Use of modern technology for diagnosis and monitoring in general practice
In most European countries, there is no tradition of including novel technological tests and devices in daily general practice. We often use this as a motto: ‘general practice is the low-technology medicine’, implying that it is cheap and more human. However, the technological development made devices smaller, lighter and cheaper. We used a survey in five countries to estimate the interest of GPs for new point-of-care (PoC) laboratory tests. Horizon scanning reports and contact with producers of new technological devices brought us in contact with new products and products that are in the pipeline. Currently, the challenge for primary care research is to estimate which novelties have a benefit for daily clinical work in general practice.
Testing a new device starts with estimating its possible incremental value in combination with standard clinical signs and symptoms. If this is insufficient, the device will not be able to improve clinical work, and the evaluation process should be stopped. Subsequent steps in the process include technical validation, evaluation of the feasibility and user-friendliness and testing the device's benefit in a large-scale clinical study.
At the EGPRN meeting in Timisoara, we concentrated on diagnosis and monitoring, including PoC laboratory tests and monitoring devices to be used in acute care situations. To illustrate problems and opportunities, we discussed results of recent and ongoing studies of using PoC tests in different clinical situations: the use of C-reactive Protein (CRP) tests for detecting serious disease in children, diagnosing pneumonia in adults and urinary infections in old-age residents in nursing homes, as well as the use of Heart-type fatty acid binding protein (H_FABP) in chest pain patients. Additionally, we discussed experiences with monitoring devices for use in patients with chest pain or dyspnoea: oximetry, heart scan, the Innocare PICO, and wearables, which are still in development.
To introduce the audience into designing and operationalizing their own studies, we also discussed current needs for even more additional tests and devices, the relation between general practice research groups and the industry, methodological problems in evaluating diagnostic tests for rare diseases and quality control issues.
Today, western societies are faced with the phenomenon of specialization and subspecialization in a variety of different areas such as the economy, industry, and the arts and, of course, healthcare and medicine. Moreover, we are painfully aware that there is an increasing lack of competencies and skills that are necessary for a generalistic and holistic approach. This approach is useful in any area for coordinating various specialty services or for demonstrating common sense in complex situations. In healthcare, in just a few decades we have observed that the once broad fields of internal medicine and surgery split into smaller system based specialities such as cardiology or pulmonology, which subsequently required further subspecialization into areas such as interventional cardiology or minimal invasive surgery. Without doubt, these new techniques not only require highly specialized facilities and equipment but also highly skilled professionals for improved outcomes. Similarly, within Wonca and in the field of family medicine and family medicine research, we witness the founding and growth of special interest groups such as in the fields of cardiology, gastroenterology or respiratory diseases. In clinical practice at the primary care level, we see family medicine colleagues specializing in psychosomatic diseases, in manual therapy, musculoskeletal diseases, treatment of drug-addicted patients or in complementary medicine. This focus on certain areas of clinical medicine very often leads to a research focus in the same area along with the respective research methodology.
Obviously, there are many reasons for these developments in family medicine. New methods or techniques such as point-of-care tests or ultrasound may require specific and expensive equipment and special training, which once initiated, can be the starting point for specialization in these activities. Other reasons may be the special interest of colleagues in a certain area such as psychosomatic diseases or substitution treatment for drug-addicted patients. In academia, the requirements for a career and academic promotion are set by the universities and include unique skills that add value to the faculty and emphasize scientific publications in high impact journals. Usually, with a few exceptions, specialized journals have a higher impact factor than typical family medicine journals, which may motivate ambitious colleagues to specialize in research methodologies required for a well-recognized specialty in the field of family medicine.
