Abstract
Our objective in this experimental study is to research the effect of the intra-abdominal pressure which rises following pneumoperitoneum and whether Theophylline has a possible protective activity on this situation. In our study, 24 Wistar Albino rats were used. Rats were divided into two groups. The first group was set for only pneumoperitoneum model. The second group was given 15 mg/kg of Theophylline intraperitoneally before setting pneumoperitoneum model. Then urea, creatinine, cystatin-C, tissue and serum total antioxidant capacity, total oxidant capacity and oxidative stress index in two groups were measured and compared with each other. Apoptosis and histopathological conditions in the renal tissues were examined. The differences between the groups were analyzed with the Mann–Whitney U test. Results were considered significant at p < 0.05. No statistically significant difference was determined between tissue and serum averages in two groups in terms of TAS, TOS and OSI values (p > 0.05). The mean value of urea were similar in pneumoperitoneum and pneumoperitoneum + theophylline groups (p = 0.12). The mean cystatin-C value was 2.2 ± 0.3 µg/mL in pneumoperitoneum, 1.74 ± 0.33 µg/mL in pneumoperitoneum + theophylline (p = 0.002). According to our study, lower cystatin-C levels in the group, where Theophylline was given, are suggestive of lower renal injury in this group. However, this opinion is interrogated as there is no difference in terms of tissue and serum TAS, TOS, OSI and urea values between the groups.
Introduction
Today, laparoscopic operations are commonly used in the group of all the ages for both diagnosis and treatment. It arouses interest due to advantages, such as especially removing necessity for a wide incision, postoperative hospitalization and healing period and prominently shortening the duration to return back to daily activities.Citation1 As a result of intra-abdominal mechanic pressure caused by pneumoperitoneum, there is increase in systemic vascular resistance, mean blood pressure, cerebral blood flow and intracranial pressure while decrease occurs in renal and portal blood flow and pulmonary compliance.Citation2,Citation3 Following cortical hypoperfusion and renal blood flow decreasing after increased intra-abdominal pressure (IAP), transient renal injury may occur.Citation4
Reperfusion is provided in the organs which remained ischemic by terminating pneumoperitoneum by abdominal desufflation. Free oxygen radicals (FOR) released by polymorphonuclear (PMNH) localizing on tissue during reperfusion and ischemia lead to destruction in the reperfused tissue. This case is called reperfusion tissue injury.Citation5,Citation6
Our objective in our experimental study is to research the effect of IAP increasing after pneumoperitoneum on renal functions and renal morphology and possible protective activity of Theophylline on this condition.
Material and methods
The study was conducted after ethical committee permission with 25 December 2012 date and 02 number by Süleyman Demirel University Animal Experiments Local Ethical Committee (SDU-HADYEK). In the experimental study, totally 24 adult male 12- to 16-week Wistar Albino rats weighing 250–350 g (average 319 g) were used. Animals were housed in the standard laboratory environment with a moisture of 55–60% at daylight for 12 h and dark for 12 h at a fixed temperature. Along housing, experiment animals were subjected to standard nutrition, housing and care conditions. The rats were divided into two groups. Following midline incision under general anesthesia, the rats in the group 1 (12 rats) were entered by Veress needle; after pneumoperitoneum was generated by insufflating inside the abdomen by CO2 at 14 mmHg fixed pressure for 1 h, desufflation was waited for 30 min; after this duration was completed, abdomen was opened and both kidneys were excised and sent to pathology and biochemistry laboratory for examination. Blood specimens obtained were sent to biochemistry laboratory only. Then the rats were sacrificed by leaving bleeding at the end of anesthesia.
