Abstract
Aim: To assess the relationship between mesangial hypercellularity in various childhood nephropathies and clinical and laboratory parameters. Methods and patients: The reports of the renal biopsies were evaluated retrospectively. The patients with diagnosis of IgA nephropathy (isolated and Henoch–Schönlein nephritis), IgM nephropathy, or isolated mesangial proliferative glomerulonephritis were included. Each nephropathy group was divided into two subgroups according to the severity of mesangial hypercellularity as mild and severe. The biochemical data and histopathological findings of the patients were recorded. Results: When the groups were compared, it was found that the patients with IgA nephropathy had hematuria (p = 0.043) and the patients with IgM nephropathy had nephrotic syndrome more frequently than the other patients (p = 0.01). No difference was detected between the groups regarding the severity of mesangial hypercellularity. On the other hand, when the groups were evaluated within themselves, no significant association was detected between the severity of mesangial hypercellularity and clinical and laboratory parameters. It was determined that the renal biopsy was performed earlier in patients with Henoch–Schönlein nephritis compared to the other cases (p = 0.004). Compared to the isolated IgA nephropathy group, it was found that the number of cases with severe mesangial hypercellularity was higher and the level of proteinuria was more prominent in patients with Henoch–Schönlein nephritis. Additionally, when the patients with Henoch–Schönlein nephritis were evaluated, the degree of proteinuria was found to be higher in patients with severe mesangial hypercellularity compared to those of showing mild mesangial hypercellularity (p = 0.002). Conclusion: It was observed that there is no direct relation between the severity of mesangial hypercellularity and clinical and laboratory findings in various childhood nephropathies. However, when Henoch–Schönlein nephritis is compared with IgA nephropathy, it was found that the severity of mesangial hypercellularity was higher in cases with Henoch–Schönlein nephritis and the level of proteinuria was more prominent in those cases. However, no difference was detected in glomerular filtration rates and biochemical data with regard to the level of mesangial hypercellularity.
Introduction
The most common causes of nephropathies which can induce the mortality and morbidity in childhood are Immunoglobulin A (IgA) nephropathies (isolated IgA nephropathy and Henoch–Schönlein nephritis (HSN)), Immunoglobulin M (IgM) nephropathy and isolated mesangial proliferative glomerulonephritis (MsPGN).Citation1–3 Although increment of mesangial cell and matrix is a common characteristic finding in all groups, clinical, laboratory and pathological findings of those nephropathies may be completely different.Citation4,Citation5
Mesangial cell injury is observed in all acute and progressive glomerular diseases as a common histopathological feature, which ends up with cell proliferation.Citation4,Citation5 In this study, we aimed to investigate the effect of mesangial hypercellularity on the clinical and laboratory findings in the most common childhood nephropathies.
Materials and methods
Renal biopsy reports of the patients followed up in Dokuz Eylul University, Faculty of Medicine Department of Nephrology between 1993 and 2007 were evaluated retrospectively. The clinical information, laboratory findings, localization of biopsy, mesangial hypercellularity, severity of matrix increment, presence of immune deposits and pathological diagnosis of IgA nephropathy (both isolated IgA nephropathy and HSN), IgM nephropathy and MsPGN were recorded.
The indications for renal biopsy were persistent non-nephrotic non-postural proteinuria, steroid-resistant nephrotic syndrome, recurrent macroscopic or persistent microscopic hematuria. “Persistent non-nephrotic proteinuria” was interpreted as the presence of non-nephrotic range proteinuria (4–40 mg/kg/d) at least for six months. “Steroid-resistant nephrotic syndrome” was described as a continuation of proteinuria with urine dipstick despite high-dose of (2 mg/kg/g) steroid for two months. “Persistent microscopic hematuria” was described as an observation of more than five red blood cells in each areas of urine microscopy at least 40 × for a period of six months. Glomerular filtration rate (GFR), was calculated by using the Schwartz formula. Since all blood pressure values of all cases were appropriate for their age limits, they were not addressed as a separate parameter.
Renal biopsies were performed percutaneously by pediatric nephrologists using tru-cut biopsy needle with a guidance of ultrasonography. Biopsy specimens of all patients were evaluated at the Department of Pathology, Dokuz Eylul University School of Medicine. Kidney tissues that were prepared as 3-micron-meter sections were evaluated by the light microscopy with hematoxylin–eosin, periodic acid-Schiff, Masson's trichrome, methenamine silver stains. “Mesangial hypercellularity” was defined as presence of more than three mesangial cells in the mesangial field.Citation6 Immunofluorescence examination was performed using antibodies specific for human IgG, IgA, IgM, C3, C1q, fibrinogen and albumin.