Certainly, to be firm in a special research methodology—be it in quantitative or qualitative methods—helps in designing studies and in writing publications. Similarly, being recognized in a certain area as a scientist with a documented publication record helps speed up writing time and publication output. Together, these are two helpful circumstances, which facilitate an academic career. Alternatively, increased competency and skills in a small area of expertise usually result in a loss of competence in other areas. This may not only slow down the development of academic family medicine but also may be a loss for patients in their trust in the generalist approach of their GP/FP. It also may be a loss for the healthcare system, which should be founded on sound and comprehensive primary care services. Overall, there is the danger that family medicine is losing its unique position as the specialty for primary care.
The presentation in Timisoara elaborated on the pros and cons of specializing within the discipline of family medicine. Moreover, it aims not only to make the audience aware of risks and chances but also to provoke the audience with a clear personal position on this topic.
We live in an age where we need technology to make us more efficient in every domain. Healthcare also needs to be optimized to keep up the pace with the developing world.
In Romania, the Government has passed a national programme called National Health Care Strategy 2014–2020, which is supposed to follow WHOs European Strategy 2020. Public health, healthcare services and transversal methods, which include the promotion of research, innovation and the use of technology, are the main trajectories of this national programme. It consists of the following elements:
A strategy of public health should make family doctors increasingly competent in solving problems of patients suffering from the main chronic diseases such as diabetes, hypertension, COPD, asthma and chronic renal disease.
A strategy regarding healthcare services should diversify the services offered by family doctors and make primary healthcare more effective in taking pressure off the secondary healthcare service.
A strategy regarding transversal methods should promote research and innovation in the healthcare system and accelerate the use of modern technology in the healthcare system.
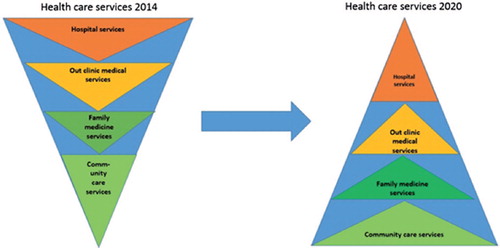
The outline of the healthcare system in 2020 is presented in .
The National Research, Development and Innovation Strategy 2020 (SNCDI 2020) is another programme issued by our government, where healthcare is supposed to be integrated with a national research and innovation programme. Results ought to be transferred into the medical practice at a national level, putting them to practical use in the daily activity of doctors at national level.
With the occasion of the EGPRN Spring Meeting 2015, the Timis Society of Family Medicine, together with the University of Medicine and Pharmacy Timisoara have taken into account all these issues and have composed a research nucleus between Romanian family doctors in the area and the university. Using all the new tools technology is providing, we want to establish a relevant database and use it as a support for new research and innovation to improve medical activity and knowledge about patients and their diseases.
This EGPRN meeting is a positive sign for Romanian colleagues from family medicine and encouragement to participate in the development of national primary research. Romania requires a new medical elite (without political implications) and positive models for repositioning of our national values. We consider it imperative for Romanian colleagues, to have greater involvement in evidence-based medicine by conducting a national research network connected to EGPRN.
Romanian family doctors, especially those with an applied research preoccupation and those who use therapeutic guides and protocols, need to be informed about the experience of EGPRN members. They need to see Western European medical activity and to communicate with those experts, to establish relationships so that in the future they can create a national research network of family doctors in Romania.
Primary healthcare services are mainly delivered by family doctors who are independent practitioners contracted by the (public) health insurance fund. Family doctors are assigned as gatekeepers of the healthcare system.
The establishment of a research tradition in Romanian primary healthcare has been inhibited by the relative isolation of practitioners, reduced financial support devoted to primary care research, less time, insufficient research training, in addition to the absence of dual (clinical and research) contracts.
We will try to build a research model, both at the regional and national level, using current resources. These resources include well-trained family physicians, existence of many instructors—trainers of family physicians, the existence of an electronic patient database, the existence of the academic disciplines of family medicine, existence of the National Society of Family Medicine consisting of 10 working groups (some old and already affiliated to Wonca, some in development) with interests in diverse areas of research. For instance, the young Romanian family doctors—Vasco da Gama Movement, respiratory diseases, vaccinology, mental health, practice ultrasonography and others, who already have the necessary infrastructure of research project development.
