Abstract
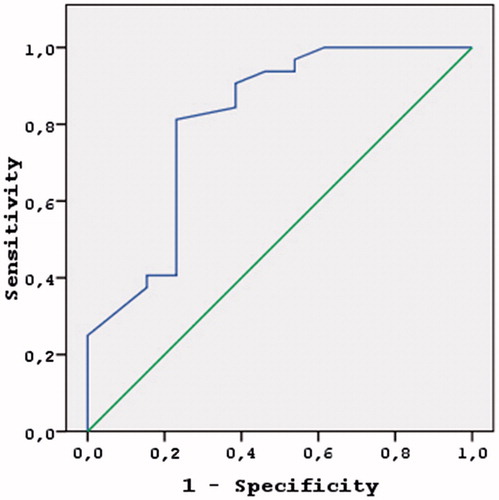
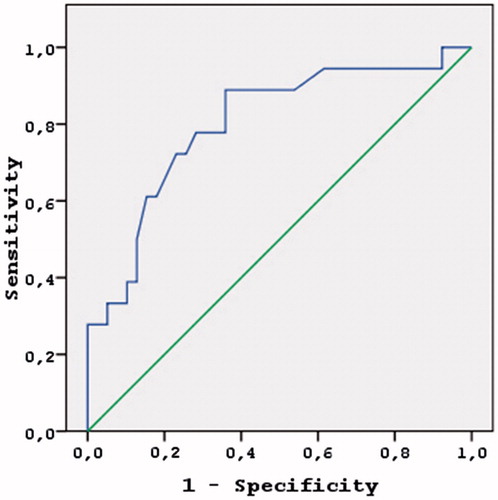
Background The living kidney donor counseling prior to the operation may be helpful to learn how to properly care for the remaining single kidney for the rest of their lives. Worsening kidney function is associated with elevated serum uric acid (UA) levels. In this study, we compared the baseline laboratory findings of renal transplant donors with their follow-up laboratory values. Methods The study consisted of 173 adult donors including 91 females and 82 males with a mean age of 46.82 ± 11.31 years. The follow-up clinical and laboratory examinations were performed on the third day at the end of the first and the sixth months of the surgery. According to donor's creatinine levels we constituted two groups: high creatinine and normal creatinine. Results Patients within the high creatinine group had significantly higher mean serum UA levels when compared with the normal creatinine group. In multivariate analysis, among the other effective variables, UA level alone was found to be the most effective parameter predicting the post-transplant creatinine levels (p = 0.004, odds ratio: 12.4, 95% CI: 2.3–68.3) at sixth month post-transplantation. In the ROC analysis for the effects of UA, the following cutoff values were found: >6 mg/dL in men (sensitivity 81.3%, specificity 76.9%, positive predictive value 89.7%, negative predictive value 62.5%, accuracy 80%) and ≥5 mg/dL in women (sensitivity 72.2, specificity 74.4%, positive predictive value 89.7%, negative predictive value 62.5%, accuracy: 73.7%). Conclusion Pretransplant serum UA levels can give important clues regarding the renal functions of the donors during the postoperative period.
Keywords:
Introduction
Due to the reduction in the deceased donor pool, living kidney donor use increases gradually during the recent years.Citation1 However, the living kidney donor pool fails to cover the requirement due to various reasons. This shortage in the living kidney donor pool mandates that the donor selection criteria be pushed to its limits.Citation2 For example, people approaching the upper age limit or lower glomerular filtration limit as well as overweight persons are sometimes selected for the donation process. Also, mildly hypertensive or glucose intolerant donors are considered to be fit. Applying the living kidney donor selection criteria within limits helps to minimize the risk for complications.Citation3 The risks and benefits both for the donor and recipient should be rigorously evaluated, and the risks should not exceed the benefits for either of them.Citation4 The follow-up controls of the donors after the transplantation procedure are not as frequent as it is for the recipients. Although donors are evaluated prior to the donation, they may be prone to renal insufficiency, hypertension, cardiovascular diseases, or diabetes postoperatively. Donors lose roughly 50% of their nephrons following the donation procedure. In studies on donors, increased creatinine values begin to subside at the end of the first week at the earliest, and in some cases it may take several months to reach normal values.Citation5 Donor counseling prior to the operation may be helpful to learn how to properly care for the remaining single kidney for the rest of their lives.
