Abstract
Context: Morus alba L. (Moraceae) is traditionally used for the treatment of urinary incontinency due its strong diuretic properties.
Objective: The present study explores the renal protective effects of M. alba, due to its free radical scavenging properties, in order to provide experimental evidence for its established use.
Materials and methods: Ethanolic extract (200 mg/kg/d) derived from M. alba fruit was employed in rabbits as a co-therapy (GM-al) with gentamicin (80 mg/kg/d) for a period of 3 weeks. Biochemical kidney functioning parameters, urinary isozymes, and histopathological examination were performed.
Results: The results showed that ethanol extract of Morus alba L. prevented alterations in serum creatinine (4.02 ± 0.14, p < 0.0001), blood urea nitrogen (54.18 ± 2.60, p < 0.0001), and serum uric acid levels (2.34 ± 0.12, p < 0.001). However, a decrease in creatinine clearance and urinary volume was observed in experimental groups. Histopathological examination and urinary enzymes excretion also suggested the protective role of the extract.
Discussion and conclusions: The co-administration of M. alba with gentamicin prevented renal functioning alterations expected with the use of gentamicin alone. Therefore, it can be concluded that M. alba to protect from kidney damage, which may be because of its free radical scavenging and diuretic properties.
Introduction
Gentamicin is the most effective bactericidal drug against a wide range of Gram negative micro-organisms with a number of pharmacological, toxicological, and chemical properties (Jawetz, Citation1992). In spite of low resistance (Chow et al., Citation1991), its use is limited due to its nephrotoxic side effects. A large number of studies have been performed in order to counteract nephrotoxic effects of aminoglycosides. These studies have resulted in the identification of a number of neproprotectants including d-glucarate (Furono et al., Citation1976), fosfomycin (Cronin & Newman, Citation1985), and vitamin E (Ademuyiwa et al., Citation1990). However, none of these were clinically applicable probably due to their lower effectiveness.
Morus alba L. (Moraceae) is cultivated in Asian countries as a food for silkworms (Nuengchamnong et al., Citation2007). The plant has long history in Chinese medicine (Zhishen et al., Citation1999). The plant is reported to have anti-inflammatory potential (Chen et al., Citation2013) and possess strong antioxidant properties (Sadighara & Barin, Citation2010). These are also reported to have diuretic, hypotensive, hypoglycemic, antiviral, and bacteriostatic properties (Chu et al., Citation2006). The plant has been used for the treatment of hypertension, diabetes, dizziness, tinnitus, anemia, urinary incontinence, and constipation (Yeung, Citation1985). The active constituents of the plant have been reported to be flavones and their derivatives (Nomura, Citation1988). Most importantly, the plant has been reported to have no harmful effects (Kimura et al., Citation2007), an abundant source of flavonoids (Katsube et al., Citation2006), and the fruits have a tonic effect on the kidney (Duke & Ayensu, Citation1985).
Morus alba fruit was evaluated in the current study for its protective effects against aminoglycosides-induced renal damage due to the presence of a large quantity of flavonoids, and antioxidant and diuretic properties with tonic effects on kidney. The major aim of the study was to increase the clinical applications of aminoglycosides without causing any nephrotoxicity.
Materials and methods
Plant extraction
Sufficient quantity of M. alba fruit was collected from Swabi, Khyber Pakhtunkhwa, Pakistan, after identification by Professor Umar Farooq, Department of Botany, Government College Abbottabad. A voucher specimen (number 1023) was deposited at the herbarium of the same department. The fruits were dried, chopped, and finally powdered. The powdered plant material (3 kg) was extracted with ethanol (70%) for about 20 d with stirring on alternate days. The extract was filtered and evaporated to dryness in a vacuum with the help of a rotary evaporator (R-210, Buchi, Essen, Germany).