The aim of the future National General Practice Research Network, under the guidance of EGPRN, is to provide a suitable setting in which to discuss and develop research in primary care, to design and coordinate multinational studies, to exchange experiences, to create training research workshops, to conduct national and international research projects and to develop a validated scientific basis for general practice.
For this purpose, we are involved in this important collaboration with you, the European researchers’ brand, where you can share with us your expertise from research in primary care. You are true models for us and we are glad to be able to learn more from your experience. One great advantage that we have for the future development of research in Romania is access to European funds made available for this purpose. For the beginning, we feel the best way to support individual researchers is to support the effective development of international research collaboration through relationships with national representatives, national colleges and Wonca.
Unbalanced rather than balanced randomized controlled trials are more often positive in favour of the new treatment: An exposed and non-exposed study

Background: Unbalanced randomized controlled trials (RCTs) are trials with unequal probability to be allocated to one group instead of another. Clinical equipoise is a prerequisite for an RCT and is defined as a state of uncertainty where a person believes it is equally likely that either of two treatment options is better. A 1:1 ratio thus appears to fit this state of uncertainty best.
Research question: Is the clinical equipoise principle respected in unbalanced RCTs, i.e. in trials in which more patients are allocated to the new treatment, as compared to the control one?
Method: Observational and comparative study between unbalanced and balanced RCTs. We searched the ‘core clinical journal’ of MEDLINE to identify reports of two parallel-group superiority unbalanced RCTs published between January 2009 and December 2010. For each unbalanced RCT, we identified a maximum of four reports (to maximize power) of matched balanced RCTs dealing with the same population. Our primary outcome was the proportion of positive RCTs, i.e. when results for its primary outcome were statistically significant (P < 0.05) with greater efficacy with the new treatment than the control treatment.
Results: Forty-six reports of unbalanced RCTs and 164 of balanced RCTs were selected. We found that 65.2% unbalanced RCTs and 43.9% balanced RCTs were positive (OR: 2.38; 95% CI: 1.23–4.63). As compared with balanced RCTs, unbalanced RCTs were more often industry-funded, and their control treatments were more often inactive. Adjusting on these latter variables did not modify the results.
Conclusion: This result questions the respect of the clinical equipoise principle in unbalanced RCTs.
REFERENCE
- Okuno J, Yanagi H, Tomura S, Oka M, Hara S, Hirano C, et al. Compliance and medication knowledge among elderly Japanese home-care recipients. Eur J Clin Pharmacol. 1999;55:145–9.
A new method for estimating population morbidity based on routine primary care electronic medical records
Background: Routinely recorded electronic health records (EHRs) from family physicians (GPs) are increasingly available and provide a valuable source of data for morbidity estimates in the population. This is one of the key elements of a learning healthcare system.
Research question: This paper describes how we developed an algorithm to process raw data to arrive at valid incidence and prevalence estimates in the population.
Methods: The study was performed using EHR data that were provided by 386 Dutch general practices that participate in the NIVEL primary care database, and that covered a total patient population of approximately 1.2 million patients in 2012. Diagnoses were recorded using the International Classification of Primary Care version 1 (ICPC-1). For this study, we used morbidity data from 2010–2012, including ICPC-coded consultations and prescriptions, to develop an algorithm to construct disease episodes over the year 2012.
Results: All 685 symptoms and diseases of ICPC-1 were categorized as acute symptoms/diseases, long-lasting reversible diseases, and chronic diseases. For each category, an algorithm was developed to construct disease episodes. The algorithm translates care episodes, as recorded in EHRs, into disease episodes as are likely to exist in the population, using input from EHRs in combination with expert knowledge on the course of diseases. These constructed disease episodes were used to calculate incidence and prevalence rates.
