Abstract
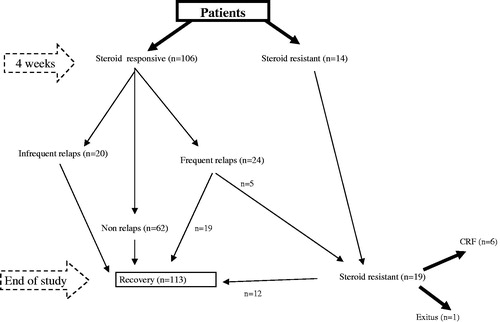
Idiopathic Nephrotic Syndrome (INS) was defined as combination of a nephrotic syndrome and non-specific histological abnormalities of the kidney. Among these abnormalities, minimal change nephrotic syndrome (MCNS) is the most common. We report our experience with MCNS; its clinical course, treatments and outcomes. One-hundred twenty children (66 male, 54 female) with MCNS, admitted to Nephrology Department between 1987–2009 was assessed. Their clinical presentations, treatment and disease courses were reviewed. The mean duration of follow-up was 11.5 ± 1.9 years. Initially, all patients given prednisone 2 mg/kg/ day single dose per four weeks a followed by eight weeks of the same daily dose given every other day. After week 12, prednisone was progressively tapered off at the rate of 0.5 mg/kg per 15 daily intervals until complete discontinuation had been achieved by week 16. Steroid resistance was accepted as no achievement of remission following four weeks of prednisone 2 mg/kg/day followed by three intravenous pulses of corticosteroids. At the end of the initial steroid treatment, 106 (88.3%) patients were determinate steroid responsive while 14 (11.7%) patients were steroid resistance. Thirty-eight patients underwent biopsy. At the end of study recovery rate was increased from 88.3% to 94.1%. In conclusion, most of patients entered remission by our therapy end of follow up time. With the support of our satisfactory results among the whole study group, long-term prednisolone treatment still remains valid.
Introduction
Idiopathic Nephrotic Syndrome (INS) was defined as combination of a nephrotic syndrome and non-specific histological abnormalities of the kidney including minimal change nephrotic syndrome (MCNS), focal segmental glomerulosclerosis (FSGS) and diffuse mesangial proliferation (DMP).Citation1 The annual incidence of INS in the general pediatric population is 2–7 per 100,000 and the prevalence is 16 per 100,000.Citation2
MCNS is the most common cause of INS in children, accounting for more than 75% of all pediatric cases and for 90% of cases in children younger than five years of age.Citation3
The causes of INS by definition remain unknown but evidence exists that a primary T-cell disorder may be responsible in MCNS and FSGS. The first suggestion that increased glomerular basement membrane permeability was caused by a lymphokine was made more than 30 years ago.Citation4 Despite numerous studies, the identity of this “glomerular permeability factor” remains elusive, but a host of experimental observations propose a T-cell-driven circulating factor that interferes with glomerular perm-selectivity to albumin.Citation5
By the knowledge of protein accumulation in lysosomes of proximal tubules, due to increased protein internalization is thought to mediate inflammation and fibrosis, eventually leading to renal failure.Citation6 Thus the best prognostic indicator in all the histological variants of the INS is the response of proteinuria to therapy.Citation7–10 Therefore, the objectives of treatment are threefold: to lower proteinuria, to reduce the frequency of relapses and to sustain the basal level of GFR (glomerular filtration rate) thus prevents progression to renal failure.
Although histological variants of INS carry prognostic significance they cannot be considered as separate entities at present.Citation11
In the consideration of repeated renal biopsies in INS, have shown morphological transition between the three main histological patterns, we can generalized the result that prognosis of INS mainly depends on the steroid response.Citation12,Citation13 There are currently a large number of effective therapeutic options for the management of NS, and the relative position of one against another is determined by the available scientific evidence and by the clinicians’ experience.Citation14 Most children with MCNS respond to steroid. However up to 50% of patients with MLH develop frequently relapsing and/or 10–15% SRNS (steroid resistant nephrotic syndrome) and often required immunosuppressive treatment.Citation15 The long-term prognosis is generally good, but almost 25% of the cases required prolonged treatment (18 weeks) with corticosteroids.Citation16 Although previous data reported better prognosis with the long-term treatment, there were any clear consensus about steroid treatment duration.Citation17,Citation18 Various regimes of corticosteroids have been used. The aim of this study is to report our experience with INS in the long-term steroid treatment.