The rats in the second group (12 rats) were administered 15 mg/kg of Theophylline through intraperitoneal way 1 h before the procedure. Subsequent procedures were exactly the same as group 1. In the experimental model, models generated previously in literature were based on determining the insufflation and desufflation time.Citation7–9
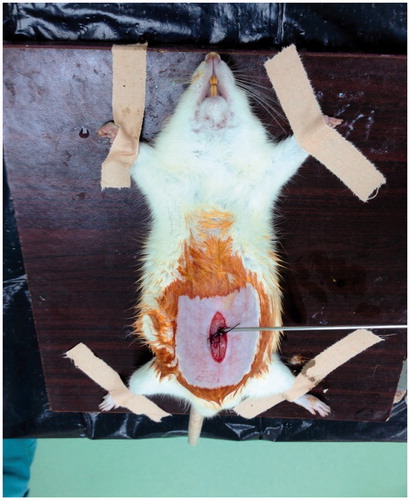
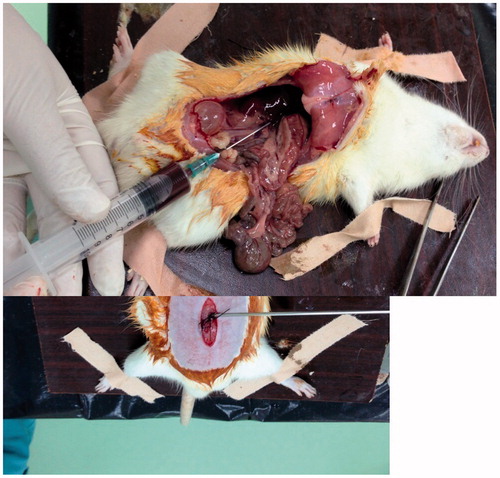
In order to create anesthesia in all the surgical operations, 90 mg/kg of Ketamine HCl (Ketalar®, Parke-Davis, Morris Plains, NJ) and 15 mg/kg of Xylazine HCl (Rompun®, Bayer, Germany) were administered intraperitoneally by the help of insulin injector. Following anesthesia, the abdominal region of all the animals were shaved and cleaned by 10% povidone–iodine. After ∼1 cm midline incision was performed and cutaneous and subcutaneous tissues were passed, Veress needle was placed into the peritoneal cavity. The same procedure was applied for the rats in all the groups (). The other end of needle was attached with CO2 insufflator (Storz, Germany). Following desufflation duration, blood and tissue specimens were taken by laparotomy incision ().
Half of renal specimens received were stored for biochemical examination and the other half for pathological examination. After 5–7 cc blood obtained was centrifuged and serum was obtained, it was stored in deep freezer (Wise Cryo, Germany) at −80 °C until biochemical measurement duration. While one of two renal tissues received from each rat was stored in deep freezer (Wise Cryo. Germany) at −80 °C for biochemical measurement, the other kidney was divided into two half as vertically symmetric and stored in 10% formaldehyde fluid with phosphate tampon for histopathological examination.
Bloods obtained from the rats were centrifuged (NF 800, Turkey) for 10 min at 3000 rpm and stored at −80 °C (Wise Cryo., Germany) until they are tested after their serums were separated. Renal tissues were weighed on assay balance (Scaltec SPB33, Germany) and homogenized by mixing with phosphate tampon at a rate of 1/10. Homogenization procedure was completed in two steps: In the first step, it was dispersed for ∼1 min with tissue mechanic disperser (Janke & Kunkel Ultra-Turrax T25, Germany) and in the second step, it was exposed to sonicator (UW-2070 Bandeun Electronic, Germany) for 30 s. Homogenates obtained were centrifuged for 10 min at +4 °C at 10,000 g (Rotanta 460, Germany). Following backing up, their supernatants were stored at −80 °C up until they are tested (Bosch, Germany).
After serums were made dissolved at room temperature and vortexed (Labinco L-46, Breda, Netherlands), urea and creatinine levels were measured in autoanalyzer device as spectrophotometric by using commercial kit (Beckman Coulter AU 5800, Kanagawa, Japan). Jaffe method was used for measuring creatinine, kinetic UV test spectrophotometric method for urea. Serum cystatin-C level was detected by enzyme-linked immunosorbent assay (ELISA) by using BioVender (Brno, Czech Republic) branded rat-specific commercial kits, washing device (Biotek Instruments ELX50, Winooski, VT) and reading device (Oganon Teknika Microwell system Reader 530, Austria). The results were given in µg/mL.