Experimental protocol
Healthy male rabbits weighing between 1 and 1.5 kg were maintained on the same diet 15 d prior to initiating the study in 12 h cycles of light and dark, after the approval from Ethical Committee of University of Malakand. Animals were divided in four groups having six animals in each group. All the animals were provided free access to food and water, and were handled and cured according to the rules and regulations of the University of Malakand as well as international laws and policies (National Institutes of Health Guide for the Care of Animals, NIH Publication no. 85-23, 1985). Morus alba L. ethanol extract and gentamicin were employed ().
Table 1. Daily treatment schedule for a period of 3 weeks.
Collection of samples
Blood and urine samples were collected from animals on days 0, 11, and 21 for the estimation of serum urea, serum creatinine, serum uric acid, serum electrolytes, urinary urea, urinary creatinine, urinary protein, and enzymes. Weight and urinary volume were also measured on the same days. Kidneys were isolated on day 21 for histological examination for the presence of any pathogenesis.
Histological exploration of nephrotoxicity
Both the kidneys were isolated and fixed with 10% formalin solution. Tissues were dehydrated with various grades of alcohol and fixed in paraffin wax after clearing with xylene. The solidified tissues were cut into thin pieces less than 3 µm and studied with the help of microscope (Buchi, Essen, Germany) after staining with hematoxylin and eosin dyes (Leong, Citation1994).
Blood urea nitrogen, serum creatinine, creatinine clearance, and serum uric acid level
Blood urea nitrogen and serum creatinine were measured by modified Bertholots indophenol assay and Jaffe reaction, respectively (Smith, Citation1985). Serum uric acid was estimated by commercially available prodia reagent kits while creatinine clearance was calculated by using formula:
Urinary protein excretions and enzymes
Urinary protein excretion was measured with the help of Chemistry analyzer (Power Lab 300, Merck, Darmstadt, Germany) by using reagent kits (DiaSys Diagnostic, Holzheim, Germany) (Johnson et al., Citation1999) while urinary excretion of enzymes, alkaline phosphatase, and lactate dehydrogenase were measured by reagent kits followed by German Society of Clinical Chemistry (Deutsche, Citation1972).
Serum electrolytes
The estimation of serum sodium and serum potassium was performed by using flame photometer while serum calcium was estimated by the Cresolphthalein complexone method (Blosser, Citation1985) by using reagent kits (Randox Laboratories, County Antrim, UK).
Urinary examination
Reagent strips URS-10 (Teco Diagnostic, Amsterdam, The Netherlands) were used for the detection of glucose, ketones, bilirubin, proteins, RBC, WBC, pH, nitrite, specific gravity, and urobilinogen in urine. Urinary microscopic examination was also been performed to authenticate the renal damage.
Statistical analysis
Results were uttered as mean ± standard error of mean (SE). The difference between group G (gentamicin treated) with group C (normal saline treated), GM-al (gentamicin and M. alba treated), and M-al (M. alba treated) were analyzed through one-way analysis of variance by using the Dunnett method with the help of Graphpad prism-5 (Graphpad Inc., La Jolla, CA). The difference was noted significant when the p-value was less than 0.05.
Results
Body weight
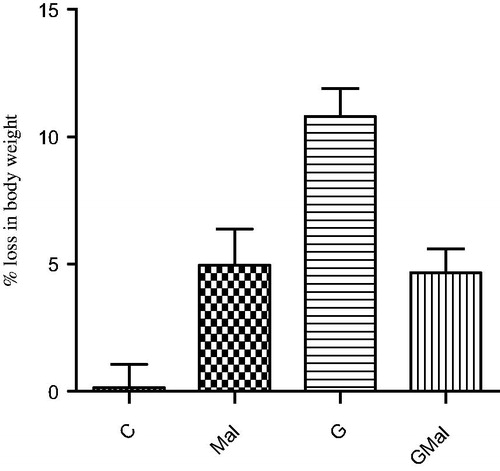
All the experimental animals lost body weight throughout the study duration. The gentamicin-treated group lost 10.795 ± 1.09% of their initial body weight, animals of the control group lost 0.155 ± 0.91%, the GM-al group lost 4.66 ± 0.94%, and the M-al group lost 5.62 ± 1.48% of their body weight. All the groups were found significantly different from the gentamicin-treated group ().
