Abstract
Background: Most patients presenting chest complaints in primary care are referred to secondary care facilities, whereas only a few are diagnosed with acute coronary syndrome (ACS).
Objective: The aim is to determine the optimal cut-off value for a point-of-care heart-type fatty acid binding protein (H-FABP) test in patients presenting to the emergency department and to evaluate a possible future role of H-FABP in safely ruling out ACS in primary care.
Methods: Serial plasma H-FABP (index test) and high sensitivity troponin T (hs-cTnT) (reference test) were determined in patients with any new-onset chest complaint. In a receiver operating characteristic (ROC) curve, the optimal cut-off value of H-FABP for ACS was determined. Predictive values of H-FABP for ACS were calculated.
Results: For 202 consecutive patients (prevalence ACS 59%), the ROC curve based on the results of the first H-FABP was equal to the ROC curve of hs-cTnT (AUC 0.79 versus 0.80). Using a cut-off value of 4.0 ng/ml for H-FABP, sensitivity for ACS of the H-FABP (hs-cTnT) tests was 73.9% (70.6%). Negative predictive value (NPV) of H-FABP for ACS in a population representative for primary care (incidence of ACS 22%) thus could reach 90.8%.
Conclusion: In patients presenting chest pain, plasma H-FABP reaches the highest diagnostic value when a cut-off value of 4 ng/ml is used. Diagnostic values of an algorithm combining point-of-care H-FABP measurement and a score of signs and symptoms should be studied in primary care, to learn if such an algorithm could safely reduce referral rate by GPs.
In patients with chest pain, heart-type fatty acid binding protein (H-FABP) and high sensitivity troponin T (hs-cTnT) have a similar diagnostic potency.
The optimal cut-off value for H-FABP is 4 ng/ml.
The diagnostic value of combining H-FABP measurement with clinical findings should be studied in primary care.
INTRODUCTION
Background
Patients with symptoms possibly due to acute coronary syndrome (ACS) frequently contact their general practitioner (GP) first. In case of suspected ACS, patients will be urgently referred to a secondary care facility since early treatment of ACS markedly increases survival and quality of life (Citation1,Citation2). In primary care, however, differential diagnosis of chest complaints is broad, and ACS is present only in a minority of patients (Citation3). In addition, signs or symptoms decisively distinguishing ACS (with a low prevalence) from high prevalent diagnoses with an advantageous course have not been described earlier (Citation4,Citation5). Furthermore, an electrocardiogram (ECG) reveals no signs of ischaemia in a significant number of patients (Citation6). Therefore, diagnostic means accessible for GPs lack potency to safely rule out ACS and a low threshold for referring patients with possible ACS is maintained. In literature, incidence of ACS among patients presenting symptoms suspected for ACS, is at most 22% and incidence of acute myocardial infarction (AMI) 17% (Citation7,Citation8). In a Dutch cohort of such patients, 27% of patients were not referred, in 8% of whom ACS was diagnosed at a later stage, leading to a false negativity rate of 2%. A total of 73% of patients were referred, 75% of whom were not diagnosed with ACS (false positivity rate or ‘unnecessary referral rate’ 54.8%) (Citation7,Citation9). For a safer and more cost-effective referral policy by GPs, new diagnostic means should become available.
