Abstract
Aims: Analyze the capacity of ICO, the ratio of waist circumference (WC) and height, in predicting hemodynamic impairment in Erectile Dysfunction (ED) patients, independently and integrated in Metabolic Syndrome (MetS) definitions.
Methods: Four hundred and eighty-five ED patients followed in Urology consult from January 2008 until March 2012 were evaluated by a standardized protocol: health questionnaire, anthropometric measurements (AM), blood pressure and analysis, and Penile Duplex Doppler Ultrasound (PDDU) exam. Associations between AM and MetS definitions, including ATPIII, IDF and a new definition replacing WC by ICO in ATPIII MetS definition (ModATPIII), and PDDU were calculated.
Results: ICO was the measure of obesity more strongly correlated with diminished mean Peak Systolic Velocity (mPSV) (r = −0.189, p < 0.001). A positive association remained when replacing WC by ICO ≥ 0.60 (a nationally obtained ratio) in ATPIII MetS definition (ModATPIII). Patients with ModATPIII had lower mPSV when compared to non-MetS patients (30.8 versus 37.1, p < 0.001). Only the IDF definition had a significant association with AD (OR = 1853; 95%CI, 1.202–2.857).
Conclusions: ICO revealed potential value to predict PDDU changes in a MetS context. However, IDF definition presented a stronger correlation with arteriogenic ED. Although longitudinal studies are necessary to confirm this hypothesis, our study highlights the importance of different MetS definitions for ED assessment.
Introduction
Erectile dysfunction (ED) is the consistent or recurrent inability of a man to attain and/or maintain a penile erection sufficient for sexual performance [Citation1]. Being mostly vasculogenic in nature, mainly due to aging or underlying comorbidity, ED can be seen as a clinical manifestation of a functional or structural abnormality that affects penile circulation and that is part of a more generalized vascular dysfunction [Citation2,Citation3]. This underlying concept is illustrated by a positive association of ED with Metabolic Syndrome (MetS), which has been shown to triple its risk [Citation3–5].
The MetS, present in 27.5% of the Portuguese population [Citation6], is defined as a set of cardiovascular risk factors such as obesity, insulin resistance, high blood pressure (HBP) and dyslipidemia, and can be seen as a low-grade chronic inflammatory state that leads to endothelial dysfunction and, in a sexual medicine context, hypogonadism [Citation5]. Many definitions exist for it, National Cholesterol Education Program – Adult Treatment Panel III (ATPIII) and International Diabetes Federation (IDF) being the most used ones, with ATPIII having a reported superior correlation with penile blood flow impairment, low testosterone and cardiovascular events [Citation5,Citation7]. Therefore, it has received worldwide appraisal for its utility as a screening tool in patients with risk for events of cardiovascular nature [Citation8,Citation9].
From all the components of MetS, obesity (measured by bioimpedance) and HBP are the ones that are independently associated with a deterioration of the hemodynamic profile in Penile Duplex Doppler Ultrasound (PDDU) measurements [Citation10]. Although visceral obesity is known to play a primordial role in the pathophysiology of MetS and ED, it is also the center of some dispute concerning its overvaluation in MetS definitions [Citation5]. This way, having none of the actual MetS definitions considered to take visceral obesity properly into account, many new measures have been proposed for its evaluation, Index of Central Obesity (ICO) being one of the most acclaimed, as it has been shown to supplant the limitations of the traditionally used Waist Circumference (WC), namely by not neglecting height variation in subjects [Citation11,Citation12]. This anthropometric measure can be defined as the ratio of waist circumference and height [Citation12].
The correlation of ICO with ED, specifically with hemodynamic changes in vasculogenic ED, has not yet been tested. Thus, this study aims to analyze the association of ICO to hemodynamic impairment in patients with ED, either independently, or integrated in the more commonly used MetS definitions.
Patients and methods
This study is of transversal, descriptive and analytical nature. The sample includes patients followed in our Urology consult for ED (n = 485) from January 2008 until March 2012, date of the start of the analysis. Signed informed consent on the inclusion of their data in this study was obtained for all patients. Exclusion criteria were the presence of any of the following conditions: history of recent coronary artery disease, neurological disease, pelvic trauma, major psychiatric disorder, thyroid disease, hepatic disease, end-stage renal disease and history of drug abuse.