Blood urea nitrogen
Blood urea nitrogen was significantly increased in animals treated with gentamicin on days 11 and 21 of the study period when compared with the control group. Further, blood urea nitrogen of animals treated with co-therapy of gentamicin and M. alba was found to be significantly decreased from animals treated with gentamicin alone ().
Table 2. Different kidney functioning parameters for the assessment of renal damage.
Serum creatinine
Serum creatinine was increased in animals treated with gentamicin in comparison with the control group. However, animals treated with co-therapy of gentamicin and M. alba were found to be significantly decreased from animals treated with gentamicin alone ().
Creatinine clearance
Creatinine clearance was decreased significantly in animals treated with gentamicin alone and in combination with M. alba. It was significantly different from animals of the control group and animals treated with only M. alba ().
Serum uric acid
Serum uric acid remained unchanged in all experimental groups untill day 11 of the study period. However, on the last day, serum uric acid was raised in animals treated with gentamicin to 2.34 ± 0.12 mg/dL, which was significantly different from the control group (1.51 ± 0.02 mg/dL). Animals treated with M. alba alone and in combination with gentamicin were found to be significantly decreased from animals treated with gentamicin ().
Serum electrolytes
Serum sodium remained unchanged in all groups of animals throughout the study period (). A significant decrease in serum potassium was observed in animals treated with gentamicin as 3.43 ± 0.17 mEq/L in comparison with animals of the control group (5.10 ± 0.24 mEq/L). Further, serum potassium level of animals treated with co-therapy of M. alba and gentamicin was also found to be decreased, which were significantly different when compared with animals treated with gentamicin alone. Serum calcium was found to be decreased significantly in animals treated with gentamicin as 7.68 (0.21 mg/dL when compared with control group animals of the control group as 9.72 (0.25 mg/dL. However, animals treated with co-therapy of M. alba and gentamicin were found to be significantly increased from animals treated with gentamicin alone ().
Urinary protein
No significant change in urinary protein excretion was observed in any group on day 11 but it was increased significantly in animals treated with gentamicin on the last day of study, which was significantly different from all other groups ().
Urinary volume
Urinary volume was decreased in animals treated with gentamicin as 126 ± 9.09 mL, which was significantly different from animals of the control group (217 ± 19.77 mL). Further, no significant difference was observed when urinary volume of animals treated with co-therapy of gentamicin and M. alba (142 ± 14.78 mL) was compared with gentamicin-treated animals.
Alkaline phosphatase and lactate dehydrogenase
Alkaline phosphatase remained statistically unchanged in all groups, both on days 11 and 21. No significant difference was observed when gentamicin-treated animals were compared with control group animals ().
Figure 2. Urinary excretions of enzymes on days 11 and 21 of the study period (C, control; MAL, Morus alba; G, gentamicin; GMAL, gentamina and Morus alba).
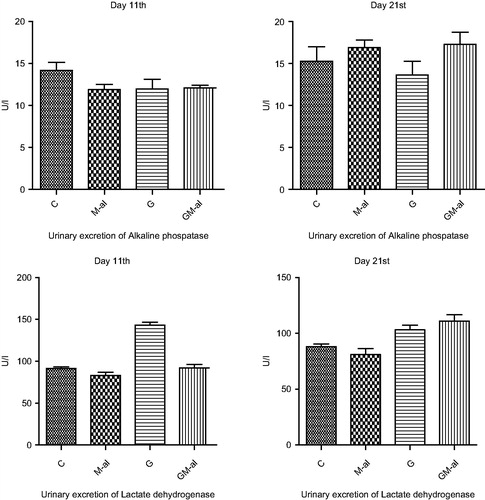
Lactate dehydrogenase excretion was increase significantly on day 11 in animals treated with gentamicin when compared with animals of the control group. However, animals treated with co-therapy of M. alba and gentamicin were found to be significantly different from animals treated with gentamicin alone. Further, only M. alba-treated animals were found to be statistically different from animals treated with gentamicin on day 21 ().