After homogenates obtained from tissues were made dissolved at room temperature and vortexed (Labinco L-46, The Netherlands), Total Antioxidant Status (TAS) and Total Oxidant Status (TOS) levels were measured as spectrophotometric by modified Erel method by using Reel Assay (Gaziantep, Turkey) branded commercial kit (Beckman Coulter AU 5800). Protein levels of homogenates were measured as spectrophotometric by using microprotein commercial kit (Beckman Coulter, Beckman Coulter AU 5800).
The results of TAS and TOS values were given in mmol Trolox Eq/g protein for TAS, in µmol H2O2 Eq/g protein for TOS by dividing its own protein value of each specimen. Oxidative stress index (OSI) was calculated according to the following formula: OSI = TOS/TAS × 100.
Kidneys received for histopathological examination were fixed in 10% neutral formalin after either half was symmetrically separated in half in the middle on vertical axis.
Following dehydration and paraffin inclusion procedure, tissues were embedded into paraffin blocks. Slices in thickness of 4–5 μm were obtained from paraffin blocks by means of rotary microtome. The slices obtained were stained with hematoxylin–eosin. Following staining procedure, all the slices were examined under optical microscope (Nikon Eclipse 400 research microscope, Tokyo, Japan) and evaluated and their photos were taken. The alterations found were scored by a modified semi-quantitative scale defined by Paller et al.Citation10 [1—chronic inflammation (0, +, ++); 2—tubular epithelial cell flattening (0, +, ++); 3—cytoplasmic vacuolization (0, +, ++); 4—cell necrosis and ischemic alterations (0, +, ++) and 5—tubuler lumen obstruction (0, +, ++)].
Apoptosis index was detected according to formula below by counting apoptotic nuclei marked as positive by TUNEL method in glomeruli, tubules and interstitial areas in 10 areas selected randomly at 40× magnification under OLYMPUS CX41 branded optical microscope (Tokyo, Japan); Apoptotic index (APOI) = Apoptotic nucleus number/Total cell number × 1005). According to this, it was evaluated as follows: 0 = no staining, 1 = mild (1–10%), 2 = moderate (10–40%) and 3 = severe (>40%).
Analyses were performed with PASW 18 (SPSS/IBM, Chicago, IL) software. The Kolmogorov–Smirnov test and P–P plot were used to verify the normality of the distribution of continuous variables. Results are reported as the mean ± SD or, in situations in which the distributions were skewed, as the median (min–max) and categorical variables are given as percentages. The differences between the groups were analyzed with the Mann–Whitney U test for non-parametric data, whereas chi-squared/Fisher’s exact test was used for categorical variables. Results were considered significant at p < 0.05.
Results
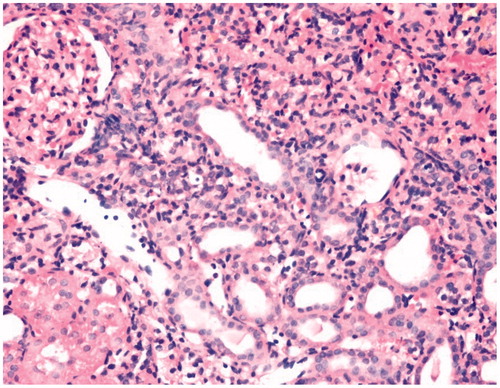
No characteristic difference was determined in terms of inflammation in the histopathological examination of kidneys in both groups (, and ). The average of apoptosis values between pneumoperitoneum and pneumoperitoneum + theophylline group were found as 46 ± 6.1 and 42 ± 5, respectively (p = 0.056).
Figure 4. Minimal inflammation findings in kidney tissue of the pneumoperitoneum + theophylline group (HE ×400).
