Case Report
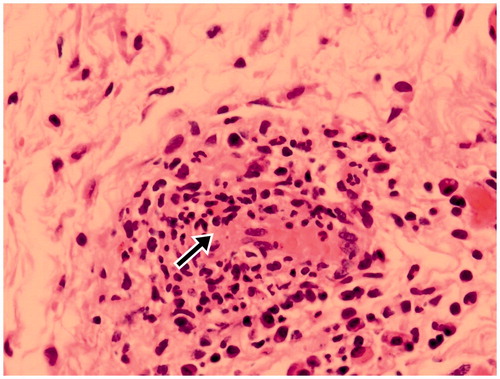
An 82-year-old man was referred by his local ophthalmologist for a 6-month history of red right eye (OD). Treatment with topical corticosteroids and antibiotics had not helped. Visual acuity at his initial visit was 20/70 (OD). Slit-lamp examination showed an injected area from 10 to 2 o’clock over the superior bulbar conjunctiva (). The lesion was pinkish and located in the subconjunctiva, without corneal involvement. There were no obvious intrinsic vessels, and a well-delineated margin was found. The remainder of the ocular examination in both eyes showed normal results (). The patient’s past medical and family histories for systemic diseases were unremarkable. He denied fatigue and weight loss recently, and there was no regional lymphadenopathy. We have performed ultrasound, but nothing in particular was found. Due to chronic conjunctivitis with a salmon patch-like lesion, lymphoma was suspected at our clinic, and the patient received excisional biopsy. We excised the conjunctiva and tenon for pathological examination, which revealed vasculitis (), without evidence of malignancy.
FIGURE 1. Slit-lamp biomicroscopy appearance of right eye (A) at presentation, and (B) 6 months after treatment. (C) Slit-lamp biomicroscopy appearance of left eye.
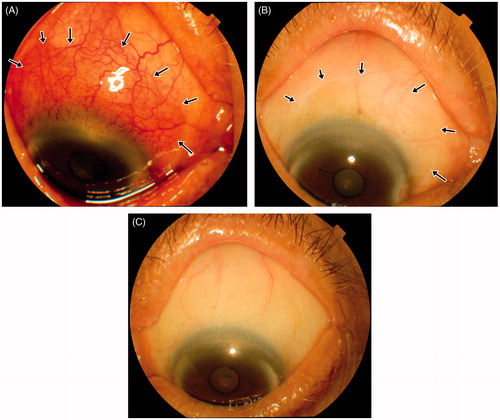
Due to intractable symptoms and conjunctival vasculitis, autoimmune profiles were checked, which revealed a high titer (1:320) of pANCA (antineutrophil cytoplasmic antibody in perinuclear pattern). The patient was referred to a rheumatologist for further survey. After thorough examination, an increased level of anti-MPO antibodies (35.0 U/mL, normal <5 U/mL) was found. Tests for the other autoantibodies, including ANCA specific for proteinase 3 (PR3-ANCA), antinuclear antibodies, and anti-glomerular basement membrane antibodies were all negative. Microscopic polyangiitis was diagnosed by a rheumatologist. Oral steroids were prescribed initially as 60 mg/day. Two weeks later, the dosage was tapered to 40 mg/day. Then the dosage was monthly tapered to 5 mg/day as maintenance dose. After prescribing oral corticosteroids, the ocular symptoms improved ().
Comment
Microscopic polyangiitis (MPA) is defined as necrotizing vasculitis primarily affecting small vessels, with few or no immune deposits.Citation1 Patients are characterized by positive antineutrophil cytoplasmic antibodies (ANCA), mainly perinuclear pattern, and particularly specific for myeloperoxidase (MPO). Systemic involvement may include the musculoskeletal, cutaneous, gastrointestinal, lung, renal, and neurological systems.Citation1 MPA is not a common disease, with an incidence rate of 3.6 cases per million in a population-based study.Citation2 Ocular involvements of MPA are even rarer. In a cohort of 85 patients with MPA, only 1 had ocular manifestations.Citation3 A MEDLINE search from 1946 to the present identified 2 case reports of MPA with ocular manifestations as initial symptoms.Citation4,Citation5 The first reported case of MPA involving the ocular area was a 23-year-old woman with renal failure and ulcerative skin.Citation6 Other reported cases of MPA with ocular involvement presented as peripheral nonulcerative keratitis and scleritis.Citation4,Citation5,Citation7–9 Retinal cotton-wool spots, which represent nerve fiber layer infarcts and microvascular diseases, have been described in MPA.Citation9 Altaie et al. also reported subacute optic neuropathy in patients with MPA.Citation10 Besides eye involvement, cutaneous findings may be presented.Citation11 In our case, the patient initially had superior bulbar conjunctiva involvement and was diagnosed as lymphoma. He did not have any systemic involvements at the beginning.
Chronic conjunctivitis is usually dry eye, infectious, and inflammatory. It is rare that MPA could lead to chronic conjunctivitis. Thus, in patients with intractable conjunctivitis, further systemic evaluation and even biopsy of the conjunctiva might be needed to establish the underlying systemic diagnosis. The prognosis of MPA is improved if the condition is recognized early and with proper treatment.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Jennette JC, Falk RJ. Small-vessel vasculitis. N Engl J Med. 1997;337:1512–1523
- Watts RA, Carruthers DM, Scott DG. Epidemiology of systemic vasculitis: changing incidence or definition? Semin Arthritis Rheum. 1995;25:28–34
- Guillevin L, Durand-Gasselin B, Cevallos R, et al. Microscopic polyangiitis: clinical and laboratory findings in eighty-five patients. Arthritis Rheum. 1999;42:421–430
- Darlington JK, Mannis MJ, Segal WA, et al. Peripheral nonulcerative keratitis as a presenting sign of microscopic polyangiitis. Cornea. 2001;20:522–524
- Hara A, Ohta S, Takata M, et al. Microscopic polyangiitis with ocular manifestations as the initial presenting sign. Am J Med Sci. 2007;334:308–310
- Caster JC, Shetlar DJ, Pappolla MA, Yee RW. Microscopic polyangiitis with ocular involvement. Arch Ophthalmol. 1996;114:346–348
- Messmer EM, Foster CS. Vasculitic peripheral ulcerative keratitis. Surv Ophthalmol. 1999;43:379–396
- Kubal AA, Perez VL. Ocular manifestations of ANCA-associated vasculitis. Rheum Dis Clin North Am. 2010;36:573–586
- Mihara M, Hayasaka S, Watanabe K, et al. Ocular manifestations in patients with microscopic polyangiitis. Eur J Ophthalmol. 2005;15:138–142
- Altaie R, Ditizio F, Fahy GT. Microscopic polyangitis presenting with sub-acute reversible optic neuropathy. Eye (Lond). 2005;19:363–365
- Kluger N, Pagnoux C, Guillevin L, et al. Comparison of cutaneous manifestations in systemic polyarteritis nodosa and microscopic polyangiitis. Br J Dermatol. 2008;159:615–620