Serial measurement of plasma high sensitivity cardiac specific troponin (hs-cTn), the cornerstone in diagnosing as well as ruling out AMI, is impossible to perform in primary care (Citation10,Citation11). Furthermore, current point-of-care troponin tests are less accurate due to detection limits higher than the widely used cut-off values for a positive test, usually set at the 99th percentile of a healthy population (Citation12). Heart-type fatty acid binding protein (H-FABP) is a small sized protein (molecular mass 15 kD) (Citation13). Therefore, in case of AMI, elevation of plasma H-FABP can be detected within the first one–two hours after onset of complaints (Citation14–16). Several studies have described an added value of H-FABP when measured besides troponin in an emergency room setting in an early phase (Citation17,Citation18). As a solitary rule-out test at admission, high sensitivity cardiac specific troponin T (hs-cTnT) outperforms H-FABP slightly but H-FABP tested in addition to hs-TnT leads to an increase in sensitivity compared to hs-TnT alone (Citation19). The value of H-FABP as a solitary marker in a primary care setting with a typical low prevalence of ACS has been studied once using a point-of-care H-FABP test. Prevalence of ACS was 22% in this study (Citation7). Safe implementation of this test in daily care was opposed by excessive false negative results. This was possibly caused by the relatively high cut-off value for H-FABP (7 ng/ml) of the point-of-care test and a high number of early presenters (presenting within three hours after onset of symptoms) included in this study. In daily general practice, however, a point-of-care test facilitating early rule-out of ACS and reducing unnecessary referral to secondary care facilities would improve the interface between primary and secondary care. It would add to an evidence-based approach of unselected and early presented problems that GPs are faced with and it would increase efficient use of diagnostic facilities in primary care. Thus, several main goals, as formulated by the European General Practice Research Network in the research agenda for general practice/family medicine and primary health care in Europe (http://www.egprn.org) are met.
Objectives
The main objectives of this study are twofold. First, the intention to determine the optimal cut-off value for a point-of-care H-FABP test. Second, to evaluate H-FABP as a potential marker for early triage of patients presenting complaints possibly due to ACS in primary care. Therefore, in an emergency department setting, plasma H-FABP and high sensitivity troponin T (hs-cTnT) levels were compared in an early phase after onset of chest complaints. This study is part of a larger project focusing on point-of-care H-FABP testing in suspected ACS in primary care.
METHODS
Study design
A delayed type cross-sectional diagnostic study was performed in the emergency department of Ziekenhuis Oost-Limburg (ZOL), a large academic hospital in Genk, Belgium.
Patient selection
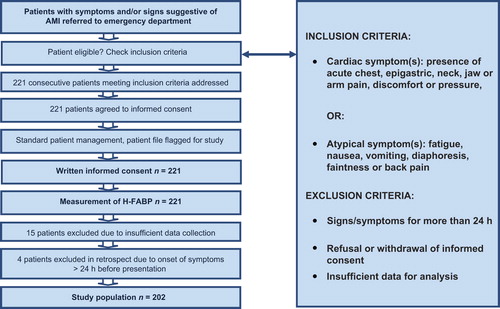
Patients consecutively presenting with cardiac symptoms (presence of acute pain, discomfort or pressure in either chest, epigastric, neck, jaw or arm) or atypical symptoms suspected of cardiac origin (fatigue, nausea, vomiting, diaphoresis, faintness and back pain, without apparent non-cardiac source like a trauma) after triage by an emergency department physician were included. Excluded were patients from whom no informed consent could be obtained and patients with symptoms lasting more than 24 h (H-FABP levels return to baseline 24–36 h after onset of myocardial ischaemia) (Citation13). Patients visited the emergency department on their initiative or they were brought in by an emergency service after referral by a GP or after contacting the emergency service themselves. All patients received routine care considering rule in and rule out of ACS and subsequent treatment. Treating physicians were blind to H-FABP results. A flowchart summarizing patient numbers and the process of inclusion is presented in .
Informed consent
Obtaining patients’ written informed consent in an acute life-threatening situation was considered inconvenient. Furthermore, all medical acts were part of usual care, including blood sampling, except for the additional determination of H-FABP. Patients were, therefore, asked for written informed consent at a later stage. They could decide to withdraw their consent then or at any time after. Only H-FABP results and clinical data of patients who returned a written informed consent were included in the study. The study protocol was in agreement with the WMA Declaration of Helsinki for Ethical Principles for Medical Research Involving Human Subjects and was approved by the Ethical Review Board of ZOL that specifically agreed on the solution for the consent procedure as described above.