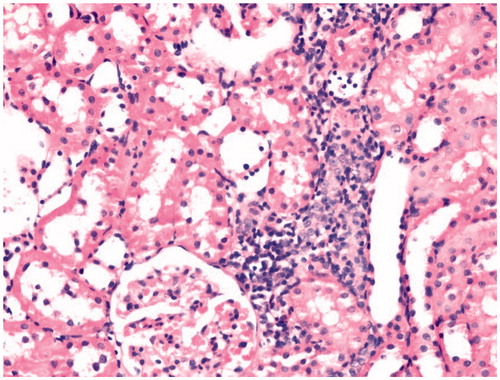
Table 1. Comparison of inflammation in the histopathological examination of kidneys in both groups.
No statistically significant difference was detected between tissue averages in terms of TAS, TOS and OSI values among groups (p = 0.27, p = 0.54 and p = 0.18, respectively).
Similarly, no statistically significant difference was found between serum TAS, TOS and OSI values (p = 0.20, p = 0.72 and p = 0.72, respectively) ().
Table 2. Comparison of TASt, TOSt, OSIt, TASs, TOSs, OSIs, urea, creatine and cystatine-c level between the groups.
The mean urea values in pneumoperitoneum and pneumoperitoneum + theophylline groups were similar (p = 0.12). Interestingly, the mean creatinine values were determined higher in theophylline group (p = 0.001). While the mean cystatin-C value in pneumoperitoneum group was detected as 2.2 ± 0.3 µg/mL, it was 1.74 ± 0.33 µg/mL in pneumoperitoneum + theophylline group (p = 0.002, ).
Discussion
During pneumoperitoneum performed for laparoscopic surgery, intra-abdominal pressure increases and undesired systemic and local impacts occur as a result of resorption of CO2 used from peritoneal surfaces. Increase in intra-abdominal pressure decreases systemic cardiac output by causing pressure on Vena Cava Inferior and causes hypoperfusion in organs by decrease in arterial pressure. Ultimately, pneumoperitoneum leads to a hypoxic environment at cell level.Citation11 Laparoscopic surgeries were shown to cause ischemia–reperfusion injury in organ and tissues depending upon hypoperfusion and subsequent reperfusion period.Citation12 Furthermore, it was shown that tissue perfusion of liver, kidney and bowels decreases when the intra-abdominal pressure is above normal vena portae pressure (7–10 mmHg).Citation13,Citation14
In literature, numerous agents were used in order to prevent renal ischemia–reperfusion injury. Melatonin, l-carnitine, N-acetylcysteine, nitroglycerine, PGE1, aminoguanidine and vitamin E were used experimentally and the results were found significant.Citation15–17 In order to prevent ischemia–reperfusion injury, these agents of which impacts were observed experimentally set light to researchers in terms of finding alternative and more effective agents. In our study, we applied 15 mg/kg of Theophylline through intraperitoneal way. In literature, theophylline was used in experimental models with respect to preventing pulmonary ischemia reperfusion injury, improving of acute renal failure seen in asphyxiating newborns, renal vasoconstriction and preventing tardive dyskinesia.Citation18–20 However, it is not used in any study for preventing renal ischemia reperfusion injury arising from pneumoperitoneum.
Following ischemia–reperfusion occurring, free oxygen radicals develop in tissues and oxidative stress resulting in when the balance of oxidant–antioxidant system impaired in favor of oxidant system causes various injuries in tissues. Researchers revealed that oxidative stress occurring is not only an indicatorCitation21 but also activates several mechanism causing functional and structural disorders in many organs, including also kidneyCitation22,Citation23 and liver,Citation24 by causing injuries in tissues as a result.Citation25 Free oxygen radicals play the most crucial role in disorders of renal functions after renal ischemia. Furthermore, it was reported that, following reperfusion, there is a rapid raise in free oxygen radicals and, as a consequence of this, there is increase in lipid peroxidation level.