Patients and methods
We assessed 120 children (66 male, 54 female) with MCNS admitted to Ege University Children Hospital Nephrology Department, Izmir, between 1987–2009. Their clinical presentations, treatment and disease courses were retrospectively reviewed. The mean duration of follow-up was 11.5 ± 1.9 years. At presentation, the presence of any accompanying diseases, majority of initial complaints, common physical findings, anthropometric parameters (height, weight, body surface area), albumin and lipid values, levels of proteinuria in 24 hours collected urine were evaluated. None of the patients had hematuria (microscopic or macroscopic), hypertension, uremia and hypocomplementemia at presentation. Patients having secondary nephrotic syndrome were excluded from study.
NS is defined as the presence of signs and symptoms including edema, hypoalbuminemia (serum alb <3 g/dL), nephrotic proteinuria and hypercholesterolemia. Nephrotic proteinuria is defined as urine protein (mg/dL)/urine creatinine (mg/dL) (Up/Ucr) ratio >2 or 24 hours collected urine protein >40 mg/m2/hour. Remission is defined as Up <4 mg/m2/hour or Up/Ucr <0.2 mg/mg for three consecutive days. Absence of remission after four week of daily steroid therapy at a dose of 2 mg/kg/day, followed by three high doses of pulse steroid is called, resistance. Frequent relapses were having relapses more than two, within six months or four within twelve months. Also patients having relapse with steroid taper or within two weeks of steroid withdrawal, were referred to as steroid dependent (SDNS).
Initially, all patients were treated with a single dose of 2 mg/kg/day (maximum 60 mg/day) prednisolone for four weeks, followed by eight weeks of the same daily dose given every other day.
During the first four week, penicillin V, gastro-protective agent, calcium plus D vitamin were given. After twelfth week, prednisone doses were gradually decreased with a rate of 0.5 mg/kg per 15 daily intervals until complete discontinuation had been achieved by week 18th. The response to therapy was classified according to the definitions from the International Study of Kidney Disease in Children (ISKDC), as mentioned above. Renal biopsy was performed in the following situations by obtaining the informed consent: (1) age of onset younger than two and older than eight years (2) Steroid resistant or dependent. Frequent relapsers and SRNS were treated with cyclophosphamide and /or cyclosporine, after performing renal biopsy. The patients were evaluated for the side effects of steroid therapy, whether the short stature, cataract, osteoporosis and glucose intolerance were present.
Molecular analysis was also performed to evaluate to possible association of podocin gene mutations in SRNS and frequent relapsers and association of nephrin gene mutations in patients with early onset.
Statistical analysis
Descriptive statistics are presented as percentages, means and standard deviations. Univariate analyses for group comparisons of continuous variables were performed using Student t test.
Multivariate analyses for group comparisons were performed using analysis of covariance. The correlation between measurements and continuous variables was determined using the Pearson correlation coefficient. Chi-square test was used to analyze the relative percentage of categorical variables by group. p-Value less than 0.05 indicated statistical significance. Data were expressed as mean ± SD. Differences in categorical variables between groups were tested with Fisher’s exact and chi-square tests. Differences in mean values between groups were examined for statistical significance by using the Mann–Whitney U test. p < 0.05 was accepted as statistical significant.
Results
Total number 120 children (66 male, 54 female) were evaluated with a follow up of 11.5 ± 1.9 years. At the end of the four weeks of steroid treatment, we classified patients into two groups. Steroid responsive patients (n = 106) were called as group 1, steroid resistant patients (n = 14) were called as group 2. Then group 1 was divided into three subgroups, 62 patients (58, 5%) as non-relapsers, 20 patients (19%) as rare relapsers and the rest 24 (23%) as frequent Relapsers (also called SDNS). The demographic characteristics, physical and laboratory data at the time of first admission are given in . All members of group 2 and frequent relapsers were admitted with edema, some of them were having also oliguria. Mean age of onset was 138.6 ± 19 in group 1 whereas 27 ± 12 in group 2 (p = 0.00). Another idiopathic nephrotic syndrome case in the first-degree relatives was found in 16% and 36% of frequent relapsers and SRNS group, respectively.
Table 1. Data at the time of admission.