Conclusion: An algorithm was developed to construct disease episodes based on routinely recorded morbidity data from EHRs of GPs, which can be used to estimate morbidity rates. The ingredients of this algorithm are available in most EHR systems, implying that the method can be easily applied in other countries and other primary care networks.
Background: The few Danish studies on email consultations were undertaken before it became mandatory under the Danish law in 2009 to offer patients email consultation. These first movers, i.e. enthusiastic patients and GPs, showed that the GP's enthusiasm for email consultation affects the patient's approach to the medium. In 2013, the number of email consultations had increased markedly, reaching four million—equivalent to 11.2% of all GP consultations in Denmark.
Research question: This study investigates the ways in which patients and GPs communicate with each other by email, explore factors influencing this means of communication and puts into perspective the potential of email consultations in patient's treatment.
Method: The study is explorative and based on an individual interview and four qualitative focus group interviews. The empirical data were analyses from a social constructivist and a practice-theoretical approach.
Results: Patients wanted to be able to use the GP as a sparring partner in email consultations. They expected a reply in case of uncertainties. The GPs found it difficult to handle complicated medical problems by email and they tended to send a standard reply. Some patients perceived the wording of the standard reply as a rejection of their problem. Patients highlighted the logistical advantages of email consultations, the physical separation of doctor and patient, which made it easier for them to disclose psychological or intimate issues. The GPs preferred short, uncomplicated questions with no option for the patient to enter into a discussion.
Conclusion: Patients and GPs have different approaches to email. The development of clear guidelines for patients and revised guidelines for GPs regarding email consultations is, therefore, recommended. The medium has potential as a platform for sharing information and images and for helping patients to learn more about their conditions by providing links to articles and websites.
Background: Ultrasonography is a quick inexpensive imaging technology to complete clinic examination. Practitioners need regular practice and initial formation to have an optimal diagnosis. There is no formalized teaching for general practitioners (GPs) in France.
Research question: The aim of this study was to update knowledge about indications for ultrasonography in general practice, following a systematic review of the literature.
Method: Following the PRISMA recommendations for systematic reviews, articles from PubMed, Cochrane Library and Embase were examined. All articles referring to ultrasonography done by GPs before 2012 were included. Languages were not a limitation. Articles without IMRAD structure were excluded.
Results: Thirty-five studies were found. Publication period was between 1985 and 2012. Only a few references on specific organs took an interest in primary care. Most articles came from North America, England and Norway. Five fields were identified: vascular, cardiac, obstetrical, abdominal and emergency. Obstetrical papers were the most frequent, but vascular were the most recent. Most recent article described new indications: screening for abdominal aortic aneurism (AAA) and assessment of left ventricular function, respectively. A training model for abdominal ultrasound was approved. GPs technical skills were sometimes equivalent (92% for abdominal exam, 92–96% for fetal age estimation, or fetal weight, AAA screening), and sometimes less than trained specialists (cardiac examination in emergency context).
Conclusion: GPs are as good as specialists are in abdominal ultrasonography, AAA screening, fetal weight and age estimation. New indications for GP's ultrasonography practice are being published in the medical press.
Background: Early in the consultation with the patient, diagnostic hypotheses ‘pop into the mind‘ of the clinician. Further information search is guided by a small number of hypotheses aiming at confirmation or disconfirmation. This hypothetico-deductive strategy (HDS) has been the prevailing model to understand diagnostic reasoning in medicine.
Research question: Is the HDS the prevailing cognitive strategy in primary care? To what extent do other strategies contribute?
Method: Twelve GPs had 282 of their consultations videotaped, 134 contained at least one of an overall 163 diagnostic episodes. After each consultation, GPs were asked to reflect on their diagnostic reasoning. Transcripts were analysed using quantitative and qualitative methods. We quantified cues, i.e. pieces of clinical information, obtained by different cognitive strategies.
