Abstract
Background: Recently, two topical issues in total hip arthroplasty (THA) have been robot-assisted surgery and use of a short stem. The purpose of this study was to evaluate the effects of robotic milling on the accuracy of short femoral stem positioning and on the short-term clinical outcome in THA using a prospective, randomized design.
Methods: We randomized 54 patients into two groups, either robotic milling group or manual rasping group. The patients were assessed clinically and radiographically at 8 weeks, 5 months, 12 months, and 24 months.
Results: Robotic milling group had a significantly longer operation time, requiring on average 8.9 min for registration and 11.2 min for milling. On the other hand, robotic milling group showed superior results in terms of stem alignment and leg length equality. Two intraoperative femoral fractures occurred only in manual rasping group. Harris hip scores and WOMAC scores at 24 months postoperatively were similar in both groups. No complications including stem loosening, infection, nerve palsy, or dislocation were encountered in either group during the follow-up period.
Conclusions: The present study suggested that robot-assisted short stem THA could increase the accuracy of stem alignment, improve leg length equality, and help reduce the risk of intraoperative femoral fracture as compared with manual rasping. However, the clinical outcome scores did not differ between the two groups at the time of short-term follow-up. Long-term follow-up is needed to determine whether there will be a long-term clinical relevance of robot-assisted implantation of short femoral stems in THA.
Introduction
The use of a short stem is a topical issue in total hip arthroplasty (THA). Given recent interest in less invasive surgical approaches, new short stem designs have emerged and become more popular in practice.[Citation1] Short stems have potential advantages over long stems, as they are more bone conserving and thus could provide more favorable conditions for revision.[Citation2] Furthermore, the tip of a short stem does not need to extend into the diaphyseal bow of the femur, and thus, the stem can be oriented in a more flexed position in the proximal femur, which allows greater retention of the femoral neck.[Citation3] Early clinical reports on several types of short stems have been encouraging with providing less proximal stress shielding.[Citation2–6] Nonetheless, because of the absence of diaphyseal fitting, there is a potential risk of stem malalignment when a short stem is used. Furthermore, due to the small surface area for stem anchorage, there is a potential risk of stem subsidence leading to unstable fixation and the possibility of intraoperative femoral fracture.[Citation3] To address these limitations, robot-assistance could provide be a solution. The ROBODOC system (Curexo Technology Corp., Fremont, CA) was developed to provide proper cementless femoral component positioning[Citation7,Citation8]. Several studies have shown favorable short-term outcomes of robot-assisted THA with conventional cementless femoral components.[Citation9,Citation10] Recently, preclinical study has provided evidence of an improved positioning of a short femoral using the ROBODOC system.[Citation11]
The purpose of this study was to evaluate the effects of robotic milling on the accuracy of short femoral stem positioning and on the short-term clinical outcome in THA using a prospective, randomized design.
Materials and methods
From November 2011 to June 2012, a total of 54 patients scheduled for primary THA using a short femoral stem were enrolled in this prospective study, after obtaining approval from our institutional review board and written informed consent from all participating patients. Inclusion criteria for patients in this study were admitted for primary THA, between 20 and 70 years of age, and expressing willingness to participate without difficulty in returning for follow-ups. The exclusion criteria were age older than 70 years, inadequate femoral bone stock (Dorr type C), septic hip sequelae, Crowe type III or IV hip dysplasia, and fused hip. Initially, we recruited 80 patients (90 hips) requiring primary THA a short femoral stem. However, 16 patients (24 hips) were excluded after applying the exclusion criteria, and 10 patients (12 hips) refused to participate. The remaining 54 patients (54 hips) constituted the study cohort and randomly assigned to a robotic milling group or a manual rasping group using a computer-generated random number table. Both groups consisted of 27 patients (27 hips). No patient died during the minimum 2-year follow-up. Three patients (3 hips) in the robotic milling group and two patients in the manual rasping group were lost to follow-up before 2-year evaluations, leaving 24 patients (24 hips) in the robotic milling group and 25 patients (25 hips) in the manual rasping group. No significant demographic differences in terms of age, gender, body-mass index, and etiologies leading to THA were evident between patients in the two groups ().
Table 1. Comparison of demographic data between robotic milling and manual rasping groups.