Uric acid (UA) is a product of purine metabolism and is filtered through glomeruli and then reabsorbed from the proximal tubules. This results in 70% excretion from the kidneys and the remaining 30% is excreted through the gastrointestinal tract.Citation6 Worsening kidney function is associated with elevated serum UA levels due to the impairment of UA transport through nephrons.Citation7 Elevated UA levels may also be a sign for the deterioration of glomerular filtration rate (GFR) and the emergence of a kidney disease.Citation8 Renal parenchymal lesions may be related with higher levels of UA.Citation9 UA may be associated with kidney damage through direct or indirect pathways. Endothelial dysfunction and elevated renin–angiotensin–aldosterone activity associated with higher UA levels may be directly related with the kidney damage found in hyperuricemia.Citation10
Hyperuricemia is also thought to be related with kidney impairment through indirect pathways. Microalbuminuria in Type II diabetes, untreated hypertension, and pre-hypertension are presumed to be related with serum UA levels.Citation11,Citation12 Renal functional impairment in non-proteinuric Type I diabetics is thought to be related with high-normal serum UA levels.Citation13 As a result, serum UA levels may be a predictor for renal dysfunction. The predictor value of serum UA levels in renal transplant donors is uncertain. In this study, we compared the baseline laboratory findings of renal transplant donors with their follow-up laboratory values.
Methods
This study included living renal transplantation donors during the years 2011–2015 in Baskent University's two different centers for renal transplantation. The study consisted of 173 adult donors including 91 females and 82 males with a mean age of 46.82 ± 11.31 years. Donor characteristics such as age, gender, past medical history, use of any medications, physical examination findings, and follow-up information were retrieved from the medical database of the healthcare centers. All of the subjects have undergone cardiological, respiratory, gastroenterological, dental, and psychiatric consultations. Blood urea nitrogen (BUN), creatinine, electrolytes, calcium (Ca), phosphorus (P), UA, high-sensitive C-reactive protein (hs-CRP) levels were determined by either the C8000 system (Abbott, USA) or Cobas e-411 (Roche, Germany) autoanalyzer. Urinary protein and microalbumin levels were determined, and creatinine clearance rates were calculated in all donors on a 24-h urinary specimen prior to the donation surgery. The follow-up clinical and laboratory examinations were performed on the third day at the end of the first and the sixth months of the surgery. The exclusion criteria for the donors consisted of the following: age <18 years, body mass index (BMI) >35, any use of medications for hypertension or diabetes, presence of any kidney disease, malignant or ongoing infectious diseases, cardiovascular diseases, gout, any psychiatric disorders, or elevated UA levels.
This study was conducted according to the Helsinki declaration and the study protocol was approved by the local institute's Committee on Human Research (our local ethics body). All of the subjects gave their informed consents.
Statistical analysis
Statistical analyses were carried out using SPSS (SPSS Inc. Version13.0, Chicago, IL, USA). The results were presented as means ± standard deviation for continuous variables and frequency and percent values for categorical variables. Mean values among groups were compared by either Student's T test when the distribution was normal or Mann–Whitney U test if otherwise. A logistic regression was used to identify the independent predictors of the sixth month increase in creatinine. Inclusion of variables was assessed using a forward method. The receiver operating characteristic (ROC) curve and the area under ROC (AUROC) curve analyses were used to assess the utility of parameters in the levels of UA. p-Values less than 0.05 were considered statistically significant.
Results
The demographic and laboratory values for the subjects are depicted in . An increase of 30% or more in creatinine values in any subject or a creatinine value of >1.4 in males and >1.3 in females were considered to be elevated at the end of the sixth month after surgery. These criteria classified 71.1% of male and 32.1% of female donors and an overall 49.5% of all of the donors to be in the high creatinine group. The characteristics for donors either with high or normal creatinine groups are presented in . Patients within the high creatinine group were predominantly male, had significantly higher levels of pretransplant BUN, creatinine clearance rate, and mean serum UA levels when compared with the normal creatinine group. In multivariate analysis, among the other effective variables such as age, pretransplant creatinine, BUN, creatinine clearance rate of the living donor, UA level alone was found to be the most effective parameter predicting the post-transplant creatinine levels (p = 0.004, odds ratio: 12.4, 95% CI: 2.3–68.3) at sixth month post-transplantation.
Table 1. The demographic and laboratory values for the donors.
Table 2. The characteristics for donors either with high or normal creatinine groups.
In the ROC analysis for the effects of UA, the following cutoff values were found: >6 mg/dL in men () (sensitivity 81.3%, specificity 76.9%, positive predictive value 89.7%, negative predictive value 62.5%, accuracy 80%) and ≥5 mg/dL in women () (sensitivity 72.2, specificity 74.4%, positive predictive value 89.7%, negative predictive value 62.5%, accuracy: 73.7%).