Urinary examination
Microscopic examination of urine of gentamicin-treated animals revealed the presence of significant number of red blood cells, leukocytes, and renal cast, which was considerably different from animals treated with co-therapy of gentamicin and M. alba with an addition of significant number of yeast cells. Yeast cells were also observed in the urine of animals treated with M. alba alone. Urinary reagent examination presented trace amount of nitrite and urobilinogen with the absence of ketones and glucose in all treated groups. However, bilirubin was detected in animals treated with gentamicin and animals of the control group.
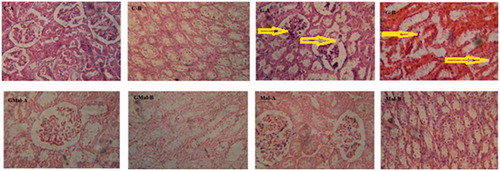
Histological exploration of nephrotoxicity
Animals of the control group presented normal glomeruli and normal tubules with no evidence of necrosis or other significant abnormality ( and ). Animals treated with gentamicin were found have glomerular atropy and proximal tubular necrosis with a large number of ruptured tubules ( and ). Animals treated with co-therapy of gentamicin and M. alba presented some dilated proximal tubules with few ruptured cells. Further, hazy façade with regenerative activities was also present ( and ). Additionally renal cortex of M. alba-treated animals presented normal glomeruli and normal tubules with hyaline-filled lumina ( and ).
Figure 3. Photomicrographs at 100 magnification of the control group; C–A: cortex presenting no major defect, C-B: medulla presenting normal tubules. The gentamicin-treated group, G-A: cortex presenting proximal tubular necrosis, glomerular atropy, G-B: medulla presenting ruptured tubules. Co-therapy of gentamicin and M. alba, GMal-A: cortex presenting dilated proximal tubules with few ruptured cells, GMal-B: medulla presenting hazy façade with regenerative activities. The M. alba-treated group, Mal-A: cortex presenting ordinary glomeruli with usual tubular façade, Mal-B: medulla presenting normal tubules with a some hyaline-packed lumina.
Discussion
Administration of large doses of aminoglycosides has been reported to produce alteration in kidney functioning (Bennett et al., Citation1991). A daily dose of 30–60 mg/kg of gentamicin for about 10 d causes proximal tubular necrosis and significant rise in serum creatinine (Tulkens, Citation1989). To produce nephrotoxicity in experimental animals, a daily dose of 40 and 60 mg/kg has been employed in different researches (Zager, Citation1992). Therefore, a daily dose of 80 mg/kg of gentamicin was selected in the current study to produce significant nephrotoxic effects in experimental animals.
The results obtained in the present investigations revealed an elevation in blood urea nitrogen and serum creatinine with a significant fall in creatinine clearance in gentamicin-treated animals. These results were consistent with those reported previously (Bennett et al., Citation1991) and confirmed the nephrotoxicity associated with aminoglycosides. Further, the concurrent administration of M. alba extract was observed to prevent the rise in serum creatinine, blood urea nitrogen, and serum uric acid; however, it could not protect fall in creatinine clearance.
Elevation of sodium excretion and reduction in re-absorption of potassium has been previously reported with gentamicin (Derakhshanfar et al., Citation2007). It has also been reported that large doses of gentamicin causes hypokalemia (Asif et al., Citation2012). In the current findings, extreme decrease in serum potassium was also observed in gentamicin-treated animals. A small decrease in serum potassium was also noted in the case of animals treated with co-therapy of gentamicin and M. alba but was significantly different from gentamicin-treated animals, which may be due to the depression of sodium/potassium ATPase induced by aminoglycosides (Cronin et al., Citation1982). Extremely significant loss in body weight of animals treated with gentamicin, which was significantly different from animals of the control group and animals treated with co-therapy of gentamicin and M. alba gives declaration of potassium loss (Brinker et al., Citation1981).
