Abstract
We aimed to investigate the predictive factor of erectile dysfunction (ED) in prostate cancer (PCa) patients who underwent low-dose permanent I125 seed implant brachytherapy and to investigate if ED could represent a patient’s reported outcome measures (PROMs) of efficacy of BT and indirectly associated with biochemical recurrence free survival (BRFS). From 2000 to 2012, 176 consecutive patients with low-risk PCa underwent BT. ED was evaluated with the International Index of Erectile Function (IIEF-5). Cox regression analysis was performed to assess significant predictors of mild-to-severe ED and BRFS after BT, including covariates. The 10-year actuarial rate of ED was 66%. Subjects with severe ED had higher values of D90 (183.0 versus 177.0; p < 0.05) and V100% (40.1 versus 31.4; p < 0.05) compared with normal. At the multivariate logistic regression analysis, D90 (OR: 1.10; p < 0.05) was an independent predictor of ED. Multivariate Cox-regression analysis did not demonstrate significant association between erectile preservation and biochemical recurrence (BCR) after 10 years of follow up (HR: 2.15; p = 0.20), while D90 ≤ 180 Gy independently predicted BCR (HR: 4.65; [95%CI: 1.25–17.34]; p < 0.05). Erectile preservation should be addressed as valuable PROMs after permanent seed I125 implant, but it is not associated with better BRFS.
Introduction
Prostate cancer (PCa) is the most common cancer amongst men in Europe [Citation1]. The European Association of Urology (EAU) and the European Organization for Research and Treatment of Cancer (EORTC) recommend brachytherapy (BT) as a suitable treatment for patients with low-risk PCa [Citation2–5].
Given the cancer control of this treatment, issues such as quality of life and sexual function become a major preoccupation for patients diagnosed with clinically localized PCa [Citation6].
In a recent study of Ong et al. [Citation7] on 366 consecutive patients treated with BT, the 5-year actuarial rate of EF preservation was 59%. Age at BT seed implant, presence of medical comorbidities, Gleason score and the biologically effective dose were associated with EF preservation.
The quality of surgical care is commonly assessed by objective indicators of operative success such as perioperative morbidity and mortality, intra operative complications, length of hospital stay and readmission rates. Although these are fundamentally important and useful markers of surgical performance, the need for better qualitative, subjective assessment of health care delivery from the patient’s own perspective has led to increased interest in patient-reported outcome measures (PROMs). Indeed, PROMs are deemed useful to analyze surgical outcomes.
With regard to dosimetry, conflicting reports have reported a correlation between biochemical recurrence (BCR) and D90 (the minimum dose received by the “hottest” 90% volume of the prostate), although differences between institution could be explained by the treatment regimens employed [Citation8–10]. To this regard, it could be speculated that erectile dysfunction (ED) could indirectly be associated with BCR, taking into account all patients clinical characteristics and dosimetry data. In fact, the impact of BT parameters' influence on erectile function and the relationship between ED and BCR have not yet been investigated in a long-term setting.
Aim of this study was to investigate the association between long-term ED and BCR after 10 years of follow-up in PCa patients who underwent low-dose permanent I125seed implant brachytherapy (BT). We also aimed to investigate whatever long-term ED could represent a PROMs of efficacy of BT due to its relationship with D90.
Methods
From January 2000 to December 2012, 176 consecutive patients with low-risk PCa who underwent permanent BT were enrolled in this prospective study. Indications for permanent BT were biopsy-proven adenocarcinoma of the prostate and clinically localized low-risk PCa (T classification cT1a–cT2a) with PSA serum level <10 ng/ml and Gleason sum ≤6, <50% of biopsy cores involved with cancer, a prostate volume of <50 cm3 and an International Prostatic Symptom Score (IPSS) <12 [Citation3]. For reduction of the prostate volume or longer waiting time, short-term (3 months) neoadjuvant hormone ablative therapy with anti-androgens was given in 61 patients (34.26%). BT was administered via trans perineal approach using I125 seeds with a prescription dose of at least 145 Gy, respecting the ESTRO/EAU/EORTC recommendations.