Results: GPs were shown to use HDS in only 39% of diagnostic episodes. Other cognitive strategies were at least as important, such as inductive foraging in 91% of consultations and triggered routines in 38% of diagnostic episodes. On average, the HDS contributed only 12% of cues obtained by GPs during a diagnostic episode.
Conclusion: HDS is relevant only after narrowing the range of possible hypotheses. In generalist settings with unselected patient problems, the range of diagnoses should not be restricted too early. Cognitive strategies such as inductive foraging or triggered routine help GPs keep an open mind and prevent premature closure.
Background: Ankle-brachial index (ABI) changes with the periphery arterial damage. Pulse wave velocity (PWV) represents the gold standard for determining arterial stiffness.
Research question: Does ABI correlate with arterial stiffness in a hypertensive person directly or indirectly?
Method: We selected 95 hypertensive patients aged between 40 and 80 years. Secondary hypertension has been excluded. Using the Guideline of the European Cardiology Society, we evaluated the ABI for each patient with an (8M continuous bidirectional) Doppler device. PWV has also been determined for each patient, using an arteriograph (Medexpert) device. Trying to establish a correlation, the patients have been split into two groups: group (A) patients with ABI ≤ 1 and group (B) patients with ABI > 1. We calculated the Pearson correlation index.
Results: We calculated the correlation index between ABI and PWV: The correlation index in group (A) between ABI = 0.921 (standard deviation (SD) = ± 0.072) and PWV = 9.29 m/s (SD = ± 1.94) was r = –0.701 (negative correlation). The correlation index in group (B) between ABI = 1.178 (SD = ± 0.089) and PWV = 9.29 m/s (SD = ± 1.94) was r = 0.691 (positive strong correlation).
Conclusion: Arterial stiffness measurement represents a simple method to evaluate patients in primary care (GPs). PWV correlates positively to ABI when it is greater than one value and negatively when less than one.
Mutual trust in general practitioner–patient relationship in the context of irritable bowel syndrome: A qualitative study
Background: Chronic diseases are major causes of morbidity and mortality worldwide. Their effects can be mitigated by high-quality evidence-based care, but this is not the norm in most health systems. Mutual trust in the general practitioner (GP)–patient relationship is crucial for patients’ adherence to doctors’ therapeutic recommendations. However, there is little knowledge with respect to how mutual trust is built in the GP–patient relationship.
Research question: What are the pathways through which mutual trust in the GP–patient relationship is built and maintained in the context of irritable bowel syndrome (IBS)?
Method: We conducted a qualitative study using semi-structured interviews with 20 patients with IBS, living in Iasi, Romania. IBS has been used as a case study for mutual trust in the context of chronic diseases. Interviews were focused on trust-related experiences of patients with their GPs in the context of IBS. Interviews were analysed by using the constant comparative method. Data analysis was assisted by QSR NVivo software.
Results: Our preliminary data analysis identified two communication styles—positive reinforcement (PR) and negative reinforcement (NR)—with different impacts on mutual trust. We describe these two communication patterns and show that PR style has promoted mutual trust in the GP–patient relationship. Through this, patients’ engagement with their care and patients’ motivation to maintain their health more generally was also promoted. NR style has promoted patients’ confidence in their GPs in only some cases and to some extent patients’ compliance with medical approaches.
Conclusion: This study enlarges our understanding of mutual trust in general practice by showing patients’ trust in their GPs and GPs’ trust in their patients were interdependent for building mutual trust in the GP–patient relationship in the context of IBS. This, in turn, underpinned all the dimensions of patients’ motivation to engage in their care and to maintain their health more generally.
Background: The French Health Authority recommends a systematic weighing of adults (expert agreement). Overweight patients feel stigmatized and are reluctant to talk about weight. Physicians wonder about the efficiency of overweight management. No study has been found on GPs doing the weighing, and the feelings of non-obese patients about this action.