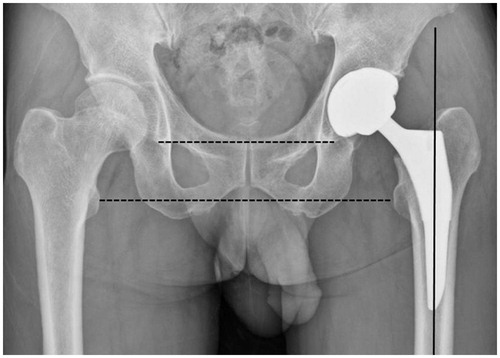
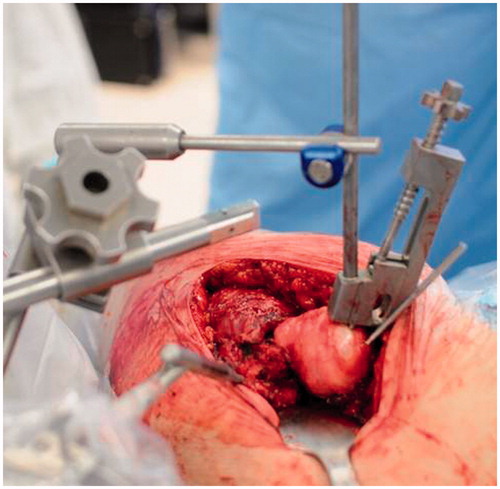
The Tri-Lock Bone Preservation Stem (DePuy/J&J, Warsaw, IN) was used in all 54 hips () and all operations were performed by one surgeon in the lateral decubitus position using a lateral positioner under general or spinal anesthesia. In the robotic milling group, a computed tomography scan was performed according to the manufacturer’s protocol (1.25-mm slice thickness; 3-mm scan interval; 200-mm field of view; less than 200 total slices). Three-dimensional (3D) preoperative planning was performed using the CT image data of each femur on the ORTHODOC workstation. Prior to each surgical procedure, patient surgical plan data were loaded into the robot system and a routine setup and diagnostic check were performed. Hip dislocation was performed prior to femoral neck cutting. In previous version of ROBODOC system, the femoral fixator clamp was attached around the femur distal to the lesser trochanter, which required wider exposure with more muscle detachment and might increase risk of the sciatic nerve injury. In this study, a new femoral fixator clamp attached to the femoral head was used to decrease soft tissue dissection and nerve injury (). Additional fixation devices were used to fix affected thighs, enable hip flexion and extension, and to minimize the effects of vibration or movement during the femoral milling procedure. Because a pinless version of the ROBODOC system was used, locater pins were not necessary. Instead, a MicroScribe 3D digitizer (Immersion Corp., San Jose, CA) was used for femoral registration. The surgeon oriented the robot by selecting points on the femoral surface using a digitizer. Registration pins were located in femoral head and trochanter, and after placing 1cm sized incisions, registration pins were additionally located in femoral anterior, lateral, and medial portions. The ROBODOC computer recorded the surface point spatial information and then compared and matched this information with a coordinate surface model created preoperatively in ORTHODOC. When registration had been completed, the surgeon verified its accuracy by touching bone surfaces with a digitizer, and if the difference between the digitization-based surface contour and the CT-derived surface contour was within 1 mm registration was accepted.[Citation12] After completing the verification process, the surgeon located the ROBODOC milling device in a suit position, and after re-checking the verification process, femoral milling was initiated. If an alteration in pin position occurred due to intraoperative vibration, the registration and verification process were repeated. After the femoral milling procedure, the ROBODOC device was removed. The remaining procedure was performed in the manner usually used for THA at our institution.
Figure 2. Intraoperative photograph showing a new femoral fixator clamp attached to the femoral head.
In the manual rasping group, hip dislocation was performed after femoral neck cutting. The femoral procedure and femur stem insertion were performed according to the manufacturer’s recommendations.
All the data were recorded and compiled by an independent observer, who had not participated in the patient clinical care and was blinded to allocation. Total operation times were noted in both groups. In the robotic milling group, registration time and milling time were also noted, respectively. Intraoperative, postoperative, and total blood losses were noted. All patients were followed prospectively with clinical evaluation at 8 weeks, 5 months, 12 months, and 24 months. The clinical outcome was measured with use of the Harris hip score[Citation13] at each visit and Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) score[Citation14] at the latest follow-up. Standard anteroposterior and cross-table lateral radiographs, which were obtained at each clinical visit, were evaluated by an independent orthopedic surgeon experienced in reviewing hip radiographs. All the measurements were performed using roentgenogram images saved on PathSpeed software (General Electric Inc., Milwaukee, WI). Stem alignment was defined as the angle between the femoral medullary axis and the femoral stem axis (the vertical axis from the stem shoulder). The perpendicular distance between a line passing through the lower edge of the tear drop points (the inter-teardrop line) or the lower edge of ischial tuberosities (the bi-ischial line) to the tip of the lesser trochanter was measured on each side and side-to-side differences were defined as leg length discrepancies. The bi-ischial line was used if tear drop deformity was severe.[Citation15] For femoral stem alignment, an outlier was defined as above varus 3° or valgus 3°, and for leg length discrepancy, an outlier was defined as >10 mm. Femoral subsidence of >4 mm, a change in the varus angle of >2°, or a complete radiolucent line was considered to indicate stem loosening.[Citation16] Complications that occurred intraoperatively or during the early postoperative period were noted.