Discussion
According to our renal function impairment criteria, donors having UA levels higher than 6 mg/dL in males and 5 mg/dL in females prior to surgery pose a significantly higher risk for postoperative kidney function impairment. In donors whose creatinine values still persist at high levels at the end of the sixth month may develop chronic kidney disease (CKD) sometime later. We have not encountered any studies that investigate the predictive value of the pretransplant UA levels on the post-transplant kidney function in living donors. The studies that evaluate the predictive value of UA levels on renal function impairment mostly investigate the values of the recipients. As there are a couple of confounding factors that affect the UA levels in these studies such as cyclosporine-induced hyperuricemia, they are of limited value. In a study performed on kidney transplantation recipients by Haririan et al., higher serum UA levels were found to be associated with higher risk for graft loss and a decrease in estimated GFR.Citation14 However, Akalin et al. reported that death, graft failure, new cardiovascular events, and chronic graft nephropathy were more frequent in hyperuricemic recipients.Citation15 Bandukwala et al. demonstrated the association of hyperuricemia with the decrease in renal allograft function in their study of 405 stable renal transplant recipients.Citation16 Renal graft outcomes were found to be poorer in hyperuricemic recipients in general.
Studies on the relationship between UA levels and renal function report equivocal results. In studies performed on healthy individuals, UA levels were found to be a useful predictor during the follow-up of renal functions. Increased UA levels were found to be predictive for incipient kidney disease and end-stage renal disease in people with normal renal function as well as the progression in individuals with kidney disease.Citation17,Citation18 While Ishani et al., in their study on male subjects, report a relation between UA levelsCitation19 and end stage kidney disease, an independent association was only observed for women in another study from Japan.Citation20 Zhang et al. studied a community-based Chinese population with eGFR >60 mL/min/1.73 m2 and found UA levels to be independently associated with the likelihood for the decline in renal function.Citation21 Although, the association was not significant in the modification of diet in renal disease (MDRD) study of Madero et al.Citation22 Previous studies revealed inconsistent results, and researches among the non-hypertensive and non-diabetic population are limited. As research regarding the predictiveness of UA levels and kidney damage on the non-hypertensive and non-diabetic population is scarce in the literature, the present study has a value in itself. The present study underlines that UA levels which may be of importance during the living donor exclusion process. As the donor loses almost 50% of its nephrons instantly following the surgery, the benefits of donation must outweigh the risks associated with the procedure. The search regarding the risk factors and the clinical course regarding the development of kidney dysfunction following kidney donation is still far from being complete.Citation23 Living donor assessment prior to kidney donation aims at choosing the most suitable donor with a minimum risk of complication.Citation24 Because we are currently pushing the donor selection criteria to its limits (e.g., accepting donors with a GFR at lower limits, overweight donors, donors with glucose intolerance, elderly donors, and mildly hypertensive individuals on monotherapy) to overcome the shortage of the living donor pool, we presume that pretransplant UA values may be useful for the follow-up of the donors after surgical intervention. The literature discusses whether the increase in UA is a result or a reason for kidney function impairment. Not all of the hypertensive or diabetic individuals universally have elevated levels of UA. For instance, in the adult population, the prevalence of prehypertension and hypertension is approximately 60%, whereas prevalence of hyperuricemia (defined as UA >6.0 mg/dL in women and UA >7.0 mg/dL in men) is approximately 17%.Citation25 In such populations, UA may have an enhancing role for end-organ impairment through direct or indirect pathways. The nephrotoxic effect of elevated UA levels is supported in animal experiments and cellular biological studies. Higher UA levels leading to glomerular hypertension, elevated renal vascular resistance, reduced renal blood flow, activation of renin–angiotensin system (RAS), arteriolosclerosis, glomerular hypertrophy, glomerulosclerosis, and interstitial disease have been shown in various animal experiments. In these studies, the mentioned effects were suggested to be induced through oxidative stress and endothelial dysfunction caused by higher levels of UA.Citation26,Citation27 Nitric oxide generated in vitro in endothelial cells was found to be directly impaired by UA.Citation10 Our findings of UA levels within normal range (<7.2 mg/dL in males and <6 mg/dL in females) in the present study are of significance. In the cardiovascular health study (CHS) of Choncol et al., a strong correlation was observed between the baseline kidney function and UA levels.Citation28 Interestingly, although