All patients were submitted to a standardized evaluation protocol that included a health questionnaire, physical examination, blood analysis and PDDU exam. The Health questionnaire contemplated past medical history, cardiovascular and metabolic risk factors such as High Blood Pressure (HBP), Diabetes mellitus and Total cholesterol (TCho), Low-Density Lipoprotein (LDL), Triglycerides (TG) and/or High-Density Lipoprotein (HDL) abnormalities. Pharmacological history was also collected, along with alcohol and tobacco use. Physical examination was performed by the same technician and with patients barefoot and with light clothing. It contemplated systolic and diastolic blood pressure evaluation and the recording of the anthropometric parameters weight, height and WC. WC measurement was obtained using an anthropometric tape (to the nearest 0.1 cm) at the end of normal expiration at the level of the midpoint between the lower end of the 12th rib and upper end of iliac crest. Body Mass Index (BMI) was calculated by dividing the weight in kilograms by the square of the height in meters, and ICO by dividing WC by height, both in centimeters.
The systolic and diastolic blood pressures were measured in the right arm using an automatic manometer (DINAMAP® Procare 300, GE, UK) in the sitting position after a 10-min rest period. HBP was defined as present if arterial blood pressure was equal or over 130/85 mmHg.
Blood analysis was performed from samples of venous blood collected between 8 and 10 am after a 12-h overnight fasting period, and the following measurements were made by routine laboratory methods: blood glucose, HDL, LDL, TG, TCho. Patients were then classified according to three MetS definitions: ATPIII, IDF and a Modified ATP III (ModATPIII) definition. Presence of MetS according to ATPIII was considered if three or more of the following five conditions were present: WC > 102 cm; TG > 1.7 mmol/L (150 mg/dL) or anti-hypertriglyceridemic medication; HDL < 1.03 mmol/L (40 mg/dL) or HDL-directed medication; plasma glucose ≥ 6.1 mmol/L (110 mg/dL); arterial blood pressure ≥130/85 mmHg or treatment for previously diagnosed HBP [Citation13]. MetS according to IDF was considered if central obesity (WC > 94 cm or BMI ≥ 30 Kg/m2) was present along with two of the following four conditions: TG > 1.7 mmol/L or anti-hypertriglyceridemic medication; HDL < 1.03 mmol/L or HDL-directed medication; plasma glucose > 5.6 mmol/L (100 mg/dL); systolic blood pressure ≥130 mmHg or Diastolic blood pressure ≥85 mmHg or treatment for previously diagnosed HBP [Citation14]. MetS, according to our ModATP III, was derived from ATPIII definition by substitution of the criterion WC > 102 cm for ICO ≥ 0.60. ICO was calculated using the formula ICO = WC (cm)/Height (cm), and the adopted cut-off of ≥0.60 was based on National Portuguese ICO values provided by Portuguese Society of Cardiology, based on a near 17 000 individual representative anthropometric nationwide study [Citation15].
PDDU examination was performed by the same investigator using the protocol suggested by the International Society for Sexual Medicine Standards Committee in Standard Practice in Sexual Medicine [Citation1]. A 12 MHz transducer (GE Logic 7 Ultrasound System, UK) was used to record penile vascular flow patterns 5, 10 and 20 min after the injection of 10 to 20 mcg of commercial E1 Prostaglandin (Caverject®). Before and in-between evaluations, patients were left alone to prevent disturbances and consequent loss of sexual arousal, and asked to maintain the best possible erection by tactile stimulation. The mean values of Peak Systolic Velocity (mPSV), End-Diastolic Velocity (mEDV) and Resistive Index (RI) (accordingly to the formula: RI = (PSV-EDV)/PSV) were obtained from spectral waveform measurements. The classification criteria were the following: normal for mPSV > 35 cm/s, EDV < 5 cm/s and RI > 1; arterial insufficiency for mPSV ≤ 35 cm/s; mPSV asymmetry for an asymmetry in mPSV > 10 cm/s; cavernous venous-occlusive disease for mPSV ≥ 35 cm/s and EDV ≥ 5 cm/s; mixed when 35 > PSV > 25 cm/s and EDV ≥ 5 cm/s. Finally, the degree of erectile response was classified according to a graded scale: 0 (no response); 1 (minimal tumescence and no rigidity); 2 (moderate tumescence and no rigidity); 3 (full tumescence and moderate rigidity); 4 (full rigidity).