Research question: How is the topic of weight initiated in the GP consultation?
Method: Explorative study with direct observation of GPs’ consultations by trainees. A standardized observation grid allowed collecting a description of adult patients, physicians, the first sentences delivered during weight discussion and weighing, and the patient's reaction. Analyses were univariate and multivariate on statistical data, and inductive (grounded theory) on verbatim (double-blind coding, resolution of disagreements by discussion).
Results: The topic of weight occurred in 72 (38.2%) of the 187 consultations, with a discussion and/or weighing. Physicians initiated the majority of the discussions about weight and weighing. Frequency of bringing up the topic of weight varies among physicians (from 13.6% to 80%). This topic occurred more often with older patients, those overweight, and those with a cardiovascular and endocrine history and with those who consulted for a chronic follow-up (P < 0.05). Requests for weighing by physicians were very directive and sometimes seemed to make patients feel uncomfortable. The discussion about weight without weighing seemed to enhance reflection on a possible change of the patient's behaviour.
Conclusion: GP's behaviours are numerous. A less directive approach seems to allow a reflexive approach by patients that is concordant with motivational interviewing theory. The importance of weighing during consultations could be reconsidered.
Background: Authors of guidelines or proposals for clinical trials are increasingly requested to prove that their outcome measures or recommendations meet patients’ concerns and priorities. Some programmes obligate authors to consult patient representatives to discuss the relevance of outcome measures in both clinical trials and guidelines.
Research question: Which outcome measures for urinary tract infection (UIT) trials are considered most relevant by patients and do address their concerns and priorities?
Method: To assess the patient relevance of outcomes of a planned UTI trial as well as in the national guideline, we (a) systematically reviewed outcome measures used in UTI trials, (b) systematically searched for papers on patients’ views and concerns on UTI and its treatment, and (c) plan to perform focus groups with patients to discuss which treatment goals and outcome measures are considered relevant.
Results: (Preliminary.) A first (still incomplete) literature review suggests that most UTI trials feature either urine cultures and/or typical symptoms as primary outcome measures. Symptoms are often assessed by doctors or nurses rather than patients and scored nominally (yes/no) or assessed using simple symptom scores, which are mostly not formally validated. Trials looking in more detail at how much patients are bothered or concerned by their condition are rare. Few quantitative studies look in depth into patient perceptions and priorities on treatment goals or relevance of outcomes.
Conclusion: (Preliminary.) It seems that many studies do not consider patient-relevant outcomes at all, or only with a relatively coarse approach. Thus, our results will help to create a basis for patient-relevant UTI research.
Background: Ambulatory care contributes massively to the rising of health costs. It is recognized that general practitioners (GPs) are more cost-efficient in the treatment of ambulatory patients than hospital emergency departments.
Research question: We aimed at understanding the subjective reasons, which lead patients, confronted with a perceived urgent medical problem, to choose either their GP or the hospital emergency facilities.
Methods: This qualitative study was based on the grounded theory. We collected data using a semi-structured questionnaire. We interviewed adults suffering from non-acute medical problems. Half of them were recruited after an ambulatory consultation at the hospital emergency department. The other half consisted of patients who consulted their GP. Audiotape recordings of the interviews were transcribed verbatim and coded with NVivo software. Attention was paid to a balanced sample concerning sex, age, nationality, education level, and geographical location.
Results: Twenty interviews were necessary to obtain saturation of the information. The quality of the relationship between the patient and their family doctor was one of the major reasons for them consulting the primary care physician first rather than the emergency hospital unit. The more patients feel they have a meaningful relationship with their doctor, the more readily they will seek advice from him. This attitude is often appropriate but sometimes patients have indiscriminate trust in their GP, which leads them to make this choice even if they suspect their problem to be serious and even if the hospital is nearer to their home than the general practice. One surprising marker of the closeness between patient and physician was the patient's possession of the physician's private telephone number.