All the patients with mesangial proliferation were included in this study, while the patients with crescents, sclerosis and endoproliferation in pathology reports were excluded. Patients were defined as IgA nephropathy, IgM nephropathy and MsPGN according to the renal biopsy findings of light microscopy and immunofluorescence microscopy. The diagnosis of IgA nephropathy and IgM nephropathy were described according to the increment of mesangial cells and matrix accumulation accompanied by the presence of IgA and IgM dominancy.Citation6 The diagnosis of isolated MsPGN was described according to the increment of mesangial cells and matrix accumulation accompanied by the absence of any accumulation of immunoglobulins.Citation6 On the other hand, all groups were separated into two sub-groups according to the severity of mesangial hypercellularity as “mild” (four to six mesangial cells in a mesangial field) and “severe” (more than six mesangial cell in a mesangial field).Citation6
The distribution of patient gender, blood urea nitrogen (BUN) at the admission, serum creatinine and albumin levels, glomerular filtration rate (GFR), proteinuria values (in 24-h urine), and the presence of macroscopic or microscopic hematuria and prognosis (the presence or absence of attack in follow-up) were compared between different glomerulonephritis groups and between subgroups in each group. Since HSN is a systemic disease and has similar pathological findings with IgA nephropathy, it was compared with an isolated IgA nephropathy and own subgroups.
Statistical analysis
Data analysis was performed using SPSS Windows Version 11.0 statistical package program (SPSS Inc., Chicago, IL). The distribution between the groups was normal. A one-way ANOVA test was performed for the parametric values and the Kruskal–Wallis test was performed for non-parametric values in clinical and laboratory between the groups of isolated IgA nephropathy, IgM nephropathy, isolated MsPGN and HSN. Mann–Whitney U-test was used for the parametric comparison of the subgroups (mild and severe) according to the mesangial hypercellularity. The Chi-square test was used for non-parametric comparison of the subgroups. The value of p < 0.05 was considered significant.
Results
Clinical and laboratory characteristics of patients
Reports of 81 patients (17 isolated IgA nephropathy, 19 IgM nephropathy, 27 isolated MsPGN, and 18 HSN) from a total of 160 renal biopsy reports were selected for the study. Six of 81 patients (two isolated IgA nephropathy, two IgM nephropathy, one HSN and one isolated MsPGN) were excluded for insufficient data. Thus, a total of 75 patients (17 IgM nephropathy, 26 isolated MsPGN, 15 IgA nephropathy and 17 HSN) were included into the study. Clinical and laboratory findings of the groups are summarized in . The duration between diagnosis and biopsy was significantly different between the groups (p: 0.004) and this difference was caused by the HSN group.
Table 1. Clinical and laboratory characteristics of patients with different types of glomerulonephritis.
The clinical situation at the application
It was observed that nephrotic syndrome was more frequent in patients with isolated MsPGN than the other cases at first admission (p: 0.010). There was no significant difference compared to other groups (). On the other hand, there was no significant difference in clinical findings at first admission between the subgroups when evaluated as mild or severe mesangial hypercellularity.
Table 2. Clinical findings at first admission in patients with different types of glomerulonephritis.
Comparison of clinical and laboratory findings of isolated IgA nephropathy and HSN group
Proteinuria
There was no significant difference in proteinuria between the three groups (p: 0.199). However, the amount of proteinuria in the HSN group was significantly higher than that of the isolated IgA nephropathy group (p = 0.013) ().
Table 3. Comparison of clinical and laboratory data of patients with isolated IgA nephropathy and HSN.
Hematuria
The number of patients with hematuria in the isolated IgA nephropathy group was significantly higher as compared to other groups at first admission (p: 0.043) (). There was no significant difference in the number of patients with hematuria between the isolated IgA nephropathy and the HSN groups (p > 0.05) ().