Statistical analysis
The differences between the groups were assessed by unpaired Student’s t-test or Mann–Whitney U-test as appropriate for continuous variables. Multivariate analysis was performed by multivariate linear regression and multivariate logistic regression for continuous and categorical-dependent variables, respectively. Odds ratio (OR) with respective 95% confidence intervals (95% CI) were calculated to evaluate the association of categorical variables. Pearson correlation was performed to evaluate the association between continuous variables. Statistical analysis was performed using SPSS® version 17.0 for Windows® (SPSS Inc., Chicago, IL). The software handled missing data automatically: frequencies and cross-tabulations were computed based only in cases with non-missing data; correlations and regressions were computed based on pairs with non-missing data. Statistical significance was considered at p level <0.05.
Results
The population in study (n = 485) had a mean age of 55.8 ± 11.1 years, mean weight of 79.9 ± 13.3 kg and a mean height of 1.7 ± 0.1 m (mean BMI of 27.7 ± 4.2 kg/m2). Mean ICO and WC were of 0.60 ± 0.07 and 101.9 ± 10.6 cm, respectively. More data about the participants are presented in .
Table 1. Description of the population in study.
PDDU was normal in 30.8% of patients. Arterial Dysfunction (AD), veno-occlusive dysfunction, arterial dysfunction by cavernous arteries asymmetry and mixed dysfunction were identified in 41.0%, 14.7%, 7.7% and 5.8% of patients, respectively. MetS, according to ATPIII criteria, was identified in 31.1% of the population, 48.4% of it having AD diagnosed with PDDU. On the other hand, IDF MetS criteria were identified in 46.5% of patients, 49.7% of them having AD diagnosed with PDDU. Finally, using ModATP III, the prevalence of MetS was of 32.4%, 49.2% of these having AD diagnosed with PDDU. The agreement (overlap) between MetS definitions was calculated, and the results are presented in .
Table 2. Rate of concordance between different MetS definitions.
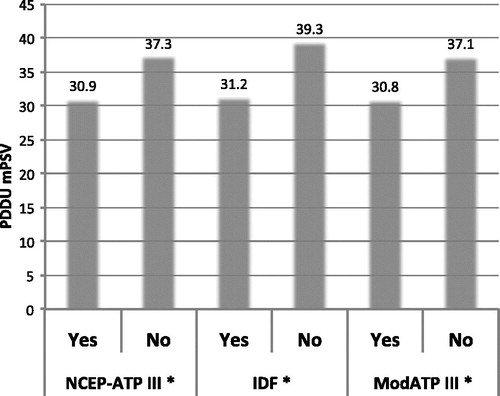
Patients with ATPIII and IDF MetS criteria had significantly lower mPSV comparatively to non-MetS patients (30.9 versus 37.3 cm/s, p < 0.001; 31.2 versus 39.3 cm/s, p < 0.001, respectively). Similarly, patients with ModATP III MetS criteria had significantly lower mPSV when compared to non-MetS patients (30.8 versus 37.1, p < 0.001) (). For this analysis, out of a total 485 patients 409, 351 and 379, respectively, had the complete necessary data. None of the three MetS definitions showed association with mean Peak Diastolic Velocity or RI changes on PDDU (data not shown).
Figure 1. Penile Doppler Duplex Ultrasound mean Peak Systolic Velocity with/without diagnosis of Metabolic Syndrome using different definitions. *p < 0.001 NCEP-ATP III, National Cholesterol Education Program - Adult Treatment Panel III; ModATP III, Modified definition of National Cholesterol Education Program - Adult Treatment Panel III; IDF, International Diabetes Federation; PDDU mPSV, Penile Duplex Doppler Ultrasound mean Peak Systolic Velocity.
Multivariate analysis including the variables High Blood Pressure (HBP), Hypertriglyceridemia (HTG) (serum level of TG > 1.7 mmol/L/150 mg/dl), fasting glucose > 5.6 mmol/L (100 mg/dL), HDL < 1.03 mmol/L, BMI ≥ 30 Kg/m2 and Waist Circumference (WC) > 94 cm showed that only HBP was independently associated with diminished mPSV on PDDU examination (p = 0.005) ().