Conclusion: Our study shows that, when confronted with a perceived medical emergency, intimacy with the family physician together with the latter's availability seems to be the major reason for the patient choosing the family practitioner's surgery as an entry into the healthcare system.
Background: Multimorbidity is an attractive concept for general practice. An EGPRN working group has defined a comprehensive consensual definition of multimorbidity, translated into 11 European languages and published. It was important to determine if European general practitioners (GPs) recognized this definition and would add some new themes to it.
Research question: How do European GPs perceive and work with the concept of multimorbidity? Is this consistent with the EGPRN definition?
Method: Qualitative surveys designed to achieve maximal variation using focus groups or semi-structured interviews with a purposive sample of GPs in seven European countries. The interview guide was internationally designed and then tested and translated into each language. Data collection and analysis were performed until saturation. The analysis was undertaken from a phenomenological perspective, using a grounded theory based method with four independent researchers and pooling at each coding step for all national teams. Finally, an international team of 10 researchers undertook a pooling of the axial and selective coding of all teams to highlight emerging themes.
Results: Sample's maximal variation was reached in each country with 211 included GPs. Saturation was achieved in each country. The 11 themes describing multimorbidity in the EGPRN definition were recognized in each country. Two new themes (including the Wonca's core competencies and the GP's gut feeling), the dynamic of the doctor–patient relationship for detecting and managing multimorbidity, emerged.
Conclusion: European GPs add the core competencies of GP, the GP's gut feeling and the dynamics of the doctor–patient relationship to the definition of multimorbidity for detecting and managing multimorbidity.
Background: General practice seems to be perceived as less attractive throughout Europe. Most of the policies on the subject focused on negative factors. An EGPRN research team from eight participating countries was created to clarify the positive factors involved in appeals and retention in general practice throughout Europe (WomanPower Study).
Research question: Which positive factors determine the appeal and staying in general practice?
Method: The European team undertook qualitative research in each participating country, with a phenomenological perspective. GPs were selected, using a purposive sampling strategy, until data saturation. Descriptive thematic data analysis was performed. Each participating country did a translation and back translation of the codes. During the Malta and Barcelona EGPRN meetings, the team clarified and compared codes. The final code book and themes were defined in Antwerp (2014).
Results: Eight European code books were pooled in this collaborative research. Positive factors to stay in practice were summarized in the following themes: (1) the GP as a person, (2) special skills or competencies needed in practice, (3) supportive factors for work–life balance, (4) freedom to personalize your work, (5) characteristics of the GP work content, (6) elements of work organization, (7) relationship with other professionals, (8) specific relation with patients, (9) perception of the profession by society, (10) attitudes towards GP, (11) teaching and learning, and (12) positive experiences.
Conclusion: The WomanPower study identified themes for a new positive model of European GP. Crucial is the GP as a person, who needs continuous support and professional development of special competences and wants to have freedom to choose their working environment and organize their practice.
Background: Chronic diseases (CD) are certainly a major challenge both in developed and developing countries. Considering that patient assessment of chronic illness care (PACIC) is the most appropriate instrument to assess the implementation of the chronic care model (CCM), our aim was to adapt and validate the questionnaire in the Romanian context—RO-PACIC (Romanian older patient assessment of chronic illness care).
Research question: Is RO-PACIC a valid instrument for assessing chronic illness care in Romania? How does the medical system in Romania comply with the CCM?
Method: The process of translation and adaptation of a Romanian version of PACIC scale followed the methodology suggested by the World Health Organization, including (1) forward translation, (2) expert panel and back-translation, and (3) pre-testing: cognitive interviewing. A pilot study was conducted on chronically ill persons with one or more chronic condition (n = 45) from Iași and surrounding villages, 55 years or older, who had at least one visit to the doctor in the last six months. Furthermore, we have used confirmatory factor analysis to fit and test the construct structure for each PACIC subscale.