Among frequent relapsers (SDNS) group, 11 patients (45.8%) had the second episode within the first year of diagnosis (n = 11), four of these 11(17%) patients had the second episode within six months of the initial response. At the end of study, 19 of 24 SDNS patients reached recovery, 5/24 progressed to SRNS. One patient had NPHS2 gene mutation, progressed to ESRD. The other one that followed as stage 1-CKD (chronic kidney disease) had NPHS1 mutation. The detailed clinical data were shown in .
Table 2. Clinical data of frequent relapsers who having second episode within first year (n = 11).
Physical findings, laboratory values at the onset of the disease were not predictive of the response to treatment in the children with MCNS (p > 0.05). Although, steroid-resistant patients were younger than steroid responsive patients (2.9 versus 4 years, p = 0, 30) ().
Table 3. The factors affecting of steroid response.
At the end of the follow-up period, 82 patients were steroid responsive without any adverse effect of treatment (cataract, and intolerance of glucose). None of these patients had failure to thrive according to their percentile charts. Sixty-two patients did not have any episode. Total 85% of patients achieved recovery within five years, 94% in 10 years. Nineteen steroid dependent patients (19/24, 79%) recovered in 10 years while the rest five were observed as SRNS. Therefore at the end of study, 19 patients were called as steroid resistant. During the follow up, 12/19 SRNS patients achieved recovery (63%), five progressed to CKD, one to ESRD and one patient died. The recovery rates of non relapsers, rare relapsers, SDNS and SRNS were found as, 100, 100, 79 and 63% respectively. Outcome of patients were shown in and and .
Table 4. Outcome in group 1 patients.
Table 5. Full recovery status of patients.
Patients younger than two years, older than eight years and SRNS, as a total number of 38 (32%) underwent biopsy. Histopathological analysis of biopsy revealed the underlying conditions of these 38 patients to be minimal change nephritic syndrome (17 patient; 44.8%), focal segmental glomerulosclerosis (14 patients; 37%), IgM nephropathy (five patients; 13%) and C1q nephropathy (two patients; 5.2%). MCNS was found in 17 of the patients underwent biopsy and the total incidence of MCNS (presumptive and biopsy proven) was 82.5%.
Discussion
INS has highly variable therapeutic managements. It’s more difficult to manage in children because of the young age and associated comorbid conditions.
Obtaining and maintaining the lowest level of proteinuria, will result in the best quality and quantity of both renal and patient survival.Citation3 Ruggenenti et al. showed that, in adults regardless of the underlying histology, patients with INS proteinuria 43.8 g/ day, had a 35% risk of end-stage renal disease (ESRD) within two years, compared to only a 4% risk for those with proteinuria <2.0 g/ day.Citation19
In our cohort, 106 (88.3%) patients were responsive to steroid treatment, at the end of four weeks of therapy. Two patients (1.6%) had progressed to ESRD, similar to literature. We analyzed the histopathological pattern of INS in our population by evaluating 38 patients who underwent biopsy. Our results show the most common histopathologic type is MCNS. FSGS was the second most common histopathologic subtype in our population. Recently studies from different countries have shown a higher incidence of FSGS in African, American and Indian children when compared to Hispanics and Causations.Citation20,Citation21 As we know Turkish children belong to Caucasians ethnicity our results were parallel to literature.Citation20,Citation21 Corticosteroids are the first-line treatment for MCNS. Approximately 95% of children with MCNS achieve remission of proteinuria within four weeks and complete remission after an eight week course of prednisone. We showed 88.3% of patient (n = 106) had remission of proteinuria within four weeks. Among children with steroid-responsive nephrotic syndrome (SSNS), relapse is common. It is estimated that 70% of children with nephrotic syndrome will experience one or more relapses.Citation22 However, the frequency of relapses decreases over time. In Cochrane review, a direct correlation was reported between longer duration of steroid therapy and longer duration of remission and an indirect correlation with frequency of relapse.Citation23
Tarshish et al. reported a gradual increase in the number of non-relapsing patients over time, such that eight years after disease onset, 80% of children were relapse-free.Citation24 In addition, 75% of those children either had neither relapses in the first six months nor rare relapses or continued in remission for their entire clinical course.Citation25 In our cohort, 4.7% of patients with SSNS (five patient in 106) had their second episode in the first six months of diagnosis ().