An extreme decrease in serum calcium was recorded in gentamicin-treated animals, which was significantly different from animals treated with co-therapy of gentamicin and M. alba. Similar results in animals treated with gentamicin have also been reported previously (Cronin et al., Citation1980). In contrast, gentamicin has also been found to have no effect on serum calcium (Brinker et al., Citation1981). Aminoglycoside causes abnormal urinary excretion of sodium, potassium, calcium, and magnesium (Bennett et al., Citation1991); however, serum sodium was remained statistically unchanged in all groups throughout the study period in the current study.
Serum creatinine and tubular necrosis were reported to be dependent on each other (Solez, Citation1983). The obstruction of tubules through leaking of filtrate from damaged areas may responsible for rise of serum creatinine. Urinary volume was found to be decreased significantly in animals treated with gentamicin and in animals treated with co-therapy of gentamicin and M. alba, which was significantly different from animals of the control group. Urinary protein excretion was found unchanged till day 11 in all the groups. On the last day of the study period, the urinary protein excretion in gentamicin-treated animals was significantly increased when compared with other groups including the control group. This evidence indicates signs of renal damage. Tubular brush border enzymes have also been used for the identification of kidney damage (Furuta & Nakada, Citation1993). Therefore, urinary excretion of lactate dehydrogenase and alkaline phosphatase was studied to confirm nephroprotective properties of M. alba. Alkaline phosphatase was found statistically unchanged throughout the study period. Urinary excretion of lactate dehydrogenase was increased in animals treated with gentamicin on day 11, which showed early detection of renal damage. However, it was decrease on the last day of the study period, may due to their prolong use.
Renal histology of animals treated with gentamicin presented with necrosis, ruptured tubular cells, and glomerular atropy. However, co-therapy of gentamicin and M. alba showed regenerative cells and necrosis which may counteract each other as described previously (Bennett et al., Citation1991; Cronin et al., Citation1980). Granular casts in the animals treated with co-therapy of gentamicin and M. alba may be the most important reason for leaking of protein, which may cause obstruction accountable for the reduction in glomerular filtration and may lead to renal injury (Solez, Citation1983). Animals treated with M. alba extract showed normal glomeruli and tubules with hyaline-filled lumina, which may be due to pinocytotic activity because of salts and proteins. The mechanism but it is not confirmed but not related with considerable cell injury (Thompson et al., Citation1990).
Conclusions
Morus alba successfully prevented renal damage, assessed by measuring blood urea nitrogen, serum creatinine, serum uric acid, urinary enzymes excretion, and histopathological examination.
Declaration of interest
The authors report that they have no conflict of interest. Higher Education Commission, Government of Pakistan, is highly acknowledged for their financial support through indigenous Ph.D. fellowship.
References
- Ademuyiwa O, Nagaha EO, Ubah FO. (1990). Vitamin E and selenium in gentamicin nephrotoxicty. Hum Exp Toxicol 9:281–8
- Asif AH, Rasool ST, Khan TM. (2012). Pyridoxal phosphate a possible intervention to prevent aminoglycoside induced electrolyte imbalance. J Clin Res Bioeth 3:124
- Bennett WM, Elzinga LW, Porter GA. (1991). Tubulo-interstitial disease and toxic nephropathy. In: Brenner BM, Rector FC, eds. The Kidney. Philadelphia: WB Saunders Company, 1430–96