Table 3. Multivariate analysis to evaluate the independent association of the Metabolic Syndrome criteria to a diminished mean Peak Systolic Velocity (mPSV) on Penile Doppler Duplex Ultrasound (PDDU) examination.
In another model where ICO substituted for BMI, ICO and WC were also found to be independently associated with diminished mPSV on PDDU examination (p = 0.017 and p = 0.046, respectively) ().
ICO, when compared to WC, was found to be the measure of obesity more strongly correlated with diminished mPSV on PDDU (r = −0.189, p < 0.001 versus r = −0.147, p = 0.003, respectively; 79 patients excluded for incomplete data).
An ICO over the established cut-off of 0.60 was found in 51.9% of patients. Of these, 46.0% had AD on Doppler measurements. The calculated Odds Ratio (OR) for having AD in PDDU when having ICO ≥ 0.60 was of 1.471 (95% CI: 0.986–2.194; 83 patients excluded for incomplete data). The different MetS definitions (ATPIII, IDF and ModATPIII) were all found to be independent predictors of diminished mPSV in PDDU measurements (p = 0.007 and β Standardized Coefficient = −0.140; p = 0.002 and β Standardized Coefficient = −0.182, p = 0.008 and β Standardized Coefficient = −0.140, respectively) after adjustment to age, tobacco use and TCho. Again, no association was found regarding End Diastolic Velocity or RI alterations in this multivariate analysis.
When comparing the three definitions in their correlation with AD in PDDU, IDF was found to have the only statistically significant OR (1853; 95% CI: 1.202–2.857). MetS ATPIII and ModATP III presented OR of, respectively, 1.507 (95% CI: 0.983–2.310) and 1.534 (95% CI: 0.992–2.374). Excluded due to incomplete data were, respectively, 139, 82 and 108 patients.
Discussion
Due to the existence of several MetS definitions, their specificity, sensitivity and prediction capability of different pathological outcomes have been widely and thoroughly studied, but their clinical impact is still controversial. In the particular setting of vasculogenic ED, different definitions have been studied, and ATPIII has been found to have the strongest correlation with diminished mPSV in PDDU measurements [Citation7]. In our study, such conclusion was not verified as ATP III, IDF and ModATP III definitions were all found to be positively correlated with diminished mPSV after adjustment for confounding factors. However, from the three definitions, IDF was the one that showed a stronger independent association with mPSV and the only one to show a statistically significant association with AD.
The IDF’s superior correlation with Arteriogenic ED, although not consistent with the findings of Corona and colleagues, corroborates the results of other studies that show a superior correlation of IDF with pathological cardiovascular alterations such as carotid atherosclerosis and arterial stiffness [Citation7,Citation16,Citation17]. Thus, these results constitute an upgrade on the already polemical comparison between MetS definitions, where studies repeatedly show conflicting results.
Although visceral subtype of obesity has been shown to be the one that mostly determines the deleterious effects of MetS such as ED, the most used MetS definitions (ATPIII and IDF) do not evaluate it properly and also disregard interindividual anthropometric variations such as height [Citation11,Citation12,Citation18,Citation19]. Different anthropometric parameters of visceral obesity have been analyzed in the context of ED, although few studies have been done to test these parameters in the specific setting of hemodynamic alterations in PDDU [Citation18]. In fact, Riedner and colleagues have found that from a series of anthropometric indicators of visceral obesity, only WC > 102 cm was found to be the strong predictor of ED [Citation18]. However, when evaluating the predictive value of hemodynamic changes in PDDU, WC > 102 cm failed to show such an independent association [Citation10]. This way, although WC is the visceral obesity measure most used in clinical practice and in the definitions of MetS, its limitations in evaluating short-stature individuals suggest that it may also not be the more appropriate or predictive measure when evaluating penile hemodynamic changes in ED patients [Citation7,Citation12,Citation20]. ICO, a nouvelle anthropometric measure, has been proposed not only as a more accurate measure in the evaluation of central obesity but also as a more accurate substitute of WC in MetS definitions [Citation8]. Although having been positively correlated with insulin resistance and hypogonadism, no studies have been done so far to test its utility in ED.
