To the editor,
I read with interest the case presented by Ercan et al. recently published in your journal [Citation1]. They presented a case of huge left atrial appendage (LAA) thrombus in a patient with atrial fibrillation (AF) that was successfully treated with the combination of acetylsalicylic acid, unfractionated heparin and tirofiban. We also initiated the same treatment (combination of acetylsalicylic acid, unfractionated heparin and tirofiban for eight day) to a similar patient with huge left atrial appendage thrombus due to atrial fibrillation. However, our treatment failed and thrombus persisted in this period. Our patient had high-risk for surgical treatment because of heart failure. Thus, we started warfarin to prevent thromboembolic complications. Thrombus completely disappeared in 6-weeks follow-up.
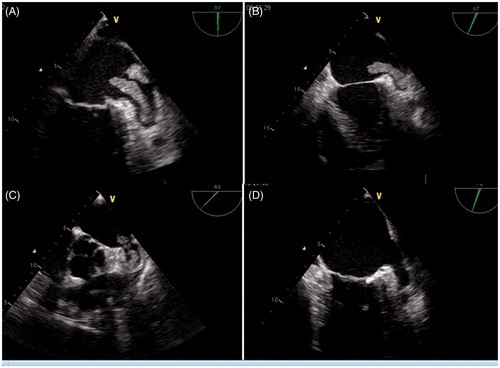
A 62-year-old male with a history of heart failure admitted to our hospital with intermittent palpitation for last two weeks. On physical examination, he had irregular pulse and electrocardiogram showed atrial fibrillation with 85 beats per minute. Echocardiography showed global hypokinesia of left ventricular walls and ejection fraction was estimated to be 30% by modified Simpson’s method. We performed transeosophagial echocardiography (TEE) to exclude any thrombus formation in LA/LAA, because we planned to restore sinus rhythm. TEE revealed a giant mobile thrombus filling LAA and protruding to left atrium (). We started acetylsalicylic acid 100 mg daily, unfractionated heparin infusion by adjusting activated clotting time to 200–250 s and tirofiban infusion 11 cc/h adjusted according to his weight. Control TEE was performed 5 days after starting treatment and we saw no change in thrombus size and shape (). We continued the treatment, but still there was no change on the trombus formation confirmed by TEE on 10th day of the treatment (). Thus, the treatment was stopped. Warfarin was initiated and the patient was discharged with warfarin after adjusting international normalized ratio value between 2.0 and 3.0. TEE showed complete lysis of the thrombus in 6-weeks follow-up ().
Figure 1. Transeosophageal echocardiography (TEE) showing a huge trombus in LA/LAA (A), TEE image is being shown after five-day treatment of acetylsalicylic acid, unfractionated heparin and tirofiban (B), there was no change in trombus size and shape on10th day of the same treatment.
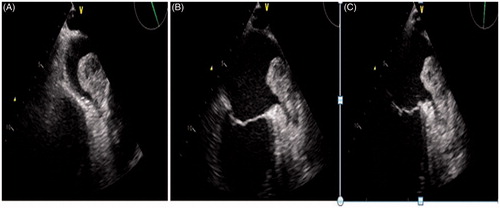
Figure 2. Transeosophageal echocardiography images performed one week intervals showing complete lysis of the giant thrombus in 6-weeks follow-up (A-D).
Incidence and prevalence of atrial AF are increasing significantly worldwied and this increase will probably impose a significant burdeb on healthcare resources. Two factors are mainly concerned in management of AF: symptom relief (through rate or rhythm control) and and prevention of complications. AF management including stroke prevention depends on multiple factors including patient age, comorbidities, and disease profile [Citation2]. Left atrial appendage (LAA) has an anatomic structure very favorable for thrombus formation in patients with AF, who often experience limited contraction and stagnant blood flow. In fact, a review of published reports reveals that 90% of cardiothrombic events in patients with AF originate from the LA/LAA [Citation2]. Many physicans want to restore sinus rhythm to improve symptoms and to protect from complications of AF. If AF duration is longer than 48 hours, TEE may be performed to rule out the presence of an intracardiac thrombus formation before cardioversion. If there is detectable thrombus in the LA/LAA, guidelines recommend warfarin for 3 weeks before and 4 weeks after cardioversion, but guidelines are not helpful when a giant thrombus is detected in LA/LAA [Citation2, Citation3]. In a case which was published in your journal, Ercan et al. reported a huge left atrial appendage thrombus in a patient with atrial fibrillation which was successfully treated with the combination of acetylsalicylic acid, unfractionated heparin and tirofiban. We also administered same treatment to a similar patient over 10 days butthis method failed and we started warfarin. TEE showed complete lysis of the thrombus after warfarin treatment in 6 weeks follow-up. Development of a giant thrombus in LA/LAA due to AF is a very rare condition. Additionally, there is no consensus on how to treat a giant thrombus with AF in guidelines. Usually, heparin infusion is not enough, thrombolysis carries high risk of embolization and surgery seems as a risky treatment for LA/LAA thrombus. Glycoprotein2b/3a inhibitors may be considered as an alternative therapy for giant thrombus in LA/LAA. To our knowledge, glycoprotein2b/3a receptor blockers have been used in patients that have undergone percutaneous coronary intervention with a lower rate of bleeding and there are two reports on the successful use of glycoprotein2b/3a inhibitors in patients with mechanical prosthetic valve thrombosis[Citation4, Citation5]. Additionally, Yuce et. al reported that tirofiban was successfully used for the treatment of atrial septal defect occluder device thrombus in a patient with heart failure [Citation6]. However, there is no sufficient evidence for glycoprotein2b/3a inhibitors in these conditions. In our view, effective anticoagulation with warfarin for at least 3 weeks is treatment of choice in these situations and the potential use of glycoprotein2b/3a inhibitors should be tested with randomized studies.
Declaration of interest
On behalf of all authors, we have no financial or industrial relationships to disclose.
References
- Ercan S, Sari I, Ozer O, Yuce M, Davutoglu V. Huge left atrial appendage thrombus in a patient with atrial fibrillation: Successful treatment with tirofiban. Platelets. 2013;24(4):333–334
- Fuster V, Rydén LE, Cannom DS, Crijns HJ, Curtis AB, Ellenbogen KA, Halperin JL, Kay GN, Le Huezey JY, Lowe JE, et al. ACCF/AHA/HRS focused updates incorporated into the ACC/AHA/ESC 2006 guidelines for the management of patients with atrial fibrillation: A report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2011;123(10):e269–e367
- Camm AJ, Kirchhof P, Lip GY, Schotten U, Savelieva I, Ernst S, Van Gelder IC, Al-Attar N, Hindricks G, Prendergast B, et al. Guidelines for the management of atrial fibrillation: The Task Force for the Management of Atrial Fibrillation of the European Society of Cardiology (ESC). Eur Heart J. 2010;31(19):2369–2429
- Yuce M, Davutoglu V, Sari I, Cakici M, Ercan S. Complete thrombus resolution with tirofiban in obstructive mechanical prosthetic mitral valve thrombosis. Platelets. 2010;21(5):386–388
- Caceres-Loriga F, Santos-Gracia J. Use of glycoprotein IIb/IIIa receptor antagonist in prosthetic valve thrombosis. Platelets. 2010;21(7):583
- Yuce M, Davutoglu V, Sari I, Ozer O. Atrial septal defect occluder device huge thrombus in patient with low ejection fraction. Echocardiography 2010;27:E96–E97
