Abstract
Intravascular large B-cell lymphoma (IVLBCL) is a very rare subtype of extranodal large B-cell lymphoma. It may involve various organ systems such as skin, liver, lung or kidney. Isolated kidney involvement of IVLBCL is also very rare. Herein we report a very rare case of isolated renal IVLBCL presented with fever of unknown origin, acute kidney injury and nephrotic syndrome. Diagnosis was suspected with isolated high renal 18F fluorodeoxyglucose uptake in positron emission tomography and confirmed with renal biopsy. Complete remission was obtained with combined chemotherapy including rituximab. We reviewed the English literature in terms of IVLBCL with renal involvement and we could only find 16 such cases. Accordingly, fever, AKI and nephritic syndrome are the most common presenting symptoms in renal intravascular lymphoma.
Introduction
Intravascular large B-cell lymphoma (IVLBCL) is a rare subtype of non-Hodgkin lymphoma and characterized by the involvement of the lumens of the vessels and capillaries.Citation1 Heterogeneous symptoms may be observed depending on the involvement of the organ-system such as skin, liver, lung, kidney or central nervous system. Because lymphadenopathy, involvement of the peripheral blood or bone marrow is usually absent in the course of this aggressive and life threatening disease, early diagnosis and treatment may be difficult to achieve. Herein we report a very rare case of isolated renal IVLBCL presented with fever of unknown origin (FUO), acute kidney injury (AKI) and nephrotic syndrome.
Case presentation
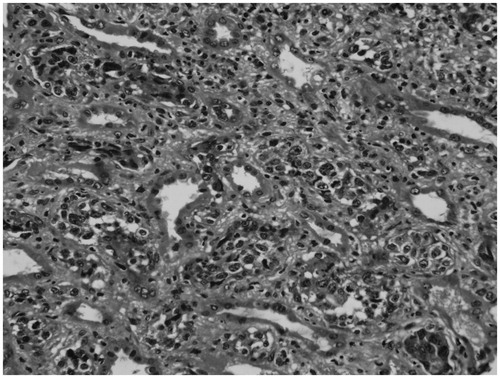
A 59-year-old male presented with high fever (up to 40 °C), weight-loss and fatigue for two months. The physical examination revealed paleness and severe pitting edema in the bilateral legs. Baseline biochemical parameters are presented in . Accordingly, neutrophilic leukocytosis, anemia, high serum creatinine, C-reactive protein and lactate dehydrogenase (LDH) levels were found. In urinalysis, 4.2 g/day proteinuria was found without hematuria or pyuria. Multiple blood and urinary cultures were taken however no microorganisms could be isolated. Wright test was also negative excluding the diagnosis of systemic brucellosis. Peripheral blood smear did not show any pathologic findings other than neutrophilic leukocytosis and hypochromic erythrocytes. No schistocytes or atypical cells were present in the smear. Coombs test was also negative. Protein electrophoresis showed polyclonal hypergammaglobulinemia (1.59 mg/dL) without a prominent M band. Anti-nuclear antibody was negative. With a pre-diagnosis of a malignancy, thorax and abdominal computed tomographies (CT) were performed however no mass or pathologic lymphadenopathy could be detected. A bone marrow biopsy was also performed and no pathologic finding was found. To rule out infective endocarditis as a cause of FUO, transthoracic echocardiography was also performed and no vegetation or sign of endocarditis could be detected. During the follow-up, urinary output gradually decreased and serum creatinine levels rapidly increased together with metabolic acidosis. Because of hypervolemia and severe metabolic acidosis, hemodialysis treatment was started. Thorax and abdominal CTs were repeated however they could not reveal any pathology. For the investigation of FUO and malignancy, 18F fluorodeoxyglucose positron emission CT (FDG-PET-CT) was performed which revealed diffuse FDG uptake of bilateral kidneys with a SUVmax of 13.80 (). Subsequently renal biopsy was performed revealing CD 20(+), PAX5(+), CD3(−) lymphocytes filling the lumens of the renal arterioles, venules and capillaries ( and ). The diagnosis of isolated renal intravascular large B cell lymphoma was established. Rituximab, cyclophosphamide, Adriamycin, vincristine and prednisolone (R-CHOP) regimen was started. After the treatment, high fever dramatically subsided within a couple of days. Serum creatinine levels declined dramatically and the need for dialysis disappeared. After the third session of the R-CHOP regimen, complete clinical response was obtained.
Figure 1. (a, b) FDG-PET-CT images depicting diffuse FDG accumulation in both kidneys with a SUVmax of 13.80.
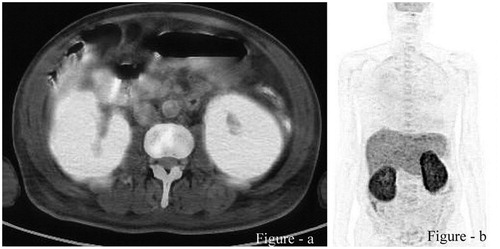
Figure 3. Renal biopsy revealed CD20 (+) lymphoma cells in renal arterioles, venules and capillaries.