All patients underwent a CT scan for dosimetric purposes 4 weeks following the implant. The quality of BT radiation dose was quantified with D 90 (dose received by 90% of the prostate volume) based on this scan.
For each subject, we collected a detailed medical, socio demographic data and sexual history. The short form of the International Index of Erectile Function (IIEF) questionnaire was used for the assessment of subjects’ erectile function and the severity of ED calculated by scoring the five questions as follows: severe (1–7), moderate (8–11), mild to moderate (12–16), mild (17–21) and no ED (22–25) [Citation11]. Patients with severe ED at baseline were excluded. The IIEF-5 was given before the procedure or the start of neoadjuvant therapy. For the purpose of the study, we considered the last IIEF-5 score obtained at the last follow-up on December 2012.
Health-significant comorbidities were scored with the Charlson comorbidity index (CCI) [Citation12], both as a continuous or a categorized variable (i.e. 0 versus ≥1). Follow-up was performed according to the American Brachytherapy Society consensus and biochemical progression after surgery was defined as the first occurrence of an increase of PSA 2 ng/ml above the nadir [Citation13,Citation14].
All participants provided written informed consent before enrolment and the study was conducted in accordance with regulatory standards of Good Clinical Practice and the Declaration of Helsinki (1996). The Institutional review board approved the study protocol.
Statistical analysis
Continuous variables are presented as means ± SDs and differences between groups were tested by Student’s independent t-test or Mann–Whitney U-test according to their normal or not-normal distribution, respectively (normality of variables’ distribution was tested by the Kolmogorov–Smirnov test). The probability of mild-to-severe ED (IIEF-5 ≤ 16) was plotted on the Kaplan–Meier curves, stratified by each patient-, tumor- and treatment-related factor of interest and differences were tested using the log-rank test.
Uni and multivariate Cox regression analysis was performed to assess significant predictors of the probability of mild-to-severe ED(IIEF-5 ≤ 16) and BCR after BT, including: patient age, CCI, pre-operative PSA, prostate volume, use of neo-adjuvant hormones, tumor characteristics, pre-implant IPSS score, pre-implant IIEF-5, D90, V100%, DU, number of needles and number of seeds implanted. A p value < 0.05 was defined to be statistically significant.
Results
lists the baseline characteristics of subjects included. Of all patients, median age was 69.5 years (IQR: 66.0–74.0), median serum PSA was 6.8 ng/ml (IQR: 4.0–8.7), median IIEF-5 was 16.5 (IQR: 14.0–18.75) and median D90 was 185.6 (IQR: 178.67–191.62). Baseline ED was present in 79 (44.4%) patients.
Table 1. Clinical characteristics of patients.
After a median follow-up of 116.58 months (range: 19.96–162.18), the 10-year actuarial rate of ED mild-to-severe ED (IIEF-5 ≤ 16) was 66%. When comparing subjects with mild-to-severe ED with those with normal erectile function, we demonstrated higher values of D90 (183.0 versus 177.7; p < 0.05) and V100% (40.1 versus 31.4; p < 0.05). No difference was observed in terms of DU max, VU150, DR100, VR100, number of needles and number of seeds (). Further, at chi-square analysis, we did not observe any statistical difference in terms of comorbidities at baseline, like hypertension, diabetes, dyslipidemia and CCI, between mild-to-severe (IIEF-5 ≤ 16) ED and normal-to-mild ED (IIEF-5 > 16).
Table 2. Clinical and dosimetry characteristics of patients according to the presence of mild-to-severe (IIEF-5 ≤ 16) ED at the last follow-up.