Statistical analysis
We performed priori power calculation using a clinically relevant difference in Harris hip score of 3 points and a standard deviation of 3.65 points, with a power of 80% and a level of significance of 5%. A calculation revealed that a total of 24 patients would be needed in each group. To account for possible dropouts, we recruited about 10% more participants, leading to 27 patients in each group. The normality of the continuous data was checked with the Kolmogorov–Smirnov test. The independent-sample t test (or, when necessary, the Mann–Whitney U test) was used for continuous variables and the chi-square test (or, when necessary, Fisher’s exact test) was used for dichotomous values. p Values of <0.05 were considered significant.
Results
Total operation time in the robotic milling group was significantly longer than in the manual rasping group (p = 0.012). Average total operation times in the robotic milling and manual rasping groups were 103 min (range, 83–141) and 78 min (range, 57–147), respectively. In the robotic milling group, average registration time was 8.9 min (range, 5–15) and average milling time was 11.2 min (range, 7–20). Total blood losses in the two groups were not significantly different (p = 0.271); 1010 cc (range, 610–1800) in the robotic milling group and 895 cc (range, 410–1370) in the manual rasping group. Mean Harris hip scores at 24 months postoperatively were 93 points (range, 85–100) in the robotic milling group and 95 points (range, 89–100) in the manual rasping group, respectively. Mean WOMAC scores at 24 months postoperatively were 11 points (range, 6–17) in the robotic milling group and 12 points (range, 5–15) in the manual rasping group, respectively. No significant differences were found between the two groups with respect to the postoperative Harris hip scores and WOMAC scores (p = 0.512 and P = 0.301, respectively) ().
Table 2. Comparison of outcome data between robotic milling and manual rasping groups.
Femoral stem alignment was significantly better in the robotic milling group (p = 0.005) (). Average stem alignments in the robotic milling and manual rasping groups were 0.3° (range, 0–2.8) and 2.2° (range, 0–7.4), respectively. Leg length discrepancy was significantly smaller in the robotic milling group (p = 0.011); average leg length discrepancies in the robotic milling and manual rasping groups were 1.9 mm (range, 0–6.4) and 4.9 mm (range, 0–16), respectively. Based on the above-mentioned criteria, there were four femoral stem alignment outliers () and two leg length discrepancy outliers, and all occurred in the manual rasping group. The six femoral stem alignment outliers represented a significant intergroup difference (p = 0.022), but the two leg length discrepancy outliers did not (p = 0.235). At 24 months postoperatively, no loosening of femoral component was noted in either group. Two intraoperative femoral cracks requiring cerclage wiring occurred in the manual rasping group and none in the robotic milling group, but this did not constitute a significant intergroup difference (p = 0.490). At 24 months postoperatively, no complication, such as infection, nerve palsy, or dislocation, occurred in either group.
Discussion
The idea of using a robot in the field of orthopedic surgery, especially for THA, originated in the USA in the early 1990s. Since 1992 when the ORTHODOC system and the milling robot ROBODOC were first used on humans for THA, many reports have advocated their usefulnesses, but their usages still cause controversy.[Citation7–10] Honl et al. reported that robotic-assisted THA has advantages in terms of preoperative planning and the accuracy of the intraoperative procedure, but they also reported that this technology had a higher revision rate, a higher dislocation rate, and prolonged surgery.[Citation8] Schulz et al. reported that robotic-assisted THA with the Orthodoc/Robodoc system achieves results similar to a manual technique. However, a high number of technical complications related directly or indirectly to the robot were encountered. Technical complications directly related to the robotic device occurred in nine cases (9.3%), and included, five milling process stoppages and two femoral shaft fissures that required wire cerclage.[Citation9] However, Nakamura et al. reported that postoperative limb lengths in their robotic-milling group showed significantly less variance than a hand-rasping group. Furthermore, at 2 years postoperatively, significantly more stress shielding of the proximal femur was observed in the hand-rasping group, and this became more significant at 5 years postoperatively.[Citation10] Despite the several reports on robotic-assisted THA, no clinical report has been issued on the recently popularized use of a short stem and only one preclinical study has provided evidence of an improved positioning of a short femoral using the ROBODOC system.[Citation11] In the present prospective randomized study, we focused on two topical issues, namely, robotic milling and the use of a short stem, based on the assumption that robotic-assisted implantation of a short stem would increase the accuracy of femoral component positioning. We found that robotic milling using the ROBODOC system had advantages in terms of the accuracy of femoral stem alignment and leg length equality and that it probably reduced the risk of intraoperative femoral fracture, which corroborates the findings of Nakamura et al.[Citation10] A potential disadvantage of robot-assisted THA may be the additional time required for surgery. In our study, we observed that total operation time in the robotic milling group was significantly greater than in the manual rasping group. This time difference was caused by an average registration time of 8.9 min (5–15 min) and an average milling time of 11.2 min (7–20 min) in the robotic group. Despite this significantly longer operation time, total blood loss was not significant different in the two study groups. However, in the current study, the short-term clinical outcomes, which were evaluated by Harris hip scores and WOMAC scores at 24 months postoperatively, did not differ statistically between the robotic milling and manual rasping groups.