In this study, we have found that ICO (with a cut-off of 0.60 defined by the national median) was correlated with diminished mPSV in PDDU measurements, but the same has been found for WC and BMI, although with less significant results. In a statistical model including factors such as HBP, HTG, HDL levels, WC, ICO and insulin resistance, only HBP and the anthropometric parameters ICO and WC > 94 cm have been shown to be independently associated with a diminished mPSV on PDDU measurements. ICO over 0.60 represented a 47% chance of detecting hemodynamic changes in PDDU exam in patients with diagnosed ED.
Such results corroborate the findings of Tomada and colleagues that highlight HBP as an important factor for the deterioration of penile hemodynamics in patients with ED [Citation10]. Indeed, HBP is thought to contribute to ED by inducing local and widespread endothelial damage, thus impairing the vasodilation capability of the vasculature [Citation21,Citation22].
However, our data also highlight the positive correlation of hemodynamic alterations in ED with an anthropometric parameter. Contrarily to previous findings, WC was found to be independently associated with diminished mPSV, which can be partly explained by the use of a lower cut-off (94 versus 102 cm). Because central obesity parameters have been positively linked to HBP, this might be one of many possible paths through which central obesity relates to ED. In this setting, ICO has shown to be better correlated with HBP when compared to central obesity parameters such as WC and BMI [Citation23,Citation24].
Despite such positive association, one must point out that the sole nature of an anthropometric parameter makes this correlation liable to potential confounding factors, such as morphologic differences between individuals.
Although both WC and ICO correlated positively with penile AD, ICO revealed to be more strongly associated with diminished mPSV on PDDU. Bearing in mind the positive associations of ICO with penile hemodynamic changes, our study suggests that ICO might be more appropriate than the traditional WC in predicting hemodynamic changes when evaluating patients with ED. This finding is especially useful in populations in which there is a higher prevalence of individuals of short stature, who are especially prone to adverse cardiovascular events and whose central obesity is not correctly evaluated by WC [Citation19,Citation25]. This is also valid in the elderly population, in which there is a decrease of height with age. ICO also outstands WC on the strength of correlation with insulin resistance, while simultaneously maintaining its simplicity of calculation [Citation8].
The transversal nature of this study and the fact that the study only included patients with ED does not allow us to state that ICO is a predictive measure of ED. Indeed, although it is proposed as a more accurate measure of visceral obesity, further representative longitudinal studies comparing the different visceral obesity measures are necessary to clarify this question [Citation12].
Concerning the adopted ICO cut-off value, it is possible to observe that our study's median ICO and national-based ICO are similar (0.60), both globally and within the 50–59 age group (in which this study’s median age is included). Although the national ICO was obtained from a statistically representative nationwide population, it is not completely correct to present it as a national cut-off as it was obtained from a primary health-care seeking population. Thus, it might be an overestimation of national values, and hence its proximity to our ED population’s ICO. This cut-off seeking limitation is one of the principal difficulties of ICO usage, as pointed out by Parikh and colleagues [Citation12]. Despite this limitation concerning ICO’s cut-off value, it is clear that when analyzed as a continuous variable it has an important correlation with mPSV.
In conclusion, ICO has been shown to be the measure of obesity more strongly correlated with hemodynamic changes in Penile Doppler Measurements. Its integration in the traditional MetS definitions has also been shown to be associated with penile hemodynamic changes in an ED setting.
Despite such association, the integration of ICO in the MetS definition has not been found to increase the prediction capability of Penile Hemodynamic results compared to the traditional MetS definitions. Other studies are necessary to confirm these findings.
Declaration of interest
The authors report no declarations of interest.
Acknowledgements
The authors thank the Portuguese Society of Cardiology (SPC) for providing anthropometric data of the Portuguese population.