When renal tissues received from the rats were evaluated histopathologically with hematoxylin–eosin, no characteristic difference was determined to occur between two groups in our study although there is an alteration in terms of only chronic inflammation from alteration specified in scale. When tissues received by TUNEL method used for evaluating apoptosis are looked at, the result does not show significant difference although the apoptosis value in pneumoperitoneum + theophylline group is lower than pneumoperitoneum group. In an experimental study performed by Farias et al.,Citation26 similarly, they did not encounter significant alterations in the examination with hematoxylin eosin in renal tissues received from the rats where pneumoperitoneum was applied. In another study, moderate hydropic degeneration and congestion were observed in both kidneys between the control group and the group where pneumoperitoneum was performed in the histopathological examination, but no significant difference detected.Citation27 In another study, however, in the histopathological examination of kidneys received from the rats, pathologic data varying from minimal alterations to moderate Acute tubular necrosis (ATN) in kidneys were obtained proportionally to increasing pressures.Citation7 When these results were considered, it could be thought that histopathological alterations occurring in kidneys change depending upon the duration to form pneumoperitoneum and the pressure of pneumoperitoneum formed.
Antioxidants are in interaction in plasma. Due to these impacts, more impact than the total impact formed by components alone occurs. Measurement of total antioxidant status can give more valuable information than measurement of antioxidants single by single. Antioxidant activity reflects the total activity of all the antioxidants found in plasma and body fluids.Citation28,Citation29 Total oxidant level measurement method was developed by Erel in order to measure oxidative stress caused by free radicals such as hydroxyl, hydrogen peroxide, singlet oxygen, lipid hydroperoxide and superoxide. Oxidative stress index is calculated to detect whether oxidative stress is balanced or not.Citation30,Citation31
No significant difference was able to be found between two groups of which mean TAS levels were measured in the kidney tissue taken. The mean TOS value measured in the tissue was determined lower in pneumoperitoneum group compared to pneumoperitoneum + theophylline group. Even if the difference is insignificant, higher TOS values in the treatment group suggest that antioxidant activity of theophylline given is not adequate. This result may depend on administration way or dose of theophylline. When the mean OSI data in the renal tissue were analyzed, the results in pneumoperitoneum + theophylline group were detected lower than pneumoperitoneum group as expected; however, no statistically significant difference was able to be determined between the results of these two groups.
No significant difference was found in TOS values in the results of TAS, TOS and OSI parameters in serums obtained from the rats. As expected in OSI and TAS values, the mean TAS values were detected lower in pneumoperitoneum group compared to pneumoperitoneum + theophylline group. Similarly, although OSI values were found higher in pneumoperitoneum group in proportion to pneumoperitoneum +theophylline group, no significant difference was observed between these two parameters among groups.
The reason why we found insignificant results in our study contrary to expectations may arise from inadequate gas pressures, insufflation and desufflation durations in the experimental model that we formed by the help of literature. TAS, TOS and OSI parameters used for evaluating the oxidative stress give general information about oxidative injury. We are of the opinion that more significant results can be obtained by studying with more specific parameters in order to evaluate oxidative stress.
The most used parameter in clinical practice is serum creatinine and urea values in order to show renal functions. In our study, creatinine, urea and cystatin-C parameters were examined to evaluate renal function parameters. In our study, no difference was detected between groups in terms of urea values. Interestingly, creatinine values in the group where theophylline was administered were found significantly higher. We have no reasonable explanation for this situation.
Cystatin-C is more specific and sensitive indicator than serum creatinine concentrations for glomerular filtration rate.Citation32 In a large number of clinical studies performed in children, adults and elderly people, cystatin-C was detected to show more diagnostic accuracy than serum creatinine for determining renal function disorder.Citation33
In an experimental study, where ischemia–reperfusion model was formed, cystatin-C was reported to be more sensitive than creatinine and BUN for detecting renal injury.Citation34 In another study, cystatin-C levels were found higher in rats where ischemia was formed experimentally compared to the control group and the group receiving treatment.Citation35 In our study, cystatin-C values were determined to be significantly lower in pneumoperitoneum + theophylline group. These our results show similarity to the studies performed previously in the literature.