Comparison of subgroups
There was no significant difference in the parameters except hematuria between the subgroups of isolated IgA nephropathy, IgM nephropathy or isolated MsPGN with showing a mild mesangial hypercellularity (isolated IgA nephropathy had more hematuria, p = 0.035). Additionally, there was no significant difference in the studied parameters between the subgroups of each nephropathy group with showing severe mesangial hypercellularity (p > 0.05) ().
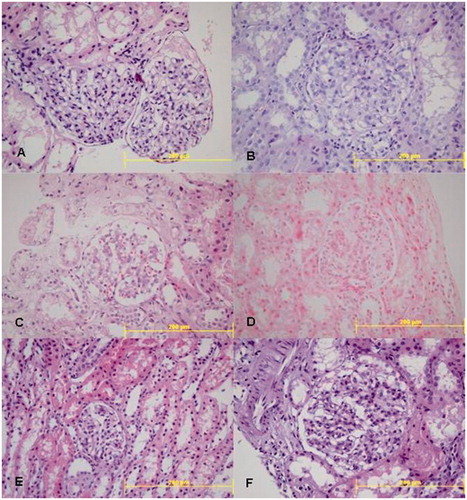
Figure 1. (A) Mild; (B) severe mesangial hypercellularity in IgA nephropathy; (C) mild; (D) severe mesangial hypercellularity in IgM nephropathy; (E) mild; (F) severe mesangial hypercellularity in isolated MsPGN.
In the HSN group, proteinuria levels were significantly higher in patients with severe mesangial hypercellularity than those with mild mesangial hypercellularity (p: 0.002). However, there was no significant difference between the subgroups regarding the clinical and laboratory findings in the isolated IgA nephropathy group (p > 0.05).
Histopathological findings
There was no significant difference in the severity of mesangial hypercellularity in cases with isolated IgA nephropathy, IgM nephropathy and isolated MsPGN (p: 0.159) ().
Discussion
In our study, the effect of mesangial hypercellularity severity on clinical and laboratory findings was investigated in the childhood nephropathies. Clinicopathologic findings were compared among themselves and with each other.
The duration between diagnosis and biopsy was significantly different between the groups and this difference was caused by the HSN group. The reason of short time between the age of biopsy and the age of diagnosis might be secondary to the presence of clinically skin rashes and additional renal involvement (hematuria and/or proteinuria).
Patients with isolated IgA nephropathy can present with different clinic. In the study of Nozawa et al. with 181 patients, they found isolated hematuria in 46% of cases, hematuria and proteinuria in 42.6% of cases.Citation7 Hematuria which is the characteristic of the isolated IgA nephropathy was found in 93% of our cases and it was consistent with the literature. The observation rate of isolated hematuria in the isolated IgA nephropathy group was significantly higher between the other groups. The patients with isolated IgA nephropathy initially have hematuria; however, it should not be forgotten that these patients might develop proteinuria in the future. Thus, the effect of these parameters on the biopsy results may be different. In our clinic, because we performed the biopsy in patients with persistent microscopic hematuria for six months, the hematuria rate was significantly higher than the other groups.
The patients with IgM nephropathy can present with macroscopic hematuria, asymptomatic microscopic hematuria–proteinuria, nephrotic syndrome and nephritic–nephrotic syndrome and more proteinuria.Citation8–11 In three different studies which include both children and adults, the nephrotic syndrome as an initial finding of IgM nephropathy was reported in 23%/51% and 81%, isolated hematuria was reported in 23%/20% and 9%, proteinuria and hematuria was reported in 15, 27 and 0%, respectively.Citation9,Citation10,Citation12
In the isolated MsPGN group, the number of patients with nephrotic syndrome was significantly higher than the other groups at the time of application. This finding is consistent with Cohen's work.Citation9 One of our reasons for the biopsy indications of the patients with nephrotic syndrome was resistance to steroid. This result can be explained with the biopsy indications of the patients. Therefore, these cases had resistant nephrotic syndrome, and in fact during the follow-up 15 out of our 26 patients developed a proteinuria attack, requiring medical treatment and cytotoxic treatments were performed for these facts.
Clinical findings of HSN can extend from isolated microscopic hematuria to rapidly progressing glomerulonephritis. Hematuria and proteinuria were determined in most children with HSN. Hypertension and renal failure were seen rarely. Hematuria and proteinuria were seen together in 15% of the patients with renal failure.Citation3 In the study with 116 children and 46 adult patients with HSP which was done by Blanco et al.,Citation13 the rate of kidney involvement was shown in 29% of the children (hematuria and non-nephrotic proteinuria in 22%, nephrotic syndrome in 3% of patients) and they did not find renal failure.
