Abstract
Opportunistic infection and reactivation of latent infection has been reported with use of monoclonal TNF alpha antibodies used for treatment of severe rheumatoid arthritis. We present a case of peritoneal tuberculosis (TB) causing renal failure secondary to ureteral constriction in a patient who had been treated with infliximab for rheumatoid arthritis. We suggest that physicians should be aware of the increased risk of false negative and false positive TST and IGRA among patients treated with monoclonal TNF alpha antibodies and should regularly look for usual and unusual symptoms of TB in this patient population.
Introduction
Opportunistic infection and reactivation of latent infection has been reported with the use of monoclonal TNF alpha antibodies used for treatment of severe rheumatoid arthritis. TNF alpha is required for recruitment of inflammatory cells and continued maintenance of granuloma structure; hence, plays an important role in protection against mycobacterium. Subsequently, inhibition of TNF alpha leads to failure of recruitment of these cells leading to re-activation of mycobacterium infection. We present a case of peritoneal tuberculosis (TB) causing renal failure secondary to ureteral constriction in a patient, who had been treated with infliximab for rheumatoid arthritis (RA).
Case report
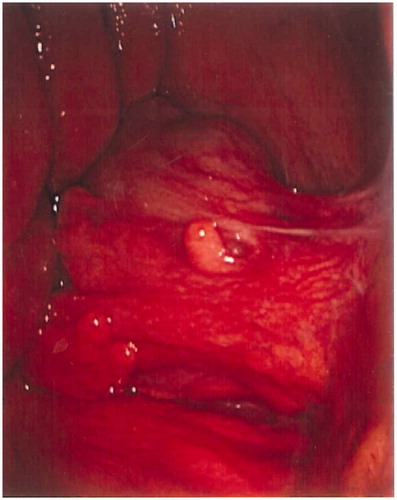
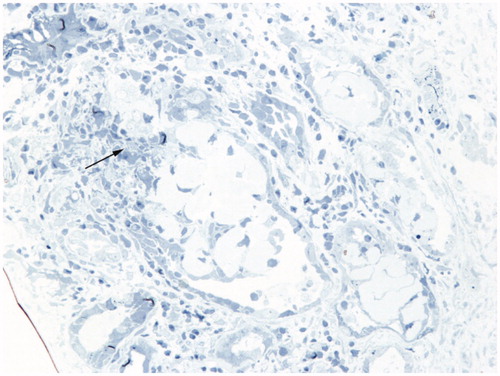
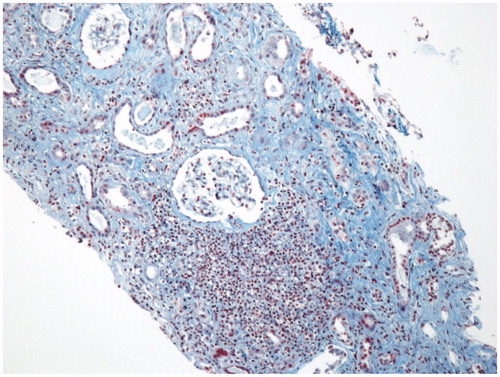
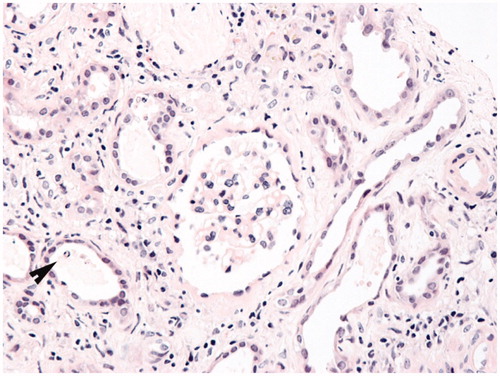
A 66-year-old female presented with intermittent fever and progressive abdominal distension for one month. She denied cough, abdominal pain, nausea, vomiting, diarrhea, constipation, sick contact, or recent travel. Past medical history is significant for RA that has been treated with TNF alpha inhibitor-infliximab for past one year. Physical examination showed moderate ascites. Blood work up reveal acute renal insufficiency (BUN/Cr 69/5.5). CT chest abdomen pelvis without contrast showed multiple enlarged mediastinal lymph nodes, measuring up to 1.1 × 1.8-cm at the right lower paratracheal and paraesophageal region, moderate ascites, nodularity of the peritoneum within the anterior lower abdomen, and upper pelvis ( and ). Paracentesis was performed and ascitic fluid analysis revealed exudative fluid, absence of acid-fast bacilli, and negative cultures. No growth was reported on repeated urine and sputum cultures. Peritoneal nodularity was seen on exploratory laparotomy () and peritoneal biopsy samples were send for pathological examination, which showed non-necrotizing granulomatous inflammation and positive acid fast bacteria (AFB). Special stain for fungi (GMS) was negative. Interstitial fibrosis and mild chronic inflammation (non-granulomatous) with extravasations of Tamm Horsfall protein was observed on IR guided renal biopsy (). Patient was subsequently started on anti-tuberculosis therapy, which resulted in resolution of acute renal failure and ascites.
Figure 1. Axial computed tomographic (CT) imaging of chest revealed multiple enlarged mediastinal lymph nodes (arrows), measuring up to 1.1 × 1.8-cm at the right lower paratracheal and paraesophageal region.