Ehrich et al. reported that, increasing the duration of corticosteroid therapy to a total of 12 weeks improves the rate of sustained remission.Citation26 Adults with MCNS generally receive lower doses of prednisone on a per kilogram basis (1 mg/ kg/ day for eight weeks), which may explain the lower-remission rate of only 50–60%. However, an increase in treatment duration to 16 weeks increases it to 80%.Citation27
Recent studies showed reduction of relapse rate (25–30%) with a steroid treatment regimen of three months or more.Citation17,Citation18,Citation27–29 In addition to these data it is reported that longer treatment duration is more important than the cumulative dose of steroids in reducing the risk of relapse.Citation30 This finding was supported with a meta-analysis study.Citation25 Longer initial steroid induction regime of ISKDC proposed and studied by Ueda et al. and Ksiazek & Wysznska, who showed a two-year relapse free rate of 50% for the long initial steroid dose versus 27.3% for the modified ISKDC regime.Citation17,Citation18 Despite that no additional benefit was demonstrated in 12 months treatment, compared with five months.Citation25
Another point of view is that, in the consideration of shorter timed corticosteroid treatment, patient will experience more frequent relapses, he would be given initial doses of corticosteroids again or if high doses of i.v. needed pulse treatment. Thus, the total cumulative doses of corticosteroids will be much more than the prior.
In group 1, 22.6% of patients had frequent relapses. About 77.2% of patients were non-relapsers and rare relapses in long-term steroid therapy ().
Recent studies experienced the various additional therapy modalities to steroid in frequent relapsers.Citation15 We used combination therapy in patients having their second episode within the first year in this group ().
On the other hand, prolonged course of glucocorticoids carries increased risk of steroid toxicity, including glucose intolerance, cushingoid features, infections, and any osteonecrosis.
In our study, we had seen any complication related to the long-term corticosteroid therapy. At the end of the study, median height Z score was found as 1.3 ± 1.5. In an ISKDC series of 521 children with nephrotic syndrome, 10 deaths were reported, resulting in a mortality rate of 1.9%.Citation31 Only one death was present in our cohort.
In conclusion by using the long-term corticosteroid treatment modality consisting of 20 weeks, we had the remission rate was 88% (106/120) at the end of four weeks, it rose to 94% (113/120) by the end of follow up period. Among the frequent relapsers, 79% of patients achieved recovery. With the support of our satisfactory results among the whole study group, long-term prednisolone treatment still remains valid.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article.
References
- Niaudet P, Boyer O. Idiopathic nephrotic syndrome in children: Clinical aspects. In: Avner ED, Harmon ED, Niaudet P, Yoshikawa N, eds. Pediatric Nephrology. 6th ed. Berlin, Heidelberg: Springer-Verlag; 2009:667–702
- Eddy AA, Symons JM. Nephrotic syndrome in childhood. Lancet. 2003;362(9384):629–639
- Cattran DC, Alexopoulos E, Heering P, et al. Cyclosporin in idiopathic glomerular disease associated with the nephrotic syndrome: Workshop recommendations. Kidney Int. 2007;72:1429–1447
- Shalhoub RJ. Pathogenesis of lipoid nephrosis – A disorder of T-cell functions. Lancet. 1974;2:556–560
- Meyrier A. Mechanisms of disease: Focal segmental glomerulosclerosis. Nat Clin Practice Nephrol. 2005;1:44–54
- Nielsen R, Christensen EI. Proteinuria and events beyond the slit. Pediatr Nephrol. 2010;25:813–822
- Korbet SM. Clinical picture and outcome of primary focal segmental glomerulosclerosis. Nephrol Dial Transplant. 1999;14(Suppl 3):68–73
- Cattran DC. Idiopathic membranous glomerulonephritis. Kidney Int. 2001;59:1983–1984
- Troyanov S, Wall CA, Miller JA; Toronto Glomerulonephritis Registry Group. Idiopathic membranous nephropathy: Definition and relevance of a partial remission. Kidney Int. 2004;66:1199–1205