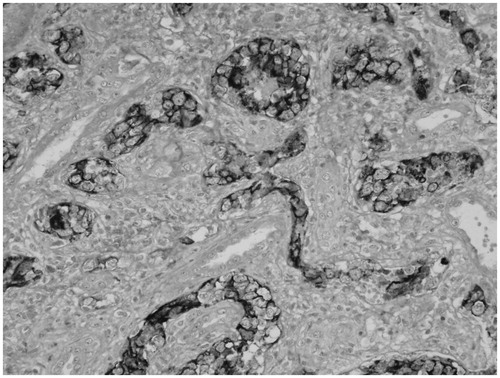
Table 1. Baseline biochemical data of the patient (BUN: blood urea nitrogen, LDH: lactate dehydrogenase, GGT: gamma-glutamyltransferase, ALT: alanine aminotransferase, AST: aspartate aminotransferase, WBC: white blood cell, PMNL: polymorphonuclear cells, LYM: lymphocytes, PLT: platelets, ESR: erythrocyte sedimentation rate, hs-CRP: high-sensitive C-reactive protein).
Discussion
IVLBCL is categorized as a type of extranodal large B-cell lymphoma in the 2008 WHO Classification of Tumors of Hematopoietic and Lymphoid Tissues.Citation2 IVLBCL are classified as non-germinal central type lymphomas.Citation3 IVLBCL is also known as angiotropic large cell lymphoma, intravascular lymphomatosis and malignant angioendotheliomatosis. It is characterized by selective growth of lymphoma cells the in the lumina of vessels.Citation1 IVLBCL is an extremely rare disease with an incidence of less than one person per one million individuals.Citation4 IVLBCL has been mostly described in older patients with a median age of 70 years. IVLBCL seemed to be present equally in men and women.Citation3,Citation4
Immuno phenotypically, IVLBCL was reported to express CD20 and CD5 in 36 of 96 patients (38.5%). In the cohort analysis by Shimada et al.Citation3, 48 of 84 (57%) patients with IVLBCL were found to have cytogenetic abnormalities however a pathognomonic cytogenetic abnormality has not been reported yet.
Presenting clinical features of this disease are variable and non-specific depending on the localization of the involvement. Anemia and elevated serum LDH levels are usually present.Citation6 The clinical patterns differ between two distinct geographical areas. In Asian countries, IVLBCL usually manifests with hepatosplenomegaly, pancytopenia and hemophagocytic syndrome however in the European countries, it is characterized by skin cutaneous variant and brain involvements.Citation6
The frequency of kidney involvement in the course of IVLBCL was found to be approximately 2%.Citation5 We reviewed the English literature in terms of IVLBCL involving kidneys and we could only find 16 cases of renal IVLBCL.Citation7–21 Clinical features, treatment modalities and outcomes of these cases are summarized in the . Accordingly, various clinical presentations may be observed in IVLBCL of the kidneys such as fever, AKI, proteinuria, edema, weight-loss and skin lesions. Fever seems to be the most common presenting symptom in IVLBCL involving kidneys. AKI is also common at a frequency of approximately 56% (9/16).
Table 2. Summary of the clinical features, treatments and outcomes of the IVLBCL cases involving the kidneys (CAVP: cyclophosphamide, doxorubicin, vincristine, prednisone, R-CHOP: rituximab, cyclophosphamide, Adriamycin, vincristine and prednisolone, AKI: acute kidney injury, VACOP-B: etoposide, doxorubicin, cyclophosphamide, vincristine, prednisone, bleomycin, LAP: lymphadenopathy).
The renal involvement of IVLBCL has been classified as either glomerular or tubulointerstitial invasion. Patients with tubulointerstitial type of disease usually present with bilateral enlarged kidneys.Citation12 AKI in IVLBCL is probably caused by obstruction of glomerular capillary tuft due to invasion of the lymphoma cells. The exact pathogenesis of nephrotic syndrome observed in the course of IVLBCL is not known. There are several studies reporting foot process fusion in electron microscopy raising the possibility of lymphoma-associated minimal change disease, probably induced by tumor related cytokines.Citation7,Citation15,Citation17,Citation19
The prognosis of IVLBCL is extremely poor and it is usually fatal without treatment in a few weeks to several months.Citation3 However prompt diagnosis and treatment may increase the rate of survival and cure.Citation11 Anthracycline based chemotherapeutic regimens are used for the treatment of IVLBCL. Retrospective studies have revealed that addition of rituximab to anthracycline based chemotherapy improved clinical outcomes. Among the patients with IVLBCL, the 2-year survival and progression-free survival rates in the rituximab group were 66% and 56%, compared to the group without rituximab, 46% and 27% respectively.Citation22
IVLBCL is a very rare cause of nephrotic syndrome and acute kidney injury. FDG-PET-CT may be especially very helpful for the early diagnosis of IVLBCL. A high-level of suspicion is required for the diagnosis of IVLBCL which is a potentially life-threatening but treatable disease.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article.