Garcia-Porrua et al.Citation14 studied in a group with 73 children and 31 adult patients for 6 years. They reported hematuria and non-nephrotic proteinuria in 45% of children, nephrotic syndrome and/or acute nephritic syndrome in 8% of children.
Twelve out of 17 cases with HSN had hematuria that supports the rate in the literature. Additionally, the presence of both hematuria and proteinuria in patients with HSN was found in eight of 17 cases with concordance of the study of Erdag and Garcia.
The most characteristic abnormality in the biopsy results of the patients with isolated IgA nephropathy is the mesangial expansion that was due to the increment of hypercellularity and matrix.Citation15,Citation16 In the study of Haas with 244 cases, there were only mesangial hypercellularity in 15% of the cases without focal or segmental glomerular sclerosis.Citation17 Three types of mesangial changes were identified in the children with isolated IgA nephropathy: (1) the mesangial hypercellularity is more obvious than the increment of matrix, (2) the increment of mesangial hypercellularity and matrix is equal to each other, (3) increase in matrix is more obvious than mesangial hypercellularity.Citation15 First type of the lesion was observed in the biopsy specimens in which biopsy was performed shortly after the start of disease. The lesions characterized with the increase in matrix were observed in the biopsy specimens, which were there for a long interval between biopsy and the start of disease. It was also seen in the high proportion of the patients with glomerular sclerosis. These findings made us thought that the progression of isolated IgA nephropathy produce slowly unfolding mesangial hypercellularity resolution, whereas the matrix increases and glomerular sclerosis occurred.Citation18
The mesangial hypercellularity was dominant in all of our cases (mild/severe), while increased mesangial matrix was not clear. This phenomenon might be secondary to biopsy in early stage. There are not enough studies about the histology of the IgM nephropathy and isolated MsPGN when compared to the isolated IgA nephropathy and HSN, and most studies evaluated both children and adult cases. Moderate or severe intensity with a light microscope and mesangial matrix increment were reported in IgM nephropathy, but also reported that glomerule might be normal.Citation8,Citation11,Citation19,Citation20 Cavallo et al.Citation21 found the mesangial cell increment in the 33% of 21 IgM nephropathy cases. Various studies found the mesangial cell increment between 50 and 100% in IgM nephropathy.Citation9,Citation10,Citation12 Because we included the patients with mild mesangial hypercellularity into our study, mesangial hypercellularity was observed 100% in our cases.
Histopathologic changes of the HSN may vary from minimal lesion disease to the common crescentic glomerulonephritis. The basic kidney lesion of the HSN is endocapillary proliferative glomerulonephritis and also it is accompanied by mesangial cell increment.Citation22–24 Histopathological changes in the HSN are classified into six groups according to the mesangial proliferation, crescent formation and weight with the criteria of ISKDC.Citation25 Kawasaki et al.Citation26 reported that detection of proliferative glomerulonephritis and storage in mesangial, subepithelial and subendothelial areas are poor prognostic features. About 70% of cases with HSN had severe mesangial hypercellularity. This ratio was not found in the isolated IgA nephropathy. The reason of this may be a systemic inflammation in organism, there can be a multi-organ involvement. Increased metabolism and hemodynamics may contribute to severe hypercellularity.Citation27
The monitoring of isolated IgA nephropathy cases resulted in the literature that supports because of lower age at the diagnosis and the expectation of renal failure in the elder ages. O'Donoghue et al. reported 40% remission, 26% progression to end-stage renal failure and 15% relapse in 77 patients with IgM nephropathy.Citation28 On the other hand, Lawler et al. have identified 4/23 end-stage renal failure, 5/23 reduced kidney function, Cohen et al. have identified 6/29 reduced kidney function, Tejani et al. have identified 2/25 chronic renal failure.Citation9,Citation19,Citation28 Bhasin et al.Citation10 have not identified progression to the renal failure. We did not observe renal failure during the follow-up in both IgM nephropathy and isolated MsPGN cases. Our results are in accordance with the results of Bhasin et al. The reason for the absence of chronic renal failure might be the young age of children in both series.
