Abstract
Renal angiomyolipoma is a benign hamartomatous lesion which contains varying proportions of abnormal blood vessels along with muscle and fat component. Tuberous sclerosis predisposes to angiomyolipoma, and when associated, the lesion is often large with increased risk of hemorrhage and complications. When this occurs, transarterial embolization and surgery are the treatment options. Such a patient presented to us with acute onset of symptoms, and on account of severe anemia with active bleeding, transarterial embolization was performed. This was followed by elective nephrectomy without any complications. We present the imaging aspects of tuberous sclerosis and emphasize role of interventional radiology in this case.
Introduction
Angiomyolipoma (AML) of kidney is a benign hamartomatous lesion comprising muscle, fat and vascular tissue in varying proportions. Approximately 80% are sporadic and 20% are associated with tuberous sclerosis. They are frequently large, bilateral and show higher incidence of complications.Citation1 Imaging plays an integral role in work up owing to multisystem involvement of the syndrome.Citation2,Citation3 Due to rupture of intralesional aneurysms, patient may present with acute flank pain, distension, hematuria and shock.Citation1,Citation2 Image guided selective renal artery embolization is a minimally invasive procedure in both prophylactic and therapeutic setting with good response.Citation4–7
Case report
A 30-year-old female of Western Indian origin presented to us with acute onset complaints of increasing abdominal distension and flank pain. On clinical examination, there was mild pallor and tachycardia; also multiple cutaneous nodules were noted. Past history revealed below average performance in school, and occasional episodes of focal seizures. Hemoglobin at presentation was 5.5 gm/dL. Her initial work-up (including clinical examination and ultrasound of abdomen) was suggestive of bilateral renal masses.
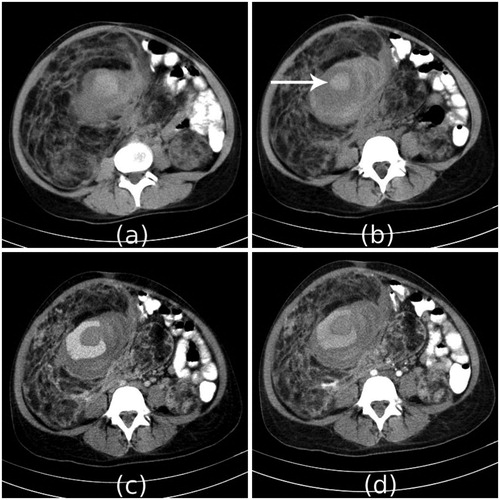
Patient underwent a dynamic contrast enhanced computed tomography (CT) of abdomen, which showed bilateral renal angiomyolipomas. The right renal angiomyolipoma measured 19 × 13 × 29 cm in size and showed pseudoaneurysm with surrounding acute hemorrhage and clot formation in inferior part (). Surrounding other angiomatous areas was also seen.
Figure 1. Non-contrast CT scan images (a), (b) show large mass of predominantly fat density replacing the right kidney. Similar lesion is also noted in the left kidney. It shows internal soft tissue and hyperdense area which represents acute hematoma (arrow). Arterial phase (c) and venous phase (d) images show contrast pooling in the lesion, which may suggest vascular ectasia.
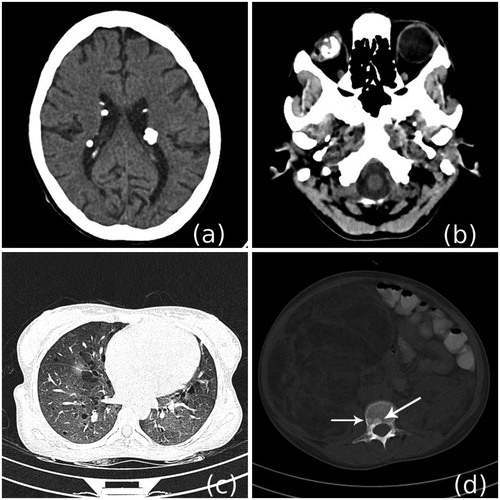
Screening CT examination also revealed a suspicious oncocytoma in upper pole of left kidney, multiple calcified subependymal nodules in the brain, calcified retinal hamartoma in right eye, multiple well defined cysts in both lung fields, sclerotic foci in few vertebrae and both innominate bones () suggestive of diagnosis of tuberous sclerosis.
Figure 2. NCCT scan of brain (a) and orbits (b) shows multiple calcified subependymal nodules, and calcified lesion in the right eyeball. Lung window images (c) show multiple thin walled cysts suggestive of lymphangioleiomyomatosis. Bone window image (d) shows few sclerotic lesions (arrow) in vertebra.