Conclusion
According to our study, low cystatin-C levels in the group receiving theophylline suggest that renal injury in this group is lower. However, no difference between groups in terms of tissue and serum TAS, TOS, OSI and urea values and high creatinine values in theophylline group interrogate this opinion. Further studies are needed to clarify the protective effect of theophylline.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the article.
References
- Menes T, Spivak H. Laparoscopy: Searching for the proper insufflation gas. Surg Endosc. 2000;14(11):1050–1056
- Polat C, Yilmaz S, Serteser M, Koken T, Kahraman A, Dilek ON. The effect of different intraabdominal pressures on lipid peroxidation and protein oxidation status during laparoscopic cholecystectomy. Surg Endosc. 2003;17(11):1719–1722
- Rauh R, Hemmerling TM, Rist M, Jacobi KE. Influence of pneumoperitoneum and patient positioning on respiratory system compliance. J Clin Anesth. 2001;13(5):361–365
- Kirsch AJ, Hensle TW, Chang DT, Kayton ML, Olsson CA, Sawczuk IS. Renal effects of CO2 insufflation: Oliguria and acute renal dysfunction in a rat pneumoperitoneum model. Urology. 1994;43(4):453–459
- Kumar V, Fausto N, Robbins SL, Cotran RS. Robbins and Cotran Pathologic Basis of Disease. Philadelphia: Elsevier Saunders; 2005
- Slater TF. Free-radical mechanisms in tissue injury. Biochem J. 1984;222(1):1–15
- Khoury W, Schreiber L, Szold A, Klausner JM, Wienbroum AA. Renal oxidative stress following CO2 pneumoperitoneum-like conditions. Surg Endosc. 2009;23(4):776–782
- Bishara B, Karram T, Khatib S, et al. Impact of pneumoperitoneum on renal perfusion and excretory function: Beneficial effects of nitroglycerine. Surg Endosc. 2009;23(3):568–576
- Wiesenthal JD, Fazio LM, Perks AE, et al. Effect of pneumoperitoneum on renal tissue oxygenation and blood flow in a rat model. Urology. 2011;77(6):1508.e9–e15
- Paller MS, Hoidal JR, Ferris TF. Oxygen free radicals in ischemic acute renal failure in the rat. J Clin Invest. 1984;74(4):1156–1164
- Neudecker J, Sauerland S, Neugebauer E, et al. The European Association for Endoscopic Surgery clinical practice guideline on the pneumoperitoneum for laparoscopic surgery. Surg Endosc. 2002;16(7):1121–1143
- De Souza AMB, Wang CC, Chu CY, Lam PM, Rogers MS. The effect of intra-abdominal pressure on the generation of 8-iso prostaglandin F2alpha during laparoscopy in rabbits. Hum Reprod Oxf Engl. 2003;18(10):2181–2188
- Richter S, Olinger A, Hildebrandt U, Menger MD, Vollmar B. Loss of physiologic hepatic blood flow control (“hepatic arterial buffer response”) during CO2-pneumoperitoneum in the rat. Anesth Analg. 2001;93(4):872–877
- Davis JM, Gute DC, Jones S, Krsmanovic A, Korthuis RJ. Ischemic preconditioning prevents postischemic P-selectin expression in the rat small intestine. Am J Physiol. 1999;277(6 Pt 2):H2476–H2481
- Ergün O, Ulman C, Kiliçalp AS, Ulman I. Carnitine as a preventive agent in experimental renal ischemia-reperfusion injury. Urol Res. 2001;29(3):186–189
- Sahna E, Parlakpinar H, Cihan OF, Turkoz Y, Acet A. Effects of aminoguanidine against renal ischemia–reperfusion injury in rats. Cell Biochem Funct. 2006;24(2):137–141