When we look at the comparison of the groups among themselves, there was a significant hematuria only isolated IgA nephropathy, but there was no difference in biochemical values and prognosis when the mesangial hypercellularity was mildly or the same with the other groups. As a reason of this situation, there are different attitudes for renal biopsy indications in patients presenting with microscopic hematuria, e.g., IgA nephropathy encounter rate is high in the series which was biopsy indication placed for the reason of microscopic hematuria only six-month follow-up. However, IgA nephropathy can appear initially with hematuria and if we consider that it can improve proteinuria in the future, the effect of these parameters will be different in the long period biopsies. Therefore, proteinuria will be added to the hematuria. Hematuria was found to be significantly higher rate than the other groups, because biopsy was performed in patients with six months persistent microscopic hematuria in our clinic.
Chronic renal failure was not observed in IgA nephropathy in childhood, but may occur later in their life. However, chronic renal failure may occur in childhood in HSN and it is rare in the elder ages. While IgA nephropathy progress, HSN does not have progression though it shows the histopathological features of IgA nephropathy and new lesions does not occur. While mesangial hypercellularity was observed in both of our groups, endocapillary proliferative, glomerular sclerosis and crescent formation were not observed. Since extrarenal involvement in HSN may be a form of systemic IgA nephropathy.Citation29
There was no difference in clinical and laboratory parameters between the isolated IgA nephropathy with mild mesangial hypercellularity and HSN groups. Similarly, there was no difference in the parameters between the patients with severe mesangial hypercellularity. However, the number of patients with severe mesangial hypercellularity was statistically higher in the HSN group. This result was consistent with the studies of Zhou and Hamada.Citation29,Citation30 The value of proteinuria in the HSN group was statistically higher than the isolated IgA nephropathy group. Davin et al.Citation31 found higher values of proteinuria in the HSN group that was higher in the cases with IgA nephropathy. High levels of proteinuria in our patients may be secondary to more patients with severe mesangial hypercellularity.
In other words, if a child with HSN has proteinuria and GFR, and blood pressure is normal at the application, more severe mesangial hypercellularity is often expected in the renal biopsy when compared with IgA nephropathy.
There was no difference in prognosis for patients in each group. Prognosis was defined that hematuria and/or proteinuria occur in bouts during follow-up. According to this definition, hematuria and/or proteinuria were no supposed to occur between attacks. There was no proteinuria and hematuria in our cases except attack. The normal kidney function was being expected, because the patients were selected from the cases that did not have glomerulosclerosis, glomerular necrosis and/or endocapillary proliferative in the histopathological result.
As a result, there was no direct relationship between the severity mesangial hypercellularity and clinical and laboratory findings in the children with IgA nephropathy, IgM nephropathy and isolated proliferative mesangial hypercellularity. However, in the comparison of Henoch–Schönlein nephritis and IgA nephropathy, the number of cases with severe mesangial hypercellularity in the HSN was higher and also the value of proteinuria in these cases was found higher. At the same degree of mesangial hypercellularity, there was no difference in proteinuria, glomerular filtration rate and biochemical values.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Delos Santos NM, Wyatt RJ. Pediatric IgA nephropathies: clinical aspects and therapeutic approaches. Semin Nephrol. 2004;24:269–286
- Petros MZ, Emmanuel K, Lydıa N, et al. Glomerulopathy with mesangial IgM deposits: long-term follow up of 64 children. Pediatrics Int. 2001;43:287–292