As patient was symptomatic, surgical excision of right renal angiomyolipoma was planned. However as patient was severely anemic and the lesion showed active hemorrhage, it was decided to do preoperative embolization followed by surgery 48 hours later.
Procedure
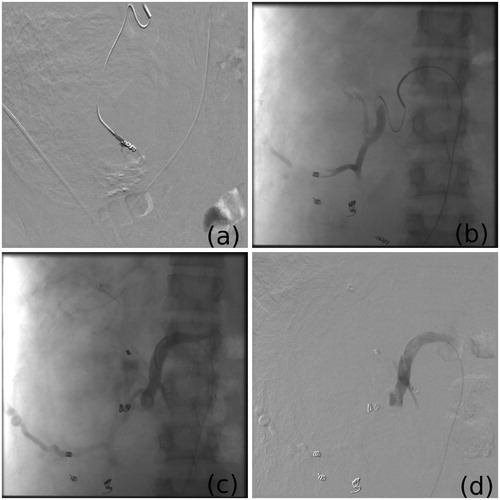
Through right common femoral artery puncture, 6F sheath was introduced and 5F Cobra 2 catheter was taken into right main renal artery. Angiogram revealed abnormal tumor vascularity, multiple aneurysms in tumor arteries and pseudoaneurysm in inferior part of tumor (). Artery supplying the tumor was selectively catheterized, and using Progreat microcatheter artery supplying the pseudoaneurysm was super selectively catheterized. This artery was embolized with polyvinyl alcohol particles and coils. Then similarly other tumor arteries were catheterized and first embolized distally with PVA particles and then proximally with coils (). Post embolization angiogram showed complete obliteration of tumour blush. No peri-procedural complications were noted.
Figure 3. Pre-procedure renal angiogram (a), selective tumor arterial angiogram (b) and demonstration of pseudoaneurysm (c), with placement of tip of microcatheter at pseudoaneurysm (d).
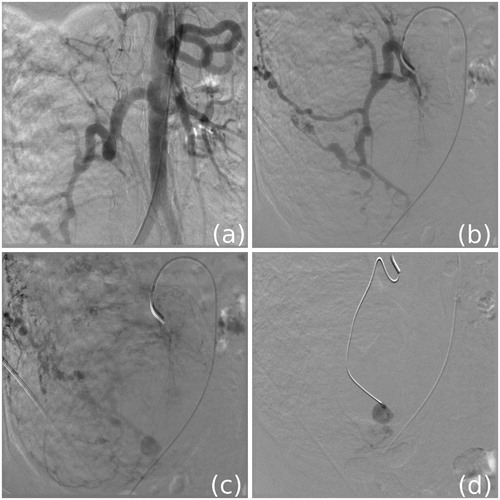
Figure 4. First the pseudoaneurysm is embolized (a) followed by lower (b) and upper (c) part of the lesion using PVA and coils. Post procedure angiogram (d) shows absence of tumor blush.
On second post procedure day, right radical nephrectomy was done. Intraoperative blood loss was 40 ml. Four units packed cell volume were transfused. Complete excision of the mass was feasible. Post operative period was uneventful and patient showed good recovery on follow-up.
Discussion
Angiomyolipoma is a benign hamartomatous renal tumour comprising of fat, smooth muscle and vascular components in varying proportions. AML is sporadic in about 80% of cases and associated with tuberous sclerosis in about 20% of cases.Citation1–3
Tuberous sclerosis is a neurocutaneous syndrome of hereditary predisposition, inherited by two genes, TSC1 coding hamartin and TSC2 coding tuberin.Citation1 TS classically presents with Vogt's triad of epilepsy, mental retardation and facial angiofibroma, however incomplete forms are frequently seen. Imaging plays an important role as patient may show involvement of only one system at presentation.Citation2,Citation3
The syndrome shows multisystem involvement with hamartomatous lesions, and presentation varies with age of the patient and organ of involvement.Citation1–3 According to Henry and Baskin, major criteria for diagnosis include facial angiofibroma or forehead plaque, periungual fibroma, hypomelanotic macules (more than three), shagreen patch, cortical tuber, subependymal nodule, subependymal giant cell astrocytoma, multiple retinal nodular hamartomas, cardiac rhabdomyoma, lymphangiomyomatosis, renal angiomyolipoma; and minor criteria include dental pits, hamartomatous rectal polyps, bone cysts, radial glial lines, gingival fibromas, non-renal hamartoma, retinal achromic patch, “confetti” skin lesions, multiple renal cysts.Citation1
Our patient showed presence of bilateral renal angiomyolipomas, calcified subependymal astrocytomas, calcified retinal hamartoma, lymphangioleiomyomatosis and cutaneous angiofibromas. Thus at least five major criteria were fulfilled suggesting definite diagnosis of TS.