- Troyanov S, Wall CA, Miller JA. Focal and segmental glomerulosclerosis: Definition and relevance of a partial remission. J Am Soc Nephrol. 2005;16:1061–1068
- McAdams AJ, Valentini RP, Welch TR. The nonspecificity of focal segmental glomerulosclerosis. The defining characteristics of primary focal glomerulosclerosis, mesangial proliferation, and minimal change. Medicine (Baltimore). 1997;76(1):42–52
- Webb NJA, Lewis MA, Iqbal J, Smart PJ, Lendon M, Postlethwaite RJ. Childhoodsteroid sensitive nephrotic syndrome: Dose the histology matter? Am J Kidney Dis. 1996;27(4):484–488
- ISKDC. The primary nephrotic syndrome in children clinical significances of histopathologic variants of minimal change. Kidney Int. 1981;20(6):765–771
- Manrique-Rodríguez S, Fernandez-Llamazares CM, Sanjurjo-Saez M. Pharmacotherapeutic review and update of idiopathic nephrotic syndrome in children. Pharm World Sci. 2010;32(3):314–321
- Beco A, Castro-Ferreira I, Coentrao L, Neto R, Sampaio S, Pestana M. Rituximab for steroid-dependent nephrotic syndrome. Clin Nephrol. 2010;74(4):308–310
- Kyrieleis HA, Levtchenko EN, Wetzels JF. Long-term outcome after cyclophosphamide treatment in children with steroid-dependent and frequently relapsing minimal changenephrotic syndrome. Am J Kidney Dis. 2007;49:592–597
- Ueda N, Chihara M, Kawaguchi S, et al. Intermittent versus long-term tapering prednisolone for initial therapy in children with idiopathic nephrotic syndrome. J Pediatr. 1988;112:122–126
- Ksiazek J, Wyszynska T. Short versus long initial prednisone treatment in steroid sensitive nephrotic syndrome in children. Acta Paediatr. 1995;84:889–93
- Ruggenenti P, Perna A, Mosconi L, et al. Urinary protein excretion rate is the best independent predictor of ESRF in non-diabetic proteinuric chronic nephropathies. ‘Gruppo Italiano di Studi Epidemiologici in Nefrologia’ (GISEN). Kidney Int. 1998;53:1209–1216
- Bonilla-Felix M, Parra C, Dajani T, et al. Changing patterns in the histopathology of idiopathic nephtotic syndrome in children. Kidney Int. 1999;55:1885–1890
- Gluati S, Sharma AP, Sharma RK, Gupta A. Changing trends of histopathology in childhood nephrotic syndrome. Am J Kidney Dis. 1999;34:646–650
- Andersen RF, Thrane N, Noergaard K, Rytter L, Jespersen B, Rittig S. Early age at debut is a predictor of steroid-dependent and frequent relapsing nephrotic syndrome. Pediatr Nephrol. 2010;25(7):1299–1304
- Hodson EM, Willis NS, Craig JC. Corticosteroid therapy for nephrotic syndrome in children. Cochrane Database Syst Rev. 2007;(4):CD001533
- Tarshish P, Tobin JN, Bernstein J, Edelmann CM Jr. Prognostic significance of the early course of minimal change nephrotic syndrome: Report of the International Study of Kidney Disease in Children. J Am Soc Nephrol. 1997;8(5):769–776
- Hodson EM, Alexander SI, Graf N. (2009) Steroid-Sensitive Nephrotic Syndrome. In: Geary DF, Schaefer F, eds. Comprehensive Pediatric Nephrology. 1st ed. Philadelphia: Mosby Elsevier; 2009:329–256
- Ehrich JH, Brodehl J. Long versus standard prednisone therapy for initial treatment of idiopathic nephrotic syndrome in children. Arbeitsgemeinschaft fur Padiatrische Nephrologie. Eur J Pediatr. 1993;152:357–361
- Nolasco F, Cameron JS, Heywood EF, et al. Adult-onset nephrotic syndrome: A long-term follow-up. Kidney Int. 1986;29:1215–1223
- Norero C, Delucchi A, Lagos E, Rosati P. Initial therapy of primary nephrotic syndrome in children: Evaluation in a period of 18 months of two prednisone treatment schedules. Chilean Cooperative Group of Study of Nephrotic Syndrome in Children. Rev Med Chil. 1996;124(5):567–572
- Bagga A, Hari P, Srivastava RN. Prolonged versus standard prednisolone therapy for initial episode of nephrotic syndrome. Pediatr Nephrol. 1999;13(9):824–827
- The primary nephrotic syndrome in children. Identification of patients with minimal change nephrotic syndrome from initial response to prednisone. A report of the International Study of Kidney Disease in Children. J Pediatr. 1981;98(4):561–564
- Wingen AM, Müller-Wiefel DE, Schärer K. Spontaneous remissions in frequently relapsing and steroid dependent idiopathic nephrotic syndrome. Clin Nephrol. 1985;23(1):35–40