- Kasap B, Kundak A, Türkmen M, et al. Correlation of IgA accumulation with clinical findings in children with Henoch-Schönlein nephritis. Rheumatism. 2008;23:114–117
- Remuzzi G, Bertani T. Pathophysiology of progressive nephropathies. N Engl J Med. 1998;12:1448–1454
- Daha MR. Mechanism of mesangial injury in glomerular disease. J Nephrol. 2000;13:89–95
- Cotran RS, Kumar V, Robbins SL, eds. The kidney. In: Robbins Pathologic Basis of Disease. 7th ed. Philadelphia, PA: WB Saunders; 2003:927–989
- Nozawa R, Suzuki J, Takahashi A, et al. Clinicopathological features and the prognosis of IgA nephropathy in Japanese children on long-term observation. Clin Nephrol. 2005;64:171–179
- Heptinsall RH. Classification of glomerulonephritis: focal and mesangial proliferative forms. In: Heptinsall RH, ed. Pathology of the Kidney. Boston, MA: Little Brown and Company; 1992:278–281
- Cohen A, Border W, Fong H. Glomerulonephritis with mesangial IgM deposits. Kidney Int. 1982;21:147 (Abstract)
- Bhasin HK, Abuelo JG, Nayak R. Mesangial proliferative glomerulonephritis. Lab Invest. 1978;39:21–29
- Nadasdy T, Silva FG, Hogg RJ. Minimal change nephrotic syndrome – focal sclerosis complex (including IgM nephropathy and diffusse mesangial hypercellularity). In: Tisher CC, Brenner BM, eds. Renal Pathology: With Clinical and Functional Correlations. 2nd ed. Philadelphia, PA: J.B. Lippincott Company; 1994:331–389
- Helin H, Mustonen J, Pasternack A, Antonen J. IgM-associated glomerulonephritis. Nephron. 1982;31:11–16
- Blanco R, Martinez-Taboada VM, Rodriguez-Valerde V, García-Fuentes M, González-Gay MA. Henoch-Schönlein purpura in adulthood and childhood. Arth Rheumatol. 1997;5:859–864
- Garcia-Porrua C, Calvino MC, Llorca J, Couselo JM, González-Gay MA. Henoch-Schönlein purpura in children and adults. Semin Arth Rheumatol. 2002;32:1149–1156
- Yoshikawa N, Iijima K, Maehara K, et al. Mesangial changes in IgA nephropathy in children. Kidney Int. 1987;32:585–589
- Yoshikawa N, Ito H. Nakamura H. IgA nephropathy in children from Japan. Clinical and pathological features. Child Nephrol Urol. 1988;9:191–199
- Haas M. Histologic subclassification of IgA nephropathy: a clinicopathologic study of 244 cases. Am J Kidney Dis. 1997;29:829–842
- Holliday MA, Barrat TM, Avner ED, eds. IgA nephropathy. In: Pediatric Nephrology. 5th ed. College Park, MD: Williams and Wilkins; 2004:615–628
- Tejani A, Nicastri AD. Mesangial IgM nephropathy. Nephron. 1983;35:1–5
- Mallick NP. Epidemiology and natural course of idiopathic nephrotic syndrome. Clin Nephrol. 1991;35:3–7
- Cavollo T, Johnson MP. Immunopathologic study of minimal change disease with mesangial IgM deposits. Nephron. 1981;27:281–284
- Athreya BH. Vasculitis in children. Pediatr Clin North Am. 1995;42:1239–1261
- Austin HA, Balow JE. Henoch-Schönlein purpura nephritis: prognostic features and challenge of therapy. Am J Kidney Dis. 1983;2:512–520
- Levy M, Broyer M, Arsan A ve ark. Henoch-Schönlein nephritis in childhood: natural history and immunopathology. Adv Nephrol. 1976;6:183–228
- White RHR, Yoshikawa N, Feehally J. IgA nephropathy and Henoch Schönlein nephritis. In: Holliday MA, Barrat TM, Avner ED, eds. Pediatric Nephrology. 4th ed. Baltimore, MD: Lippincott Williams and Wilkins; 1999:691–706
- Kawasaki Y, Suzuki J, Sakai N ve ark. Clinical and pathological features of children with Henoch Schönlein purpura nephritis: risk factors associated with poor prognosis. Clin Nephrol. 2003;60:153–160
- Takemura T, Murakami K, Miyazato H ve ark. Expression of Fas antigen and Bcl-2 in human glomerulonephritis. Kidney Int. 1995;48:1886–1892
- Sander JT, Wyatt RJ. IgA nephropathy and Henoch-Schönlein purpura nephritis. Curr Opin Pediatr. 2008;20:163–170
- Zhou JH, Huang AX, Liu TL. A clinico-pathological study comparing Henoch-Schönlein purpura nephritis with IgA nephropathy in children. Zhonghua Er Ke Za Zhi. 2003;41:808–812 [abstract]
- Hamada K. IgA nephropathy and Henoch-Schönlein purpura nephritis: clinicopathological, histopathological immunohistological, and electronmicroscopical characteristics. Hokkaido Igaku Zasshi. 1984;59:456–470 [abstract]
- Davin JC, Ten Berge IJ, Weening JJ. What is the difference between IgA nephropathy and Henoch-Schönlein purpura nephritis? Kidney Int. 2001;59:823–834
