Caterpillar setae are an uncommon cause of ocular trauma.Citation1 Ocular complications, such as iritis, conjunctiva or iris granulomas, vitritis,Citation2 and endophthalmitis,Citation3,Citation4 have been reported. The ocular reactions, called ophthalmia nodosa, can occur due to either the mechanical effect or the direct toxic effect of the penetrated setae.Citation2 Ophthalmia nodosa due to caterpillar hair is a common occupational disease in Eastern Mediterranean-region countries. A certain type of endemic caterpillar species has deleterious harmful effects on the growth and well being of red pine trees, which are highly populated in that region. To avoid colonization of caterpillars on these trees, biological warfare is being waged. Several caterpillar-breeding farms have been established in order to feed a particular form of parasite bug on these caterpillars. After being fed only on these caterpillars, those parasite bugs are released into forestry to get rid of these harmful caterpillars. Although this biological warfare is very popular and successful, particularly in the East Aegean region, there is a serious occupational hazard for employees who work in these breeding farms: ophthalmia nodosa. Due to lack of wearing protective equipment, knowledge, and education, 4 employees at one of these caterpillar-breeding farms on the west coast of Turkey, with ocular trauma caused by caterpillar hairs, were admitted to our hospital. In this report, we detail these cases and perform a knowledge, attitude, and practice study on those farm workers.
A 34-year-old male patient, the night watchman at a caterpillar breeding farm, presented with a 3-h history of photophobia, foreign body sensation, and pain in the left eye. At presentation, visual acuity was 20/100. Examination of the right eye showed edema of the eyelid, mucopurulent discharge, chemosis, corneal stromal edema, and an epithelial defect, identified using fluorescein staining. A closer examination of the eye using biomicroscopy revealed a number of hairs embedded in the cornea, along with a severe anterior chamber reaction (. No hairs were found in the fornices or tarsal conjunctivas. Removal of the superficial setae was performed in the operating room under local anesthesia. The setae were too tiny to remove with even the most delicate microforceps. The deep setae were removed using a 30-gauge needle (). A 40× magnification of the setae is shown in . The setae were removed three times, whenever they resurfaced. Four setae, lying deep and parallel to the corneal plane, were left in place. The corneal and conjunctival edema and the anterior chamber reaction were resolved with topical steroids, lubricants, antibiotics, and cycloplegics. Funduscopic examination revealed no setae in the retina.
FIGURE 1. The arrows show multiple embedded hairs in the cornea causing an acute toxic reaction and an epithelial defect (A). The white square shows a bubble-like anterior chamber reaction (B). The setae on a 30-gauge needle (C). 40× magnification of the setae under a microscope (D). Retained intracorneal seta tangential to the endothelial layer with surrounding congestion (E). AC-OCT imaging of the deep seta tangential to the endothelial layer (F).
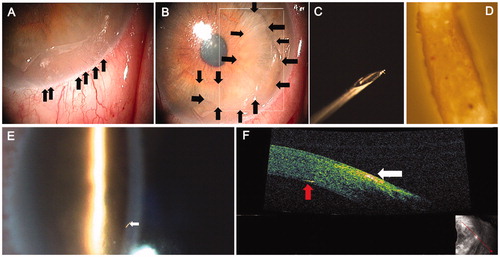
A 43-year-old male patient, a caterpillar breeder at the same company, presented with a 3-month history of itching, lacrimation, and photophobia in both eyes. He had been previously treated with anti-allergy drops for allergic conjunctivitis elsewhere. His visual acuity was 20/20. Examination of the right and left eyes showed mild conjunctival hyperemia and the presence of 1 seta in the deep cornea of the right eye with 1 tip in contact with the anterior chamber (). There were 2 setae in the deep layers of the left cornea. The tarsal and bulbar conjunctivas showed no signs of setae. The corneal epithelium was intact in both eyes. No significant anterior chamber reaction was observed and the retina was free of setae. Anterior segment optical coherence tomography (AC-OCT) was performed to localize the setae. Images showed the seta lying parallel to the endothelial plane with 1 tip touching the anterior chamber (). Due to the absence of anterior chamber reactions, the setae in the cornea were left in place, and fluorometholone drops and lubricating agents were prescribed.
A 38-year-old male patient, another caterpillar breeder at the same company, presented with a 4-month history of mild hyperemia and itching in both eyes. Examination of the right eye showed 2 setae deep in the corneal stroma and mild conjunctival hyperemia. The fluorescein staining was negative, indicating that the epithelium was intact. Funduscopic examination was unremarkable. The left eye was normal. The setae were left in place, and anti-allergy drops and lubricating agents were prescribed.
A 52-year-old male patient, also a caterpillar breeder at the same company, presented with a 1-month history of redness and itching in the right eye. He had previously received treatment but without relief. Examination of the right eye showed a tiny hair in the deep cornea. Funduscopic examination was unremarkable. The seta was left in place, and fluorometholone drops were prescribed. At reexamination, the patient’s eye was completely normal.