References
- Porst H, Buvat J. Standard practice in sexual medicine. Oxford: Blackwell Publishers; 2006:149–57
- McKinlay JB. The worldwide prevalence and epidemiology of erectile dysfunction. Int J Impot Res 2000;12:S6–11
- Demir O, Demir T, Kefi A, et al. Penile vascular impairment in erectile dysfunction patients with metabolic syndrome: penile doppler ultrasound findings. Urol Int 2009;82:175–8
- Koca O, Çalişkan S, Öatürk MI, et al. Vasculogenic erectile dysfunction and metabolic syndrome. J Sex Med 2010;7:3997–4002
- Corona G, Mannucci E, Forti G, Maggi M. Hypogonadism, ED, metabolic syndrome and obesity: a pathological link supporting cardiovascular diseases. Int J Androl 2009;32:587–98
- Fiuza M, Cortez-Dias N, Martins S. Síndrome Metabólica em Portugal: Prevalência e Implicações no Risco Cardiovascular – Resultados do Estudo VALSIM. Rev Port Cardiol 2008;27:1531–7
- Corona G, Mannucci E, Petrone L, et al. A comparison of NCEP-ATPIII and IDF metabolic syndrome definitions with relation to metabolic syndrome-associated sexual dysfunction. J Sex Med 2007;4:789–96
- Parikh R, Mohan V, Joshi S. Should waist circumference be replaced by index of central obesity (ICO) in definition of metabolic syndrome? Diabetes Metab Res Rev 2012;28:3–5
- Grundy SM. Metabolic syndrome pandemic. Arterioscler Thromb Vasc Biol 2008;28:629–36
- Tomada N, Tomada I, Botelho F, et al. Are all metabolic syndrome components responsible for penile hemodynamics impairment in patients with erectile dysfunction? The role of body fat mass assessment. J Sex Med 2011;8:831–9
- Kishida K, Funahashi T, Matsuzawa Y, Shimomura I. Visceral adiposity as a target for the management of the metabolic syndrome. Ann Med 2012;44:233–41
- Parikh RM, Joshi SR, Pandia K. Index of central obesity is better than waist circumference in defining metabolic syndrome. Metab Syndr Relat Disord 2009;7:525–7
- National Cholesterol Education Program (NCEP) Expert Panel. Third report of the expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (ATP III Final Report). Bethesda, MD: NHLBI publications; 2002;II-1–II-60
- K Alberti, P Zimmet, J Shaw. Metabolic syndrome – a new world-wide definition. A consensus statement from the International Diabetes Federation. Diabet Med 2006;23:469–80
- Cortez-Dias N, Martins S, Belo A. Prevalencia e padroes de tratamento da hipertensao arterial nos cuidados de saúde primarios em Portugal. Resultados do Estudo VALSIM. Rev Port Cardiol 2009;25:499–523
- Ma WY, Li HY, Hung CS, et al. Metabolic syndrome defined by IDF and AHA/NHLBI correlates better to carotid intima-media thickness than that defined by NCEP ATP III and WHO. Diabetes Res Clin Pract 2009;85:335–41
- Levisianou D, Melidonis A, Adamopoulou E, et al. Impact of the metabolic syndrome and its components combinations on arterial stiffness in Type 2 diabetic men. Int Angiol 2009;28:490–5
- Riedner CE, Rhoden EL, Ribeiro EP, Fuchs SC. Central obesity is an independent predictor of erectile dysfunction in older men. J Urol 2006;176:1519–23
- Parikh RM, Joshi SR, Menon PS, Shah NS. Index of central obesity – a novel parameter. Med Hypotheses 2007;68:1272–5
- Grundy SM, Cleeman JI, Merz CN, et al. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. Circulation 2004;110:227–39
- Jackson G, Montorsi P, Adams MA, et al. Cardiovascular aspects of sexual medicine. J Sex Med 2010;7:1608–26
- Brunner H, Cockcroft JR, Deanfield J, et al. Endothelial function and dysfunction. Part II: association with cardiovascular risk factors and diseases. A statement by the Working Group on Endothelins and Endothelial Factors of the European Society of Hypertension. J Hypertens 2005;23:233–46
- Lee CMY, Huxley RR, Wildman RP, Woodward M. Indices of abdominal obesity are better discriminators of cardiovascular risk factors than BMI: a meta-analysis. Journal of clinical epidemiology 2007;61:646–53
- Hongyan W, Chen L, Zhang H, Suping Z. Associations of waist to height ratio and hypertension among non-obese person. J Clin Cardiol 2007;10:007
- Siavash M, Sadeghi M, Salarifar F, et al. Comparison of body mass index and waist/height ratio in predicting definite coronary artery disease. Ann Nutr Metab 2008;53:162–6
Notice of Correction
The version of this article published online ahead of print on 18 July 2013 contained an error on page 1. The second author was incorrectly listed as “I. N. Campos Costa” and should have been “I. M. Campos Costa”. Furthermore, affiliation 1 is not the “Department of Urology” but the “Faculty of Medicine of Universidade do Porto”. These errors have been corrected for this version.