References
- Ponzoni M, Ferreri AJ, Campo E, et al. Definition, diagnosis, and management of intravascular large B-cell lymphoma: proposals and perspectives from an international consensus meeting. J Clin Oncol. 2007;25:3168–3173
- Campo E, Swerdlow SH, Harris NL, Pileri S, Stein H, Jaffe ES. The 2008 WHO classification of lymphoid neoplasms and beyond: evolving concepts and practical applications. Blood. 2011;117(19):5019–5032
- Shimada K, Kinoshita T, Naoe T, Nakamura S. Presentation and management of intravascular large B-cell lymphoma. Lancet Oncol. 2009;10:895–902
- Zuckerman D, Seliem R, Hochberg E. Intravascular lymphoma: the oncologist's “great imitator”. Oncologist. 2006;11:496–502
- Murase T, Yamaguchi M, Suzuki R, et al. Intravascular large B-cell lymphoma (IVLBCL): a clinicopathologic study of 96 cases with special reference to the immunophenotypic heterogeneity of CD5. Blood. 2007;109:478–485
- Ferreri AJ, Campo E, Seymour JF, et al. Intravascular lymphoma: clinical presentation, natural history, management and prognostic factors in a series of 38 cases, with special emphasis on the ‘cutaneous variant’. Br J Hematol. 2004;127:173–183
- D'Agati V, Sablay LB, Knowles DM, Walter L. Angiotropic large cell lymphoma (intravascular malignant lymphomatosis) of the kidney: presentation as minimal change disease. Hum Pathol. 1989;20:263–268
- Axelsen RA, Laird PP, Horn M. Intravascular large cell lymphoma: diagnosis on renal biopsy. Pathology. 1991;23:241–243
- Zhu J, Chen H, Ding G, Chen C. Mild proteinuria in a patient with glomerular limited intravascular large B-cell lymphoma. Clin Nephrol. 2013;80:286–292
- Sawa N, Ubara Y, Katori H, et al. Renal intravascular large B-cell lymphoma localized only within peritubular capillaries. Report of a case. Intern Med. 2007;46:657–662
- Niitsu N, Okamura D, Takahashi N, et al. Renal intravascular large B-cell lymphoma with early diagnosis by renal biopsy: a case report and review of the literature. Leuk Res. 2009;33:728–730
- Bai X, Li X, Wan L, Wang G, Jia N, Geng J. Intravascular large B-cell lymphoma of the kidney: a case report. Diagn Pathol. 2011;6:86 (1–5)
- Yoo J, Kuppachi S, Chander P. Quiz page. Large B-cell lymphoma, intravascular type, with diffuse glomerular and focal interstitial infiltration. Am J Kidney Dis. 2008;51:A43–A46
- Kusaba T, Hatta T, Tanda S, et al. Histological analysis on adhesive molecules of renal intravascular large B cell lymphoma treated with CHOP chemotherapy and rituximab. Clin Nephrol. 2006;65:222–226
- Nishikawa K, Sekiyama S, Suzuki T, et al. A case of angiotropic large cell lymphoma manifesting nephrotic syndrome and treated successfully with combination chemotherapy. Nephron. 1991;58(4):479–482
- Bilgili SG, Yılmaz D, Soyoral YU, Karadag AS, Bayram I. Intravascular large B-cell lymphoma presenting with anasarca-type edema and acute renal failure. Ren Fail. 2013;35(8):1163–1166
- Agar JW, Gates PC, Vaughan SL, Machet D. Renal biopsy in angiotropic large cell lymphoma. Am J Kidney Dis. 1994;24(1):92–96
- Kakumitsu H, Higuchi M, Tanaka K, Shibuya T. Nephrotic syndrome in a patient with intravascular lymphomatosis. Intern Med. 2003;42(1):98–101
- Shaknovich R, Francois DJ, Cattoretti G, D'Agati VD, Markowitz GS. A rare cause of nephrotic syndrome. Am J Kidney Dis. 2002;39(4):892–895
- Törnroth T, Heiro M, Marcussen N, Franssila K. Lymphomas diagnosed by percutaneous kidney biopsy. Am J Kidney Dis. 2003;42(5):960–971
- Cossu A, Deiana A, Lissia A, et al. Nephrotic syndrome and angiotropic lymphoma report of a case. Tumori. 2004;90(5):510–513
- Shimada K, Matsue K, Yamamoto K, et al. Retrospective analysis of intravascular large B-cell lymphoma treated with rituximab-containing chemotherapy as reported by the IVL study group in Japan. J Clin Oncol. 2008;26:3189–3195