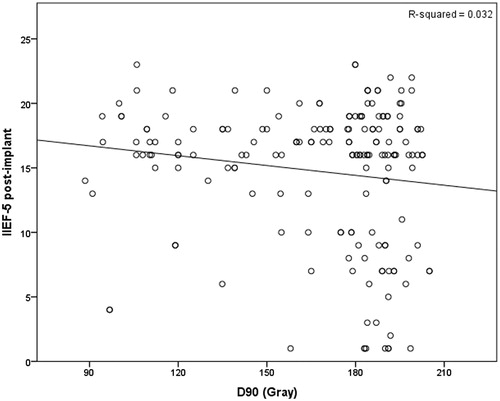
The multivariate linear regression analysis showed an inverse association between D90 (Gy) and IIEF-5 post-implant (r = −0.370; p < 0.05), after adjusting for age, CCI, IIEF-5 pre-implant, V100%, DU Max, VU150, DR100 and number of seeds (). At the multivariate logistic regression analysis, D90 (OR: 1.10 [95%CI: 1.00–1.44]; p < 0.05) was an independent predictor of ED after adjusting for confounding factors, including clinical stage, baseline PSA, biopsy Gleason score, pre-operative neo-adjuvant ADT, pre-operative IIIEF-5 and dosimetry variables (). The overall biochemical recurrence free survival (BRFS) at 10 years was 85.0%.
Table 3. Multivariate logistic regression analysis for significant predictors of mild-to-severe (IIEF-5 ≤ 16) ED.
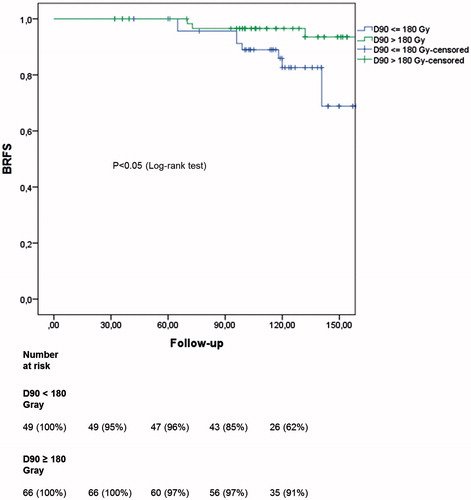
At the Kaplan–Meier curve analysis, the 10-year BRFS in D90 ≥ 180 Gy and D90 < 180 Gy were 91% and 62% (p < 0.05, ) while in moderate-to-severe (IIEF-5 ≤ 16) and moderate-to-mild ED (IIEF-5 > 16) they were 75% and 80% (p = 0.15). Multivariate Cox-regression analysis did not demonstrate significant association between erectile preservation and BCR after 10 years of follow up (HR: 2.15; p = 0.20) while D90 ≤ 180 Gy independently predicted BCR (HR: 4.65; [95%CI: 1.25–17.34]; p < 0.05).
Discussion
Identifying the risk of long-term ED after BT is an important issue for clinicians in order to counsel patients with right information and propose a tailored treatment [Citation15–18]. The Prostate Cancer Outcomes and Satisfaction With Treatment, Quality Assessment, a prospective multicenter longitudinal study predicting long-term erectile function 2 years after PCa treatment, showed that pretreatment sexual health-related quality of life score, young age, African American ethnicity and body mass index >25 were associated with erections suitable for intercourse 2 years after treatment [Citation19].
The important role of organic determinants and, in particular, CVD risk factors should be taken into account when considering pathogenic factors of ED of patients who underwent BT(20), and it may be justified by previous observations where men with CVD and overall atherosclerotic cardiovascular events frequently experienced ED [Citation21,Citation22]. Furthermore, other factors such as PCa characteristics and dosimetry should be taken into account when considering patients undergoing BT.
In the past years, PROMs have gained popularity as appropriate instruments to assess the effectiveness of healthcare intervention. In this regard, ED investigated by the use of IIEF-5 may represent a valuable PROMs after BT seed implant.
Firstly, this longitudinal study confirmed that D90 (OR: 1.10) was the main parameter of dosimetry that predicted mild-to-severe (IIEF-5 ≤ 16) ED, while IIEF-5 pre-implant (OR: 0.73) and CCI (OR: 1.75) are the cofactors.
These results have also been reported by Zelefsky et al. in a multi-institutional analysis of 2693 patients treated with permanent seed BT without ADT or supplemental external beam radiotherapy. In an undefined sub-set analysis of I125 implants (n = 312), the authors demonstrated 8-year PSA relapse free survival of 93% for those with D90 > 130 Gy compared with 76% for those with D90 < 130 Gy.