Measurements
Presence of the inclusion criteria, symptoms, ECG-findings, time of onset of symptoms, time of drawing the initial blood sample and all laboratory test results were documented. The initial blood samples to measure H-FABP and hs-cTnT were collected by the ambulance staff immediately upon arrival at the patient's site or arrival in our hospital. Routinely, in all venous blood samples—at presentation and any time later during the evaluation at the emergency department—plasma creatinine and hs-cTnT (using Elecsys Cobas fifth-generation hs-cTnT assay by Roche Diagnostics) were measured. Estimated glomerular filtration rate (eGFR) was measured in order to determine the influence of renal clearance on H-FABP and hs-cTn test results. Additionally, a quantitative H-FABP measurement was performed using an H-FABP assay developed by FABPulous BV (limit of detection: 0.5 ng/ml; 99th percentile in a healthy reference population: 5.3 ng/ml) (Citation20).
Outcomes
To allow for a final (gold standard) diagnosis, an ECG was recorded and serial venous blood samples to determine hs-cTnT—used as the reference standard—were analysed. Final diagnoses were established by propounding all data available after an in hospital follow-up of at least 12 h to an expert panel of one independent GP and one independent cardiologist. The expert panel had access to all clinical data including, if performed, the results of coronary angiography. In cases of disagreement, two extra cardiologists and GPs were consulted to determine the final diagnosis unanimously. The expert panel based all decisions on definitions of final diagnoses that were unambiguous and determined beforehand according to current guidelines (Citation10,Citation11,Citation21–24). The expert panel thus utilized the following possible diagnoses: acute myocardial infarction (AMI) with or without ST elevations on ECG (STEMI or nSTEMI), unstable angina (UA), stable angina, no coronary disorders. See for complete definitions.
Table 1. Outcome definitions as used by the expert panel.
(Statistical) analysis
Receiver operating characteristic (ROC) curves have been used to find the mathematical optimal cut-off point of the venous H-FABP-test for ACS as well as to compare H-FABP to the reference test, hs-cTnT. We used exact tests for comparisons between two areas under the curve (AUC) (Citation25). Sensitivity, specificity, positive and negative likelihood ratios (PLR and NLR) for AMI and ACS of H-FABP (cut-off value between positive and negative: greater or equal to 4 ng/ml) and hs-cTnT (cut-off value between positive and negative: above 14 pg/ml) were determined, using outcomes of the expert panel as undisputed diagnoses. Potential negative and positive predictive value (NPV and PPV) in a primary care setting were calculated using Bayes’ theorem. SPSS statistics version 21 and MedCalc were used for the statistical analyses. Before the start of the study, a power calculation revealed that 100 AMI patients were required to compare properly the performance of the plasma biomarkers.
RESULTS
Agreement to the study consent was given by 221 consecutive patients. Four patients appeared to have complaints for more than 24 h. For 15 patients, data collection was insufficient. Therefore, data of 202 patients meeting the inclusion criteria was analysed. Patient characteristics are displayed in . Duration of the complaints ranged between 15 min and 23.3 h. Median duration of complaints was 3 h and 54 min. Of the 202 admitted patients, 119 (59%) were diagnosed with ACS among whom 111 (55% of the total population) had an AMI. A total of 157 patients were males, 93 (59%) of whom had an AMI. Of 45 female patients, 18 (40%) had an AMI. Median age was 62 years (range 26–93 years) and ages of AMI and non-AMI patients overlapped. The duration of the complaints at first contact was 0–3, 3–6, 6–12, and 12–24 h in 82, 40, 56, and 24 patients, respectively. There was no relation between duration of the complaints and AMI risk (P = 0.11; Mann–Whitney). In 193 (96%) patients, the eGFR was > 30.
Table 2. Patient characteristics.
ROC curves based on the results of the first H-FABP and hs-cTnT tests, using ACS as outcome measure, were similar with an area under the curve (AUC) of 0.80 (95% CI: 0.735–0.856) for hs-cTnT and 0.79 (95% CI: 0.728–0.851) for H-FABP (). The optimal cut-point for H-FABP, based on inspection of the curve, was at 4.0 ng/ml, resulting in a sensitivity for ACS of 74.8% and a specificity of 71.1%. Additionally, in , sensitivity and specificity of H-FABP for ACS at adjacent cut-off values are shown.
