The number of patients who developed ARF on the second day post-contrast injection in the first group was five (25%), in the second group it was six (30%) and in the third group it was five (25%) (p > 0.05). Although the incidence of ARF at the end of the second day was higher in the second group, this difference was not significant when compare to the other groups. On the seventh day, one more patient developed ARF (1.66%). On the seventh day, the number of patients with ARF in the first group was five (25%), in the second group was six (30%), and the third group was six (30%) (p > 0.05). Although, the first group the incidence of ARF at the end of the seventh day was lower compared to the other groups, this difference was not significant.
There might be several explanations as to why in the group that was given diltiazem, a calcium channel blocker, the number of patients who developed CIN was higher than in the group that was given isotonic sodium chloride alone. The important determining factors may include administration of a sufficient dose and the appropriate time and duration of administration. However, there is no standardized dose and timing of administration for diltiazem with an indication to prevent CIN. Diltiazem is indicated for lowering blood pressure, which also may have an effect on renal perfusion, therefore, masking the renal protective effect of diltiazem.Citation29
As a result of this study, we determined that hydration with isotonic sodium chloride alone was more effective application in the prevention of CIN compared to hydration with sodium bicarbonate or isotonic sodium chloride with diltiazem. However, this difference did not reach a level of statistical significance. Moreover, patients in the third group received isotonic sodium chloride, similar to the first group, but the third group also had diltiazem in addition to isotonic sodium chloride.
There was no significant difference between the groups in terms of prevention of CIN. Ultimately, we did not find a significant contribution for the calcium channel blocker diltiazem in the prevention of CIN.
The absence of significant differences between the groups in the prevention of CIN may be due to the small number of patients in our study. Further, more comprehensive and controlled studies are needed to provide a more specific opinion on this subject.
Limitations
The main limitation of our study is the relatively small sample size.
Declaration of interest
The authors declare no conflicts of interests. The authors alone are responsible for the content and writing of this article.
References
- Detrenis S, Meschi M, Musini S, Savazzi G. Lights and shadows on the pathogenesis of lights and shadows on the pathogenesis of contrast-induced nephropathy: state of the art. Nephrol Dial Transplant. 2005;20(8):1542–1550
- Thomsen HS, Morcos SK. Contrast media and the kidney: European society of urogenital radiology (ESUR) guidelines. Br J Radiol. 2003;76(908):513–518
- Rihal CS, Textor SC, Grill DE, et al. Incidence and prognostic importance of acute renal failure after percutaneous coronary intervention. Circulation. 2002;105(19):2259–2264
- Lufft V, Hoogestraat-Lufft L, Fels LM, et al. Angiography for renal artery stenosis: no additional impairment of renal function by angioplasty. Eur Radiol. 2002;12(4):804–809
- Erley CM, Duda SH, Rehfuss D, et al. Prevention of radiocontrast- media-induced nephropathy in patients with pre-axisting renal insufficiency by hydration in combination with the adenosine antagonit theophylline. Nephrol Dial Transplant. 1999;14:1146–1149
- Cavusoglu E, Chhabra S, Marmur JD, et al. The prevention of contrast-induced nephropathy in patients undergoing percutaneous coronary intervention. Prog Cardiovasc Dis. 2003;45(6):493–503
- Moos SI, Stoker J, Beenen LF, Flobbe K, Bipat S. The prevention of contrast-induced nephropathy in Dutch hospitals. Neth J Med. 2013;71(2):97–103
- Alessandri N, Lanzi L, Garante CM, et al. Prevention of acute renal failure post-contrast imaging in cardiology: a randomized study. Eur Rev Med Pharmacol Sci. 2013;17:13–21