Similarly, a report on 1298 patients treated with I125 BT concluded that biochemical control was achieved in 88% of patients with D90 ≥ 140 Gy and 78% of patients with D90 < 140 Gy. Furthermore, regarding the relationship between dosimetry and long-term ED, age, pre-implant IIEF score and prostate volume have been associated with low post-implant IIEF-5 score (AUC of 0.75) [Citation6].
On the other hand, this association has been rebutted by Meyer et al. who did not demonstrate that any dosimetric parameter in the segmental dosimetry had an influence at certain time intervals on the development of ED.
Precisely to this regard, age at the time of implantation and the preoperative score in the IIEF-5 had a statistically significant impact on the development of ED in univariate analysis, while the baseline IIEF-5remained statistically significant in multivariate analysis emphasizing the prognostic value of the baseline IIEF-5. Therefore, the underlying ED before implantation as a threshold effect has the most impact on the development of ED and has also been demonstrated by Merrick et al. [Citation23,Citation24] and Solan et al. [Citation25].
However, the proposed underlying mechanism is the irradiation of the internal pudendal arteries, which are branches of the internal iliac artery running alongside the prostate as they course through the pelvis to vascularize erectile tissues of the penis [Citation6].
In this study, we also postulated that the presence of ED could be indirectly related to long-term BCR, since it has been related to D90 and therefore considered as PROMs of BT long-term efficacy [Citation8,Citation26].
We herein reported that the 10-year BRFS in mild-to-severe (IIEF-5 ≤ 16) ED and normal-to-mild ED (IIEF-5 > 16) were 75 and 80% (p = 0.15) and at the multivariate Cox-regression analysis ED was not associated with BCR (HR: 2.15; p = 0.20) in contrast with D90 (HR: 4.65; p < 0.05). We would point out that ED could not represent a valuable PROMs of BT efficacy in spite of its relationship with D90.
However, the lack of such significance may be explained by the multifactorial pathogenesis of ED that occurs in patients with PCa and the difficulty in determining the right onset of ED itself. However, we would also underline that patients of our cohort were all part of low-risk category, justifying the lack of association between PCa extension and ED.
One of the possible strengths of this study is the will of underline the importance of ED and comorbidity as valuable PROMs in patients who underwent BT based on its long-term incidence. Furthermore, erectile preservation should not be considered as a marker of BT inefficacy.
Before concluding some limitations should be addressed. First, this is a single institution longitudinal study. Second, erectile function was investigated using a validated questionnaire (IIEF-5), but no Doppler examination was performed. Finally, BT dosimetry could be different from other published data.
Patients should be addressed about the occurrence of long-term ED after BT for PCa, but it is not related to dosimetry efficacy. Probably, these kinds of patients could be approached with penile rehabilitation at an early phase.
This longitudinal study demonstrated an actuarial rate of ED (IIEF-5 ≤ 16) of 66% at the final follow-up, and it is influenced by D90 and comorbidity. Erectile preservation should be addressed as valuable PROMs in men with PCa treated with permanent seed I125 implant BT, but it is not associated with better BRFS.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article.