Figure 2. Receiver operating characteristic (ROC) curve of high sensitivity troponin and H-FABP, optimal cut-off point for H-FABP using ACS as outcome. ACS, acute coronary syndrome; H-FABP, heart-type fatty acid binding protein; hs-cTnT high sensitivity cardiac specific troponin T; ROC curve, receiver operating characteristic curve.
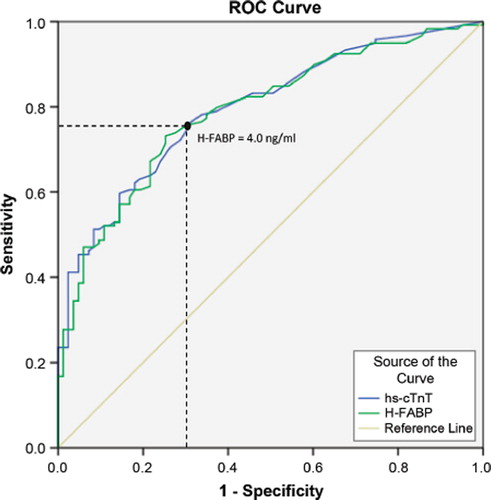
Table 3. Sensitivity and specificity of H-FABP for ACS at different cut-off values between positive and negative. Sensitivity and specificity of H-FABP for ACS at different cut-off values are given for all patients presenting complaints with a duration of 0–24 h and for all patients presenting complaints with a duration of 3–24 h at presentation. NPV is estimated for a population representative for primary care (incidence of ACS = 22%). Sensitivity, specificity and NPV for hs-cTnT with a cut-off of 14 pg/ml are given for comparison.
Sensitivity of H-FABP is strongly related to time between sample taking and the first complaints. Sensitivity for AMI was 63, 88, 96, 83% for patients presenting 0–3, 3–6, 6–12, 12–24 h after onset of symptoms (). During the first six hours after onset of complaints, sensitivity of H-FABP tended to be higher than that of hs-cTnT, without reaching statistical significance. However, within the first three hours after onset of complaints, sensitivity of H-FABP is lower than sensitivity of H-FABP at a time interval of 3–24 h after onset of complaints. Sensitivity for ACS (UA and AMI) is lower than sensitivity for AMI only ().
Table 4. Sensitivity and specificity of hs-cTnT and H-FABP. Sensitivity and specificity of hs-cTnT (cut-off 14 pg/mL) and H-FABP (cut-off 4 ng/mL) for AMI at different time intervals after onset of complaints.
Table 5. Sensitivity of hs-cTnT and H-FABP. Sensitivity and median plasma concentrations (25th, 75th percentile) of hs-cTnT (cut-off 14 pg/ml) and H-FABP (cut-off 4 ng/ml) for STEMI, nSTEMI, all AMI (STEMI and nSTEMI), unstable angina and all ACS (AMI and unstable angina) at presentation, for all patients presenting complaints with a duration of 0–24 h and 3–24 h respectively.
The overall sensitivity and specificity of H-FABP for AMI at presentation using a cut-off value of 4 ng/ml were 77.5% and 71.4% respectively. In a population of patients presenting chest complaints representative for primary care, with an incidence of AMI of 17%, NPV of H-FABP using a cut-off between positive and negative of 4 ng/ml would reach 93.9% for all patients and 97.1% for patients presenting complaints with a duration of at least three hours. For ACS, an overall sensitivity of 73.9% and a specificity of 71% was found. With an incidence of ACS in primary care among patients presenting chest complaints of 22%, NPV would reach 90.8% (). If only data of patients presenting complaints with a duration of more than three hours are regarded, NPV would amount 94.8%. Referral is made to for NPVs of H-FABP at other cut-off values. Furthermore, negative and positive likelihood ratios as well as odds ratios—all independent of the incidence of ACS—are given in .