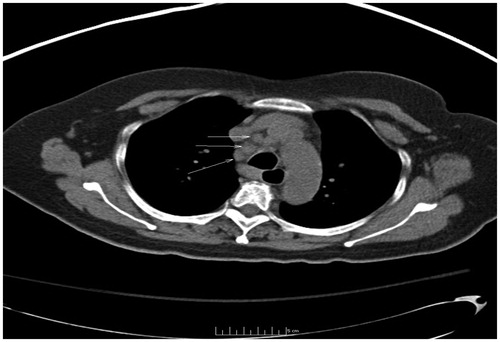
Figure 2. CT abdomen pelvis without contrast showed moderate ascites, nodularity of the peritoneum within the anterior lower abdomen and upper pelvis.
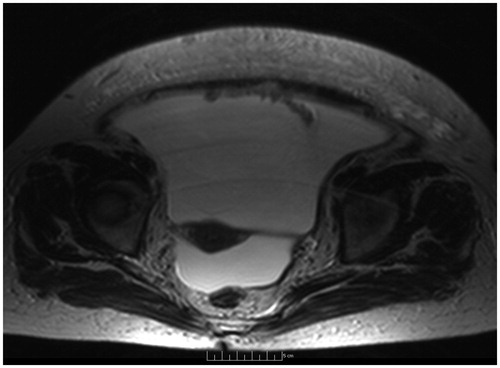
Figure 4. Biopsy shows simplification of the epithelial lining of renal tubules. Some renal tubules contain debris (arrowhead). Hematoxylin and eosin, original magnification ×200.
Discussion
Tuberculosis occurring in patient on monoclonal TNF alpha antibodies treatment is more likely to be disseminated, involving extra-pulmonary sites.Citation1 Our patient was found to have peritoneal tuberculosis with ureteral seeding, leading to ureteral constriction and renal failure. This risk in TB reactivation is greater with infliximab and adalimumab, in comparison to etanercept.Citation2 As per AERS database study (1998–2002), in US rate of TB was 54 per 100,000 among patients taking infliximab.Citation3 This high predilection of tuberculosis with infliximab may be due to higher blood levels received after intravenous infusion, higher reduction in interferon gamma and CD4 count with infliximab as compared to other monoclonal TNF alpha antibodies.Citation2,Citation4
Rheumatoid arthritis itself has been shown to increase the risk of mycobacterium infection in some studies.Citation5 In accordance to the CDC guidelines, it is crucial to screen for latent TB in all patients of RA before starting TNF alpha inhibitors. The screening includes pertinent history, physical exam, tuberculin skin test, or interferon gamma release essay (IGRA), and chest X-ray in those with positive TST/IGRA.Citation3 Our patient had a negative PPD and IGRA at the time of presentation. However, it should be noted that RA is associated with depressed T cell function in vivo and in vitro and TST and IGRA may be falsely negative or false positive (as they do not distinguish between eradication and persistence of infection) among these patients; hence, should be interpreted with caution.Citation6 In selected situations, anergy testing may assist in guiding individual decisions regarding individual therapy. However, results of currently available anergy testing methods in US populations have not been demonstrated to make a useful contribution to most decisions about isoniazid preventive therapy. Therefore, anergy testing is no longer recommended as a routine component of TB screening for immunocompromised patients in the United States.
Anti-tuberculosis therapy with a 2-month intensive phase with four drugs—rifampicin, isoniazid, pyrazinamide, and ethambutol (or streptomycin) followed by 4 to 7 months of continuation phase treatment with isoniazid and rifampin is recommended for extra pulmonary TB. However, duration of therapy is based on bacteriologic response and may even continue for more than 18 months.
Conclusion
Patients should be vigorously screened for TB before beginning treatment with monoclonal TNF alpha antibodies, as their use is associated with an increased risk of developing TB. Physicians should be aware of the increased risk of false negative and false positive TST and IGRA among patients treated with monoclonal TNF alpha antibodies and should regularly look for usual and unusual symptoms of TB.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Centers for Disease Control and Prevention (CDC). Tuberculosis associated with blocking agents against tumor necrosis factor-alpha – California, 2002–2003. MMWR Morb Mortal Wkly Rep. 2004;53:683–686
- Wallis RS, Broder MS, Wong JY, et al. Granulomatous infectious diseases associated with tumor necrosis factor antagonists. Clin Infect Dis. 2004;38:1261–1265
- Mazurek GH, Jereb J, Vernon A, et al. Updated guidelines for using Interferon Gamma Release Assays to detect Mycobacterium tuberculosis infection – United States, 2010. MMWR Recomm Rep. 2010;59:1–25
- Nestorov I. Clinical pharmacokinetics of TNF antagonists: how do they differ? Semin Arthritis Rheum. 2005;34:12–18
- Carmona L, Hernández-García C, Vadillo C, et al. Increased risk of tuberculosis in patients with rheumatoid arthritis. J Rheumatol. 2003;30:1436–1439
- Malone DG, Wahl SM, Tsokos M, Cattell H, Decker JL, Wilder RL. Immune function in severe, active rheumatoid arthritis. J Clin Invest. 1984;74:1173–1185