- Romero F, Rodríguez-Iturbe B, Parra G, González L, Herrera-Acosta J, Tapia E. Mycophenolate mofetil prevents the progressive renal failure induced by 5/6 renal ablation in rats. Kidney Int. 1999;55(3):945–955
- Bhat MA, Shah ZA, Makhdoomi MS, Mufti MH. Theophylline for renal function in term neonates with perinatal asphyxia: A randomized, placebo-controlled trial. J Pediatr. 2006;149(2):180–184
- McLaughlin GE, Kashimawo LA, Steele BW, Kuluz JW. Reversal of acute tacrolimus-induced renal vasoconstriction by theophylline in rats. Pediatr Crit Care Med. 2003;4(3):358–362
- Bishnoi M, Chopra K, Kulkarni SK. Theophylline, adenosine receptor antagonist prevents behavioral, biochemical and neurochemical changes associated with an animal model of tardive dyskinesia. Pharmacol Rep. 2007;59(2):181–191
- Sies H. Oxidative stress: Oxidants and antioxidants. Exp Physiol. 1997;82(2):291–295
- Walker LM, York JL, Imam SZ, Ali SF, Muldrew KL, Mayeux PR. Oxidative stress and reactive nitrogen species generation during renal ischemia. Toxicol Sci. 2001;63(1):143–148
- Haugen E, Nath KA. The involvement of oxidative stress in the progression of renal injury. Blood Purif. 1999;17(2–3):58–65
- Serracino-Inglott F, Habib NA, Mathie RT. Hepatic ischemia-reperfusion injury. Am J Surg. 2001;181(2):160–166
- Yilmaz S, Koken T, Tokyol C, et al. Can preconditioning reduce laparoscopy-induced tissue injury? Surg Endosc. 2003;17(5):819–824
- Farias IEC, Morais PHA, Durães L C, Carneiro FP, Oliveira PG, Sousa JB. Effects of carbon dioxide pneumoperitoneum on hepatic and renal morphology of rats after segmental colectomy and colonic anastomosis. Acta Cirúrgica Bras Soc Bras Para Desenvolv Pesqui Em Cir. 2011;26(4):279–224
- Freitas PFS, Durães LC, Carvalho FANO, Duarte SAC, Carneiro FP, Sousa JB. Effects of pneumoperitoneum with carbon dioxide and helium on renal function and morphology in rats. Acta Cirúrgica Bras Soc Bras Para Desenvolv Pesqui Em Cir. 2013;28(7):494–449
- Tello S. Meme Kanseri Oluşturulmuş Ratlarda Isirgan Otunun Total Antioksidan Durumu Üzerine Etkisi. Firat Üniversitesi Sağlik Bilim Tip Derg. 2008;22(4):179–183
- Ching S, Ingram D, Hahnel R, Beilby J, Rossi E. Serum levels of micronutrients, antioxidants and total antioxidant status predict risk of breast cancer in a case control study. J Nutr. 2002;132(2):303–306
- Erel O. A new automated colorimetric method for measuring total oxidant status. Clin Biochem. 2005;38(12):1103–1111
- Erel O. A novel automated method to measure total antioxidant response against potent free radical reactions. Clin Biochem. 2004;37(2):112–119
- Watanabe S, Okura T, Liu J, et al. Serum cystatin C level is a marker of end-organ damage in patients with essential hypertension. Hypertens Res. 2003;26(11):895–899
- Curhan G. Cystatin C: A marker of renal function or something more? Clin Chem. 2005;51(2):293–294
- Song S, Meyer M, Türk TR, et al. Serum cystatin C in mouse models: A reliable and precise marker for renal function and superior to serum creatinine. Nephrol Dial Transplant. 2009;24(4):1157–1161
- Efrati S, Berman S, Hamad RA, et al. Effect of captopril treatment on recuperation from ischemia/reperfusion-induced acute renal injury. Nephrol Dial Transplant. 2012;27(1):136–145