Table 6. Predictive values and likelihood ratios. PPV and NPV of hs-cTnT (cut-off 14 pg/ml) and H-FABP (cut-off 4 ng/ml) for AMI and ACS at time intervals of 0–24 h and 3–24 h after onset of complaints in a primary care setting with an incidence of AMI of 17% and ACS of 22%. PLR, NLR and OR of hs-cTnT (cut-off 14 pg/ml) and H-FABP (cut-off 4 ng/ml) for AMI and ACS at time intervals of 0–24 h and 3–24 h after onset of complaints.
If H-FABP was used as a stand-alone test at presentation, in this population of 202 patients among whom 119 patients were diagnosed with ACS, 31 patients (25 AMI, 6 UA) would test false negative (i.e., H-FABP < 4 ng/ml at presentation in an eventual case of ACS). Using only hs-cTnT at presentation, 35 patients would be missed (30 AMI, 5 UA). Among 24 false positive cases (i.e., H-FABP at or above 4 ng/ml in eventually ACS negative patients as based on serial hs-cTnT measurements and clinical judgment), 15 patients were diagnosed with either a non-cardiac mild disease or with stable angina, whereas 9 cases related to moderate to severe alternative cardiac diagnoses needing acute treatment.
H-FABP and hs-cTnT values were compared in patients with an eGFR at or above 30 ml/min versus below 30 ml/min according to their ROC curves and AUC. There was no significant difference between both markers in both subgroups and for each marker the 95% confidence intervals overlapped with both renal function groups. However, only 9 patients with an eGFR below 30 ml/min were included.
DISCUSSION
Main findings
The main objectives of this study were to determine the optimal cut-off point of H-FABP and to assess the possible diagnostic potency of plasma H-FABP in patients presenting with chest pain to the GP. The cut-off value for ACS of H-FABP, where sensitivity and specificity reached optimal values, is 4.0 ng/ml. Using this cut-off value for H-FABP, sensitivity for AMI of the H-FABP (hs-cTnT) tests was 77.5% (73.0%) for all patients at presentation and the sensitivity for ACS was 73.9% (70.6%). Based on the results of this study, H-FABP with a cut-off value of 4.0 ng/ml could reach an overall NPV for AMI of 93.9% and for ACS of 90.8% in an unselected primary care population (estimation based on a prevalence of ACS of 22%).
Strengths and limitations
The strength of this study is its performance in a population of consecutive patients presenting to an emergency setting covering the broad spectrum of referred and non-referred patients, complying with usual care for chest pain bridging primary and secondary care. The outcome measurement complied with recent evidence-based guidelines (Citation11). Besides, with our emergency department based data in a high prevalence setting of ACS, estimations for an NPV in an unselected primary care setting with a lower prevalence could be made. These estimations are limited by the fact that data was not gathered in a true primary care population, where sensitivity and specificity could differ slightly, as it is known that these parameters are influenced by different characteristics of a given population (Citation26). Thus, further research in primary care has to be carried out to evaluate the actual role of H-FABP in assessing patients who present complaints possibly due to ACS. All the more since in this study laboratory testing was used, whereas point-of-care testing in the field could be susceptible to more user error.
Compared to recent literature, a higher incidence of AMI was found in these patients of 55%. This is probably due to the presence of an emergency doctor that performs triage of patients before consultation by a cardiologist if necessary. Furthermore, using hs-cTnT combined with criteria meeting contemporary international guidelines, incidence of nSTEMI rises, while incidence of UA falls (only 4% in this population), as is described in current literature (Citation27).
Interpretation, implications for future research
H-FABP as a stand-alone test seems unable to rule in and out ACS, especially in early presenters (< 3 h) and in case of UA. However, the estimated NPV of 90.8% in a primary care population could be further improved when signs and symptoms are added to point-of-care H-FABP measurement in a clinical decision rule (CDR). False positivity of H-FABP alone would be 29% for ACS, whereas currently 54.8% of patients presenting chest complaints to their GP are referred without an underlying ACS. Actual effect on referral decisions of a CDR combining signs, symptoms and point-of-care H-FABP testing in primary care merits further study. We, therefore, intend to test the incremental diagnostic value of a recently launched point-of-care H-FABP test with a cut-off value of 4.0 ng/ml combined with signs and symptoms in primary care (Citation28).