the presence of a strong cross-sectional association between baseline UA levels and baseline kidney function was found along with an annual decrease of ≥3 mL/min 1.73 m2 in the patients ≥65 year of age with UA levels >5.9 mg/dL in the longitudinal analysis, Choncol et al. failed to disclose any significant relationship between UA levels and incident CKD defined by eGFR <60 mL/min per 1.73 m2 in the final examination of their study results. In non-proteinuric Type I diabetic patients with normal to high levels of UA, an early decline in GFRs was reported.Citation13 Among these studies, Ficociello et al. reported a 40% increase in the odds of developing early GFR loss for every 1 mg/dL increase in serum UA level.Citation29 The presence of a relation between the UA levels and the baseline kidney function was suggested in other studies.Citation17 In a study by Gerhardt et al. including 350 kidney transplant recipients with functioning grafts one year after the procedure, UA levels greater than 8.1 mg/dL in men and 6.1 mg/dL in women were found to be associated with worsening graft survival in the following five years when compared with normouricemic graft recipients (five-year rate 68.8% vs. 83.3%, respectively).Citation30 Studies on individuals with higher levels of UA show that these people are more prone to obesity, hypertension, diabetes, and cardiovascular events when compared with normouricemic individuals.Citation31 These diseases and entities are among the factors that may affect the renal function of the living donors either directly or indirectly later on during their lives. These diseases are significant risk factors for living donors following nephron loss. In living donors with elevated UA levels, precautions about the mentioned diseases and entities may provide significant health benefits during their lives following nephron loss. There are studies that report the beneficial effects of UA-lowering dietary precautions and medications in the progress of CKD. Sturm et al. followed 177 non-diabetic CKD patients (stage I–V) for seven years looking for an association between UA levels and CKD progression and observed that UA was not predictive for CKD progression. However, when they have excluded the patients using UA-lowering drugs, the analyses revealed a faster progression of CKD with high levels of UA.Citation32 Mild or moderate renal dysfunction is present in 20–60% of patients with gout.Citation33 Before the availability of UA lowering agents, as many as 10–25% of patients with gout developed end-stage renal disease.Citation34 In living kidney donors, UA levels that approach their upper limits but are within the normal range seem to be useful to predict the postoperative elevation in the creatinine levels in the present study. This observation leads us to recommend UA-lowering drugs and precautions to be effective in living donors, in whom UA levels approach their upper limits but are within their normal range prior to the operation. This may lessen the load and hence preserve the function of the remaining kidney in the living donors following the transplantation.
Limited sample size and the shorter duration of follow-up are the limitations of the present study. Therefore, the results of this study need to be supported by further clinical trials performed on a larger sample of living donors with elevated levels of UA prior to donation procedure and with a follow-up period longer than six months.
Conclusion
Pretransplant serum UA levels can give important clues regarding the renal functions of the donors during the postoperative period.
Disclosure statement
The author reports no conflicts of interest.
References
- NHS Blood and transplant, http://organdonation.nhs.uk/statistics/transplant activity report/current activity reports/ukt/activity report 2011 12.pdf, 2013.
- O’Brien B, Mastoridis S, Sabharwal A, Hakim N, Taube D, Papalois V. Expanding the donor pool: Living donor nephrectomy in the elderly and the overweight. Transplantation. 2012;93:1158–1165.
- Akoh JA, Stacey S. Assessment of potential living kidney donors: Options for increasing donation. Dial Transplant. 2008;37:352–359.
- Abecassis M, Adams M, Adams P, et al. Consensus statement on the live organ donor. JAMA. 2000;284:2919–2926.
- Velosa JA, Offord KP, Schroeder DR. Effect of age, sex, and glomerular filtration rate on renal function outcome of living kidney donors. Transplantation. 1995;60:1618–1621.
- Ohno I. Relationship between hyperuricemia and chronic kidney disease. Nucleosides Nucleotides Nucleic Acids. 2011;30:1039–1044.
- Sica DA, Schoolwerth AC. Handling of organic anions and cations: Excretion of uric acid. In: Brenner BM, ed. The Kidney. 7th ed. Philadelphia: WB Saunders; 2004:645–649.
- Kalantar E, Khalili N, Hossieni MS, Rostami Z, Einollahi B. Hyperuricemia after renal transplantation. Transplant Proc. 2011;43:584–585.
- Bellomo G, Venanzi S, Verdura C, Saronio P, Esposit A, Timio M. Association of uric acid with change in kidney function in healthy normotensive individuals. Am J Kidney Dis. 2010;56:264–272.
- Khosla UM, Zharikov S, Finch JL, et al. Hyperuricemia induces endothelial dysfunction. Kidney Int. 2005;67:1739–1742.
- Lee JE, Kim YG, Choi YH, Huh W, Kim DJ, Oh HY. Serum uric acid is associated with microalbuminuria in prehypertension. Hypertension. 2006;47:962–967.