Granulomatous nodules found on the iris and conjunctiva are caused by vegetation or insect hairs, including tarantulas, spiders, and caterpillars and are characteristic of a well-documented condition called ophthalmia nodosa.Citation5–8 Although ophthalmia nodosa was first described in 1904 by Saemisch,Citation7 the first report of eye reactions caused by caterpillar setae was published by Schön in 1861.Citation9
Ocular toxicity due to caterpillar setae results from the presence of setae in the eye tissues, as well as released urticating toxins.Citation10–12 A classification was previously developed for ophthalmia nodosa by Cadera et al.Citation8:
Type 1. An acute toxic reaction to hair (chemosis and inflammation)
Type 2. Chronic mechanical keratoconjunctivitis caused by hair found in the bulbar or palpebral conjunctiva with foreign body sensation and corneal abrasions
Type 3. Formation of conjunctival granulomas due to subconjunctival or intracorneal setae
Type 4. Iritis secondary to hair penetration of the anterior segment
Type 5. Early or late vitreoretinal involvement due to penetration of the hair through the cornea, iris, and lens or via the transscleral route; vitritis, cystoid macular edema, papillitis, or endophthalmitis may occur
Interestingly, ophthalmia nodosa is encountered as an occupational disease in Mediterranean-region countries. Caterpillars are harmful to red pine trees. A parasitic bug (Calasoma sycopanta) is trained to eat these caterpillars in caterpillar-breeding farms. However, due to lack of proper safety precautions, caterpillars, which are kept in the farms as feed for the parasitic bugs, pose the risk of ophthalmia nodosa in our country. The results of our knowledge, attitude, and practice (KAP) study showed that most of the employees have no knowledge about effects of caterpillar on body organs. Moreover, the attitudes of the employees are not appropriate. The employee practice patterns () revealed that most of them do not wear appropriate protective equipment to avoid caterpillar hair contact with eyes, skin, and ears.
TABLE 1. Knowledge, attitude, and practice questionnaire.
Of our four patients, three had types 1 and 2, while the most recently injured patient had types 1 and 4. The majority of patients with ocular inflammation due to caterpillar setae have type 1 or 2.Citation11
Irrigation, followed by removal of the setae and the administration of topical antibiotics and steroids, is suggested for types 1 and 2. Surgical excision of the nodules under the conjunctiva is suggested for type 3. For type 4, with or without iris nodules, topical steroids along with surgical removal of the setae are suggested, while for type 5, local and/or systemic steroids or removal of the setae with vitrectomy is suggested.
Three of our patients had chronic keratoconjunctivitis, with duration of 1–4 months, caused by retained setae in the deep cornea, suggesting that the persistence of hairs may cause continued ocular inflammation. Therefore, total removal of caterpillar setae seems crucial for relieving symptoms and preventing complications. However, it is very difficult to remove the hairs in all cases due to their fragility, deep embedment, and/or accompanying corneal edema. For patients with more than one embedded hair, it may not be feasible to remove all the hairs at once. Once the superficial setae are removed, the patient should be reevaluated, as deeper setae may resurface or be reached after corneal edema subsides.
While caterpillars release a “mist of hairs” along with a bad smell as a self-defense mechanism to ward off predators, it is not always necessary to have direct contact with a caterpillar to be exposed to hairs. Setae transported by the wind may enter the eye and become deeply embedded due to the spines on each seta’s tip.Citation11,Citation13 The first patient was a night watchman and had not entered the room in which the caterpillars were kept, demonstrating that airborne setae may cause ocular symptoms ranging from itchiness to severe iridocyclitis.
The current report details the cases of four patients with type 1, 2, and/or 4 ophthalmia nodosa, all of which were an occupational disease. Our KAP study revealed that proper education and protection is of utmost importance to avoid ophthalmia nodosa. Given the fact that caterpillar-breeding farms are common in Mediterranean-region countries, ophthalmologists must be aware of this occupational disease. Moreover, ophthalmologists may play a role in the improvement of safety precautions by giving proper education to workers and local agencies. Individuals who handle caterpillars are advised to wear proper goggles to protect their eyes and a mask to prevent inhalation of the hairs.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Teske SA, Hirst LW, Gibson BH, et al. Caterpillar induced keratitis. Cornea. 1991;10:317–321
- Fraser SG, Dowd TC, Bosanquet RC. Intraocular caterpillar hairs (setae): clinical course and management. Eye. 1994;8:596–598
- Steele C, Lucas DR, Ridgway AEA. Endophthalmitis due to caterpillar setae: surgical removal and electron microscopic appearances of the setae. Br J Ophthalmol. 1984;68:284–288
- Corkey JA. Ophthalmianodosa due to caterpillar hairs. Br J Ophthalmol. 1955;39:301–306
- Hered RW, Spaulding AG, Sanitato JJ, et al. Ophthalmia nodosa caused by tarantula hairs. Ophthalmology. 1988;95:166–169
- Watts P, McPherson R, Hawksworth NR. Tarantula keratouveitis. Cornea. 2000;19:393–394
- Saemisch T. (1904). Ophthalmia nodosa. In Graefe A, Saemisch T (eds.), Handbuch der gesamten Augenheilkunde, 2nd ed. (pp 548–564). Leipzig: Engelmann
- Cadera W, Pachtman MA, Fountain JA. Ocular lesions caused by caterpillar hairs (ophthalmia nodosa). Can J Ophthalmol. 1984;19:40–44
- Schön J. (1861). Bietragezur praktische Augenheilkunde. Hamburg: Hoffman & Campe. p 183
- Sengupta S, Reddy PR, Gyatsho J, et al. Risk factors for intraocular penetration of caterpillar hair in ophthalmia nodosa: a retrospective analysis. Indian J Ophthalmol. 2010;58:540–543
- Shibui H, Kawashima H, Kamata K, et al. Vitrectomy for caterpillar seta-induced endophthalmitis. Arch Ophthalmol. 1997;115:555–556
- Bishop JW, Morton MR. Caterpillar hair induced keratoconjunctivitis. Am J Ophthalmol. 1967;64:778–779
- Pagenstecher H. Interessante Praparate von eindringer conjunctiva und dies Iris mit daransichbildendertuberkelartigen. Knotchen Berl Disch Ophthalmolqes. 1883;15:176–182