Conclusion
In patients presenting chest pain at an early stage, H-FABP and hs-cTnT have the similar diagnostic potency. The optimal cut-off value for H-FABP is 4 ng/ml. Possibly, H-FABP could be of value in reducing referrals by GPs of eventually ACS negative patients and in reducing missed cases of ACS in primary care. Thus, in future studies performed by GPs, the diagnostic value of a CDR, combining signs, symptoms and point-of-care H-FABP testing—using 4.0 ng/ml as a cut-off value—in a true primary care population should be studied.
ACKNOWLEDGEMENTS
All authors should like to thank participating patients, as well as all emergency personnel executing our research protocol at hospital ZOL, Genk, Belgium.
FUNDING
The study is funded by means of an unrestricted grant by FABPulous BV, the company that develops point-of-care H-FABP-tests. FABPulous BV agreed not to interfere with data collection, data management and analysis of data. Publication of possible unfavourable outcome of our study was guaranteed.
Declaration of interest: JG is chief scientific officer (CSO) at FABPulous BV. The remaining authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Notes
*Oral presentation at the annual research conference of the European Primary Care Cardiovascular Society (EPCCCS) in London, September 2013.
References
- Reimer KA, Jennings RB. The ‘wavefront phenomenon’ of myocardial ischemic cell death. II Transmural progression of necrosis within the framework of ischemic bed size (myocardium at risk) and collateral flow. Lab Invest. 1979;40:633–44.
- Gersh BJ, Stone GW, White HD, Holmes DR Jr. Pharmacological facilitation of primary percutaneous coronary intervention for acute myocardial infarction: Is the slope of the curve the shape of the future? J Am Med Assoc. 2005;293:979–86.
- McConaghy JR, Rupal S. Outpatient diagnosis of acute pain in adults. Am Fam Physician 2013;87:177–82.
- Bruyninckx R, Aertgeerts B, Bruyninckx P, Buntinx F. Signs and symptoms in diagnosing acute myocardial infarction and acute coronary syndrome: A diagnostic meta-analysis. Br J Gen Pract. 2008;58:105–11.
- Body R, Carley S, Wibberley C, McDowell G, Ferguson J, Mackway-Jones K. The value of symptoms and signs in the emergent diagnosis of acute coronary syndromes. Resuscitation 2010;81:281–6.
- Rutten FH, Kessels AG, Willems FF, Hoes AW. Electrocardiography in primary care: Is it useful? Int J Cardiol. 2000;74:199–205.
- Bruins Slot MH, Rutten FH, Van der Heijden GJ, Doevendans PA, Mast EG, Bredero AC, et al. Diagnostic value of a heart-type fatty acid-binding protein (H-FABP) bedside test in suspected acute coronary syndrome in primary care. Int J Cardiol. 2013; 168:1485–9.
- Nilsson S, Scheike M, Engblom D, Karlsson LG, Mölstad S, Akerlind I, et al. Chest pain and ischaemic heart disease in primary care. Br J Gen Pract. 2003;53:378–82.
- Bruins Slot MH, Rutten FH, Van der Heijden GJ, Geersing GJ, Glatz JF, Hoes AW. Diagnosing acute coronary syndrome in primary care: Comparison of the physicians’ risk estimation and a clinical decision rule. Fam Pract. 2011;28:323–8.
- Newby LK, Jesse RL, Babb JD, Christenson RH, De Fer TM, Diamond GA, et al. ACCF 2012 expert consensus document on practical clinical considerations in the interpretation of troponin elevations: A report of the American College of Cardiology Foundation task force on clinical expert consensus documents. J Am Coll Cardiol. 2012;60:2427–63.
- Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD: the Writing Group on behalf of the Joint ESC/ACCF/AHA/WHF Task Force for the Universal Definition of Myocardial Infarction. Third universal definition of myocardial infarction. Circulation 2012;126:2020–35.