References
- Ferlay J, Parkin DM, Steliarova-Foucher E. Estimates of cancer incidence and mortality in Europe in 2008. Eur J Cancer 2010;46:765–81
- Ash D, Flynn A, Battermann J, et al. ESTRO/EAU/EORTC recommendations on permanent seed implantation for localized prostate cancer. Radiother Oncol 2000;57:315–21
- Heidenreich A, Bastian PJ, Bellmunt J, et al. EAU guidelines on prostate cancer. part 1: screening, diagnosis, and local treatment with curative intent-update 2013. Eur Urol 2014;65:124–37
- Hayashi N, Izumi K, Sano F, et al. Ten-year outcomes of I low-dose-rate brachytherapy for clinically localized prostate cancer: a single-institution experience in Japan. World J Urol 2015. [Epub ahead of print]. doi: 10.1007/s00345-015-1480-0
- Li X, Fang D, Cooperberg MR, et al. Long-term follow-up of International Prostate Symptom Score (IPSS) in men following prostate brachytherapy. World J Urol 2014;32:1061–6
- Huyghe E, Delaunay B, Njomnang Soh P, et al. Proposal for a predictive model of erectile function after permanent (125)I prostate brachytherapy for localized prostate cancer. Int J Impot Res 2013;25:121–6
- Ong WL, Hindson BR, Beaufort C, et al. Long-term erectile function following permanent seed brachytherapy treatment for localized prostate cancer. Radiother Oncol 2014;112:72–6
- Herbert C, Morris WJ, Keyes M, et al. Outcomes following iodine-125 brachytherapy in patients with Gleason 7, intermediate risk prostate cancer: a population-based cohort study. Radiother Oncol 2012;103:228–32
- Reis LO, Sanches BC, Zani EL, et al. PSA-nadir at 1 year as a sound contemporary prognostic factor for low-dose-rate iodine-125 seeds brachytherapy. World J Urol 2014;32:753–9
- Guarneri A, Botticella A, Ragona R, et al. Prostate-specific antigen kinetics after I125-brachytherapy for prostate adenocarcinoma. World J Urol 2013;31:411–15
- Rhoden EL, Teloken C, Sogari PR, Vargas Souto CA. The use of the simplified International Index of Erectile Function (IIEF-5) as a diagnostic tool to study the prevalence of erectile dysfunction. Int J Impot Res 2002;14:245–50
- Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987;40:373–83
- Davis BJ, Horwitz EM, Lee WR, et al. American Brachytherapy Society consensus guidelines for transrectal ultrasound-guided permanent prostate brachytherapy. Brachytherapy 2012;11:6–19
- Roach M, III Hanks G, Thames H, Jr et al. Defining biochemical failure following radiotherapy with or without hormonal therapy in men with clinically localized prostate cancer: recommendations of the RTOG-ASTRO Phoenix Consensus Conference. Int J Radiat Oncol Biol Phys 2006;65:965–74
- Wang Y, Liu T, Rossi PJ, et al. Influence of vascular comorbidities and race on erectile dysfunction after prostate cancer radiotherapy. J Sex Med 2013;10:2108–14
- Sullivan JF, Stember DS, Deveci S, et al. Ejaculation profiles of men following radiation therapy for prostate cancer. J Sex Med 2013;10:1410–16
- Chung E, Brock G. Sexual rehabilitation and cancer survivorship: a state of art review of current literature and management strategies in male sexual dysfunction among prostate cancer survivors. J Sex Med 2013;10:102–11
- Incrocci L, Jensen PT. Pelvic radiotherapy and sexual function in men and women. J Sex Med 2013;10:53–64
- Alemozaffar M, Regan MM, Cooperberg MR, et al. Prediction of erectile function following treatment for prostate cancer. JAMA 2011;306:1205–14
- Corona G, Lee DM, Forti G, et al. Age-related changes in general and sexual health in middle-aged and older men: results from the European Male Ageing Study (EMAS). J Sex Med 2010;7:1362–80
- Favilla V, Cimino S, Salamone C, et al. Risk factors of sexual dysfunction after transurethral resection of the prostate (TURP): a 12 months follow-up. J Endocrinol Invest 2013;36:1094–8
- Russo GI, Cimino S, Fragala E, et al. Insulin resistance is an independent predictor of severe lower urinary tract symptoms and of erectile dysfunction: results from a cross-sectional study. J Sex Med 2014;11:2074–82
- Merrick GS, Butler WM, Galbreath RW, et al. Erectile function after permanent prostate brachytherapy. Int J Radiat Oncol Biol Phys 2002;52:893–902
- Merrick GS, Butler WM, Wallner KE, et al. Erectile function after prostate brachytherapy. Int J Radiat Oncol Biol Phys 2005;62:437–47
- Solan AN, Cesaretti JA, Stone NN, Stock RG. There is no correlation between erectile dysfunction and dose to penile bulb and neurovascular bundles following real-time low-dose-rate prostate brachytherapy. Int J Radiat Oncol Biol Phys 2009;73:1468–74
- Munro NP, Al-Qaisieh B, Bownes P, et al. Outcomes from Gleason 7, intermediate risk, localized prostate cancer treated with Iodine-125 monotherapy over 10 years. Radiother Oncol 2010;96:34–7