AML may show abnormal tumoral vascularity with ectasia and aneurysm formation, due to hamartomatous disruption of vasa vasorum. This may predispose to rupture and hemorrhage.Citation1 Factors that are shown to be associated with a higher chance of hemorrhage in AML include size greater than 8 cm, multiplicity, association with TS, presence and size of intralesional aneurysms.Citation7–9
When it is symptomatic, as in our patient, treatment is necessary. Options include embolization and nephrectomy.Citation8,Citation9
Image guided transarterial selective renal embolization is a safe and minimally invasive procedure, which continues to be preferred in recent times over surgery.Citation10 It is especially useful in patients presenting with tumor bleed, and can demonstrate the rich vascular supply and site of active bleeding.Citation4,Citation10 It is the only option in patients with single functioning kidney, severe bilateral renal involvement, and those unfit for major surgery, like our patient. Other arguments favoring this procedure are that AML is a benign tumor, hemorrhage is the usual cause of symptoms, and embolization can preserve healthy renal parenchyma.Citation10,Citation11
However in patients with large tumor causing hemorrhagic and pressure symptoms, pre-operative embolization followed by partial or total nephrectomy is required to relieve patient symptoms. Pre-operative embolization in these cases controls active bleeding, and it also aids in reducing intraoperative blood loss. This allows a non-resectable tumor to be resectable, as in our case.Citation8,Citation9
Embolization is performed under local anaesthesia. In patients with non-functioning kidney or with life threatening hemorrhage, embolization can be performed from main renal artery. In other cases superselective embolization of the artery supplying the tumor is done.Citation5,Citation9,Citation11 Embolization is done with PVA particles and coils.Citation4,Citation5 However, use of PVA particles alone is associated with higher incidence of post-procedure tumor bleed.Citation4 This procedure has a low failure rate, is generally associated with acceptable complications, low-morbidity and no mortality.Citation5,Citation6,Citation10 Follow-up shows good response with average size reduction of about 40 percentCitation6,Citation10 and well preserved renal function.Citation5,Citation10
Conclusion
Transarterial embolization of renal angiomyolipoma is a safe and minimally invasive procedure. It is a good alternative to nephrectomy and can also be used prior to surgery to control active hemorrhage, make non-resectable tumors resectable and minimize intraoperative blood loss.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article.
References
- Baskin HJ Jr. The pathogenesis and imaging of the tuberous sclerosis complex. Pediatr Radiol. 2008;38(9):936–952
- Umeoka S, Koyama T, Miki Y, Akai M, Tsutsui K, Togashi K. Pictorial review of tuberous sclerosis in various organs. Radiographics. 2008;28(7):e32
- Evans JC, Curtis J. The radiological appearances of tuberous sclerosis. Br J Radiol. 2000;73(865):91–98
- Lee SY, Hsu HH, Chen YC, et al. Embolization of renal angiomyolipomas: short-term and long-term outcomes, complications, and tumor shrinkage. Cardiovasc Intervent Radiol. 2009;32(6):1171–1178
- Planché O, Correas JM, Mader B, Joly D, Méjean A, Hélénon O. Prophylactic embolization of renal angiomyolipomas: evaluation of therapeutic response using CT 3D volume calculation and density histograms. J Vasc Interv Radiol. 2011;22(10):1388–1395
- Lenton J, Kessel D, Watkinson AF. Embolization of renal angiomyolipoma: immediate complications and long-term outcomes. Clin Radiol. 2008;63(8):864–870
- Dickinson M, Ruckle H, Beaghler M, Hadley HR. Renal angiomyolipoma: optimal treatment based on size and symptoms. Clin Nephrol. 1998;49(5):281–286
- Meiri H, Soejima K, Tokuda Y, et al. The management selection of renal angiomyolipoma. Nihon Hinyokika Gakkai Zasshi. 1996;87(10):1151–1157
- Moudouni SM, En-Nia I, Patard JJ, Lobel B, Guillé F. Arterial embolization in hemorrhagic renal angiomyolipoma. Prog Urol. 2001;11(2):235–238
- Stoica G, Kheir C, Schöenig A, et al. Preventive and emergency embolization of angiomyolipomas: our experience. Prog Urol. 2011;21(8):514–520
- Pappas P, Leonardou P, Papadoukakis S, et al. Urgent superselective segmental renal artery embolization in the treatment of life-threatening renal hemorrhage. Urol Int. 2006;77(1):34–41