- Nilsson S, Andersson PO, Borgquist L, Grodzinsky E, Janzon M, Kvick M, et al. Point-of-care troponin T testing in the management of patients with chest pain in the Swedish primary care. Int J Family Med. 2013; doi: 10.1155/2013/532093. Epub 10 January 2013.
- Glatz JF, Renneberg R. Added value of heart-type fatty acid- binding protein as plasma marker for the early evaluation of suspected acute coronary syndrome. Clin Lipidol. 2014;9: 205–20.
- Dekker MS, Mosterd A, van ‘t Hof AW, Hoes AW. Novel biochemical markers in suspected acute coronary syndrome: Systematic review and critical appraisal. Heart 2010;96:1001–10.
- Glatz JF, van der Vusse GJ, Simoons ML, Kragten JA, van Dieijen-Visser MP, Hermens WT. Fatty acid-binding protein and the early detection of acute myocardial infarction. Clin Chim Acta. 1998; 272:87–92.
- Mad P, Domanovits H, Fazelnia C, Stiassny K, Russmuller G, Cseh A, et al. Human heart-type fatty-acid-binding protein as a point-of-care-test in the early diagnosis of acute myocardial infarction. QJM 2007;100:203–10.
- McMahon CG, Lamont JV, Curtin E, McConnell RI, Crockard M, Kurth MJ, et al. Diagnostic accuracy of heart-type fatty acid- binding protein for the early diagnosis of acute myocardial infarction. Am J Emerg Med. 2012;30:267–74.
- Carroll C, Al Khalaf M, Stevens JW, Leaviss J, Goodacre S, Collinson PO, et al. Heart-type fatty acid binding protein as an early marker for myocardial infarction: Systematic review and meta-analysis. Emerg Med J. 2013;30:280–6.
- Collinson P, Gaze D, Goodacre S. Comparison of contemporary troponin assays with the novel biomarkers, heart fatty acid binding protein and copeptin, for the early confirmation or exclusion of myocardial infarction in patients presenting to the emergency department with chest pain. Heart 2014;100:140–5.
- Glatz JF, Mohren R. Plasma reference value of heart-type fatty acid-binding protein, the earliest available plasma biomarker of acute myocardial infarction. Health 2013;5:1206–9.
- Hamm CW, Bassand JP, Agewall S, Bax J, Boersma E, Bueno H, et al. ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: The Task Force for the management of acute coronary syndromes (ACS) in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2011;32:2999–3054.
- National Clinical Guideline Centre for Acute and Chronic Conditions. Chest pain of recent onset: NICE Guideline. http://www niceorg uk/nicemedia/live/12947/47938/47938 pdf (2010 NICE Clinical Guideline 95) (accessed 1 July 2014).
- Steg PG, James SK, Atar D, Badano LP, Blömstrom-Lundqvist C, Borger MA, et al. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force on the management of ST-segment elevation acute myocardial infarction of the European Society of Cardiology (ESC). Eur Heart J. 2012;33:2569–619.
- Fox KA, Goodman SG, Klein W, Brieger D, Steg PG, Dabbous O, et al. Management of acute coronary syndromes. Variations in practice and outcome; findings from the global registry of acute coronary events (GRACE). Eur Heart J. 2002;23:1177–89.
- Hanley JA, McNeil BJ. A method of comparing the areas under receiver operating characteristic curves derived from the same cases. Radiology 1983;148:839–43.
- Whiting P, Rutjes AW, Reitsma JB, Glas AS, Bossuyt PM, Kleijnen J. Sources of variation and bias in studies of diagnostic accuracy: A systematic review. Ann Intern Med. 2004;140:189–202.
- Mueller C. Biomarkers and acute coronary syndromes: An update. Eur Heart J. 2014;35:552–6.
- Willemsen RTA, Buntinx F, Winkens B, Glatz JF, Dinant GJ. The value of signs, symptoms and plasma heart-type fatty acid-binding protein (H-FABP) in evaluating patients presenting with symptoms possibly matching acute coronary syndrome: Background and methods of a diagnostic study in primary care. BMC Fam Pract. 2014;15:203. doi:10.1186/s12875-014-0203-8.