The major limitation of the present study is that the follow-up period was too short, which prevents our drawing conclusions about long-term performance. The relatively small study size is also a limitation. Despite these limitations, we believe that the findings of the present study are of value, because, to the authors’ best knowledge, this is the first prospective randomized study that investigates the effects of robotic milling on the accuracy of short stem positioning and on the short-term clinical outcomes.
Our data suggested that robotic milling for short stem THA could increase the accuracy of femoral component alignment and leg length equality significantly and to reduce the risk of femoral fracture associated with femoral stem insertion marginally. However, the duration of follow-up was short and we can draw no conclusions about the advantage of utilizing a robotic surgical system in short stem THA with regard to long-term outcomes.
Declaration of interest
One of the authors has received funding in support of this research from Curexo Technology Corporation, Fremont, CA, USA.
References
- Rometsch E, Bos PK, Koes BW. Survival of short hip stems with a “modern”, trochanter-sparing design – a systematic literature review. Hip Int 2012;22:344–354.
- Kim YH, Kim JS, Joo JH, Park JW. A prospective short-term outcome study of a short metaphyseal fitting total hip arthroplasty. J Arthroplasty 2012;27:88–94.
- Gustke K. Short stems for total hip arthroplasty: initial experience with the Fitmore stem. J Bone Joint Surg Br 2012;94:47–51.
- Molli RG, Lombardi AV Jr, Berend KR, . A short tapered stem reduces intraoperative complications in primary total hip arthroplasty. Clin Orthop Relat Res 2012;470:450–461.
- Bieger R, Ignatius A, Decking R, . Primary stability and strain distribution of cementless hip stems as a function of implant design. Clin Biomech (Bristol, Avon) 2012;279:158–164.
- Ettinger M, Ettinger P, Lerch M, . The NANOS short stem in total hip arthroplasty: a mid term follow-up. Hip Int 2011;21:583–586.
- Cleary K, Nguyen C. State of the art in surgical robotics: clinical applications and technology challenges. Comput Aided Surg 2001;6:312–328.
- Honl M, Dierk O, Gauck C, . Comparison of robotic-assisted and manual implantation of a primary total hip replacement. A prospective study. J Bone Joint Surg Am 2003;85:1470–1478.
- Schulz AP, Seide K, Queitsch C, . Results of total hip replacement using the Robodoc surgical assistant system: clinical outcome and evaluation of complications for 97 procedures. Int J Med Robot 2007;3:301–306.
- Nakamura N, Sugano N, Nishii T, . A comparison between robotic-assisted and manual implantation of cementless total hip arthroplasty. Clin Orthop Relat Res 2010;468:1072–1081.
- Lim SJ, Kim SM, Lim BH, . Comparison of manual rasping and robotic milling for short metaphyseal-fitting stem implantation in total hip arthroplasty: a cadaveric study. Comput Aided Surg. 2013;18:33–40.
- Nakamura N, Sugano N, Nishii T, . Robot-assisted primary cementless total hip arthroplasty using surface registration techniques: a short-term clinical report. Int J Comput Assist Radiol Surg 2009;4:157–162.
- Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am 1969;51:737–755.
- Bellamy N, Buchanan WW, Goldsmith CH, . Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol 1988;15:1833–1840.
- Kjellberg M, Al-Amiry B, Englund E, . Measurement of leg length discrepancy after total hip arthroplasty. The reliability of a plain radiographic method compared to CT-scanogram. Skeletal Radiol 2012;41:187–191.
- Kido K, Fujioka M, Takahashi K, . Short-term results of the S-ROM-A femoral prosthesis operative strategies for Asian patients with osteoarthritis. J Arthroplasty 2009;24:1193–1199.