Results: Our pilot study yielded Cronbach alpha coefficients greater than 0.6 for each subscale, suggesting very good internal consistency, and factor loadings generally greater than 0.5, indicating that most of the items fit well into their particular subscale. Overall, the results showed that our approach is suitable and that the final study can be carried out for validating RO-PACIC.
Conclusion: We expect RO-PACIC to be a reliable and valid instrument to assess chronic care in Romania. Furthermore, the preliminary positive correlation between PACIC scores and patient satisfaction proves the importance of CCM for developing policies and quality improvement strategies to enhance the delivery of patient-centred healthcare.
Background: During the ongoing austerity period in Greece, studies regarding the quality of healthcare services in primary healthcare (PHC) could be of major importance. This paper reports on data that has been collected from two independent studies aiming to report evidence on quality in PHC.
Research questions: 1. What types of PHC services are adequate for Greece? 2. What clinical skills are required of the primary care physicians to respond to the population needs? 3. What patient experiences and preferences should the new model satisfy?
Methods: The seven core dimensions that determine strong primary care (1) and elements of the theoretical insights of the work of Barbara Starfield (2009) were utilized as the theoretical background. We combined data from: ‘QUALICOPC study’ (220 General Practitioners (GPs) and 2000 patients of PHC in Greece) and the ‘National Operational Integration (NOI) of PHC Units study’ (124 PHC units in Greece).
Results: GPs reported that they rarely or never participated in treatment and follow-up of certain clinical entities including Chalazion (22.7%) and Parkinson's disease (21.5%).The patients reported that before visiting their GP, almost 50% knew which doctor they would see, felt that they would keep their appointment (34.7%) and that the doctor had read their medical file (29.4%). The patients’ expectations during the consultation were that their doctor would listen to them attentively (68.8%), that they would not feel pressured for time (59.4%), be treated as persons, (57.8%) and be understood (56.7%). The NOI study found that more than 80 out of the 124 PHC units did not integrate with other capacities. Six health centres and five regional clinics reported that medical records were not kept. More than 50% out of the 124 units were not integrated due to efficiency, coordination, governance, continuity and comprehensiveness factors.
Conclusion: Both studies confirm the lack of integration in PHC settings in Greece while clearly indicating areas of quality improvement by taking into account the current performance of GPs’ and patients’ expectations.
REFERENCE
- Kringos D, Boerma W, Bourgueil Y, Cartier T, Dedeu T, Hasvold T, et al. The strength of primary care in Europe: An international comparative study. Br J Gen Pract. 2013;63:e742–e50.
Background: France had an ongoing public interest to child abuse prevention and did pass a Child Protection Reform Act in 2007. Family physicians practical contribution to formal child protection procedure remains scarce.
Research question: This study aimed at exploring the barriers that hinder French family physicians from being actively involved in child protection.
Methods: Two researchers undertook a structured review of field research studies between July 2013 and April 2014. A purposive search was conducted for family physician residents’ theses from 2008; obtained from the two main French thesis-indexing databases. Inclusion criteria were applied. Checklists and various assessment techniques were used to extract data from results sections of theses. The study outcome has resulted in a thematic synthesis.
Results: Major findings highlighted three barriers with practical implications for family physicians in the field: (1) diagnosis stage problems with difficulties assessing complex family situations and psychological obstacles during the decision-making process; (2) reluctance to report instances, underpinned by fear of medical misjudgement, doctor–patient relationship or family structure breakdown; (3) a low level of legislative awareness as well as knowledge of child protection partners’ roles, resulting in a feeling of inadequacy in the child protection network.
Conclusion: Affective and ethical conflicts appeared to be a source of GPs’ vulnerabilities to respond from a legal perspective. Parents’ centred approach to care prevailed over a child perspective. Despite the presence of bias, findings indicated consistencies with international published research studies in primary care settings. GPs’ perceived boundaries were related to their core professionals’ competencies as relationship skills and coordination work.