- Tseng CH. Correlation of uric acid and urinary albumin excretion rate in patients with type 2 diabetes mellitus in Taiwan. Kidney Int. 2005;68:796–801.
- Rosolowsky ET, Ficociello LH, Maselli NJ, et al. High-normal serum uric acid is associated with impaired glomerular filtration rate in nonproteinuric patients with type 1 diabetes. Clin J Am Soc Nephrol. 2008;3:706–713.
- Haririan A, Metireddy M, Cangro C, et al. Association of serum uric acid with graft survival after kidney transplantation: A time-varying analysis. Am J Transplant. 2011;11:1943–1950.
- Akalin E, Ganeshan SV, Winston J, Muntner P. Hyperuricemia is associated with the development of the composite outcomes of new cardiovascular events and chronic allograft nephropathy. Trans Plantation. 2008;15:652–658.
- Bandukwala F, Huang M, Zaltzman JS, Nash MM, Prasad GV. Association of uric acid with inflammation, progressive renal allograft dysfunction and post-transplant cardiovascular risk. Am J Cardiol. 2009;103:867–871.
- Iseki K, Oshiro S, Tozawa M, Iseki C, Ikemiya Y, Takishita S. Significance of hyperuricemia on the early detection of renal failure in a cohort of screened subjects. Hypertens Res. 2001;24:691–697.
- Weiner D, Tighiouart H, Elsayed EF, Griffith JL, Salem DN, Levey AS. Uric acid and incident kidney disease in the community. J Am Soc Nephrol. 2008;19:1204–1211.
- Ishani A, Grandits GA, Grimm RH, et al. Association of single measurements of dipstick proteinuria, estimated glomerular filtration rate, and hematocrit with 25-year incidence of end-stage renal disease in the multiple risk factor intervention trial. J Am Soc Nephrol. 2006;17:1444–1452.
- Iseki K, Ikemiya Y, Inoue T, Iseki C, Kinjo K, Takishita S. Significance of hyperuricemia as a risk factor for developing ESRD in a screened cohort. Am J Kidney Dis. 2004;44:642–650.
- Zhang L, Wang F, Wang X, Liu L, Wang H. The association between plasma uric acid and renal function decline in a Chinese population-based cohort. Nephrol Dial Transplant. 2012;27:1836–1839.
- Madero M, Sarnak MJ, Wang X, et al. Uric acid and long-term outcomes in CKD. Am J Kidney Dis. 2009;53:796–803.
- Kido R, Shibagaki Y, Iwadoh K, et al. How do living kidney donors develop end-stage renal disease? Am J Transplant. 2009;9:2514–2519.
- Delmonico FL, Dew MA. Living donor kidney transplantation in a global environment. Kidney Int. 2007;71:608–614.
- Sui X, Church TS, Meriwether RA, Lobelo F, Blair SN. Uric acid and the development of metabolic syndrome in women and men. Metab Clin Exp. 2008;57:845–852.
- Sanchez-Lozada LG, Tapia E, Santamaria J, et al. Mild hyperuricemia induces vasoconstriction and maintains glomerular hypertension in normal and remnant kidney rats. Kidney Int. 2005;67:237–247.
- Chonchol M, Shlipak MG, Katz R, et al. Relationship of uric acid with progression of kidney disease. Am J Kidney Dis. 2007;50:239–247.
- Gerhardt U, Grosse HM, Hohage H. Influence of hyperglycemia and hyperuricemia on long-term transplant survival in kidney transplant recipients. Clin Transplant. 1999;13:375–379.
- Johnson RJ, Kang DH, Feig D, et al. Is there a pathogenetic role for uric acid in hypertension and cardiovascular and renal disease? Hypertension. 2003;41:1183–1190.
- Sturm G, Kollerits B, Neyer U, Ritz E, Kronenberg F. Uric acid as a risk factor for progression of non-diabetic chronic kidney disease? The Mild to Moderate Kidney Disease (MMKD) Study. Exp Gerontol. 2008;43:347–352.
- Berger L, Yu T. Renal function in gout. IV. An analysis of 524 gouty subjects including long-term follow-up studies. Am J Med. 1975;59:605–613.
- Talbott JH, Terplan KL. The kidney in gout. Medicine. 1960;39:405–467.
- Mazzali M, Hughes J, Kim YG, et al. Elevated uric acid increases blood pressure in the rat by a novel crystal-independent mechanism. Hypertension. 2001;38:1101–1106.
- Ficociello LH, Rosolowsky ET, Niewczas MA, et al. High-normal serum uric acid increases risk of early progressive renal function loss in type 1 diabetes: Results of a 6-year follow-up. Diabetes Care. 2010;33:1337–1343.