- Okumura K, Sone T. Risk assessment and prevention of contrast-induced nephropathy in patients undergoing coronary angiography. Intern Med. 2012;51(6):519–521
- Dangas G, Iakovou I, Nikolsky E, et al. Contrast-induced nephropathy after percutaneous coronary interventions in relation to chronic kidney disease and hemodynamic variables. Am J Cardiol. 2005;95:13–19
- Solomon R, Werner C, Mann D, et al. Effects of saline, mannitol and furosemide on acute decreases in renal function induced by radiocontrast agents. New Eng J Med. 1994;331(21):1416–1420
- Weinstein JM, Heyman S, Brezis M. Potential deleterious effect of furosemide in radiocontrast nephropathy. Nephron. 1992;62:413–415
- Sudarsky D, Nikolsky E. Contrast-induced nephropathy in interventional cardiology. Int J Nephrol Renovasc Dis. 2011;4:85–99
- Baptista JP, Udy AA, Sousa E, et al. A comparison of estimates of glomerular filtration in critically ill patients with augmented renal clearance. Crit Care. 2011;15(3):R139 . doi:10.1186/cc10262
- Toprak O, Cirit M. Risk factors and therapy strategies for contrast-induced nephropathy. Ren Fail. 2006;28(5):365–381
- Taylor AJ, Hotchkiss D, Morse RW, et al. PREPARED: preparation for angiography in renal dysfunction: a randomized trial of in patient vs out patient hydration protocols for cardiac catheterization in mild-to-moderate renal dysfunction. Chest. 1998;114:1570–1574
- Mueller C, Buerkle G, Buettner HJ, et al. Prevention of contrast-media associated nephropathy: randomized comparison of 2 hydration regimens in 1620 patient undergoing coronary angioplasty. Arch Intern Med. 2002;162:329–336
- Oguzhan N, Cilan H, Sipahioglu M, et al. The lack of benefit of a combination of an angiotensin receptor blocker and calcium channel blocker on contrast-induced nephropathy in patients with chronic kidney disease. Ren Fail. 2013;35(4):434–439
- Merten GJ, Burgess WP, Gray LV, et al. Prevention of contrast-induced nephropathy with sodium bicarbonate: a randomized controlled trial. J Am Med Assoc. 2004;291(19):2328–2334
- Hogan SE, LAllier P, Chetcuti S, et al. Current role of sodium bicarbonate-based preprocedural hydration for the prevention of contrast-induced acute kidney injury: a meta-analysis. Am Heart J. 2008;156:414–421
- Meier P, Ko DT, Tamura A, Tamhane U, Gurm HS. Sodium bicarbonate-based hydration prevents contrastinduced nephropathy: a meta-analysis. BMC Med. 2009;13:7–23
- Jang JS, Jin HY, Seo JS, et al. Sodium bicarbonate therapy for the prevention of contrast-induced acute kidney injury – a systematic review and meta-analysis. Circ J. 2012;76(9):2255–2265
- Wang YX, Jia YF, Chen KM, Morcos SK. Radiographic contrast media induced nephropathy: experimental observations and the protective effect of calcium channel blockers. Br J Radiol. 2001;74(888):1103–1108
- Esnault VL. Radiocontrast media-induced nephrotoxicity in patients with renal failure: rationale for a new double-blind, prospective, randomized trial testing calcium channel antagonists. Nephrol Dial Transplant. 2002;17(8):1362–1364
- Duan SB, Liu FY, Luo JA, et al. Nephrotoxicity of high- and low-osmolar contrast media. The protective role of amlodipine in a rat model. Acta Radiol. 2000;41:503–507
- Khoury Z, Schlicht JR, Como J, et al. The effect of prophylactic nifedipine on renal function in patients administered contrast media. Pharmacotherapy. 1995;15(1):59–65
- Russo D, Testa A, Della Volpe L, et al. Randomised prospective study on renal effects of two different contrast media in humans: protective role of a calcium channel blocker. Nephron. 1990;55(3):254–257
- Spangberg-Viklund B, Berglund J, Nikonoff T, et al. Does prophylactic treatment with felodipine, a calcium antagonist, prevent low-osmolar contrast-induced renal dysfunction in hydrated diabetic and nondiabetic patients with normal or moderately reduced renalfunction?. Scand J Urol Nephrol. 1996;30(1):63–68
- Costanzi S, Danza F, Neri A, Passalacqua S, Fulignati P, Splendiani G. Use of felodipine to prevent radyokontrast nefropathy(RCN). J Am Soc Nephrol. 1994;5:s390–s394