- Blosser N. (1985). Electrolytes. In: Bishop ML, Duben-Von Laufen JL, Fody EP, eds. Clinical Chemistry, Principles, Procedures, Correlations. Philadelphia: JB Lippincott, 263–89
- Brinker KR, Bulger RE, Dobyan DC, et al. (1981). Effect of potassium depletion on gentamicin nephrotoxicity. J Lab Clin Med 98:292–301
- Chen YC, Tien YJ, Chen CH, et al. (2013). Morus alba and active compound oxy-resveratrol exert anti-inflammatory activity via inhibition of leukocyte migration involving MEK/ERK signaling. BMC Complement Altern Med 13:45
- Chow JW, Fine MJ, Shlaes DM, Quinn JP, et al. (1991). Enterobacter bacteremia; clinical features and emergence of antibiotic resistance during therapy. Ann Intern Med 115:585–90
- Chu Q, Lin M, Tian X, Ye J. (2006). Study on capillary electrophoresis-amperometric detection profiles of different parts of M. alba L. J Chromatogr A 1116:286–90
- Cronin RE, Bulger RE, Southern P, Henrich WL. (1980). Natural history of aminoglycoside nephrotoxicity in the dog. J Lab Clin Med 95:463–74
- Cronin RE, Newman JA. (1985). Protective effect of thyroxin but not parathyroidectomy on gentamicin nephrotoxicity. Am J physiol 248:332–9
- Cronin RE, Nix KL, Ferguson ER, et al. (1982). Renal cortex ion composition and Na+-K+-ATPase activity in gentamicin nephrotoxicity. Am J Physiol 242:477–83
- Derakhshanfar A, Bidadkosh A, Kazeminia S. (2007). Vitamin-E protection against gentamicin induced nephrotoxicity in rats: A biochemical and histopathologic study. Iranian J Vet Res 8:231–8
- Deutsche GKC. (1972). Standardisierung von Methoden zur Bestimmung von Enzymaktivitaten in biologischen flussigkeiten (Recommendation of the German Society of Clinical Chemistry. Standardization of methods for measurement of enzymatic activities in biological fluids). Z Klin Chem Klin Biochem 10:182–92
- Duke JA, Ayensu ES. (1985). Medicinal Plants of China. China: Reference Publications Inc., 20–4
- Furono K, Ando K, Suzuki S, Hirata K. (1976). Effect of d-glucarate on basic antibiotics induced renal damage in rats. J Antibiot 29:187–94
- Furuta N, Nakada J. (1993). Study on gamma-GTP activity in urine and renal tissue of drug induced nephrotoxicity in rats. Nippon Hinyokika Gakkai Zasshi 84:1197–205
- Jawetz H. (1992). Aminoglycosides and polymyxins. In: Katzung BG, ed. Basic and Clinical Pharmacology. New York: Appleton and Lang, 645–52
- Johnson AM, Rohlfs EM, Silverman LM. (1999). Proteins. In: Burtis CA, Ashwood ER, eds. Tietz Textbook of Clinical Chemistry. Philadelphia: WB Saunders, 477–540
- Katsube T, Imawaka N, Kawano Y, et al. (2006). Antioxidant flavonol glycosides in mulberry (M. alba L.) leaves isolated based on LDL antioxidant activity. Food Chem 97:25–31
- Kimura T, Nakagawa K, Kubota H, et al. (2007). Food-grade mulberry powder enriched with 1-deoxynojirimycin suppresses the elevation of postprandial blood glucose in humans. J Agric Food Chem 55:5869–74
- Leong ASY. (1994). Fixation and fixatives. In: Woods AE, Ellis RC, eds. Laboratory Histopathology. New York: Churchill Livingstone, 4.1-1/4.2-26
- Nomura T. (1988). Phenolic compounds of the mulberry tree and related plants. Fortschr Chem Org Naturst 53:87–201
- Nuengchamnong N, Ingkaninan K, Kaewruang W, et al. (2007). Quantitative determination of 1-deoxynojirimycin in mulberry leaves using liquid chromatography-tandem mass spectrometry. J Pharm Biomed Anal 44:853–8
- Sadighara P, Barin A. (2010). The study of antioxidant potential of M. alba L. leaves extract. J Herbal Drugs 1:43–6
- Smith ST. (1985). Non protein nitrogen. In: Bishop ML, Duben-Von Laufen JH, Fody EP, eds. Clinical Chemistry, Principles, Procedures, Correlations. Philadelphia: JB Lippincott Company, 411–23
- Solez K. (1983). Pathogenesis of acute renal failure. Int Rev Exp Pathol 24:277–333
- Thompson JR, Simmonsen R, Spindler MA, et al. (1990). Protective effect potassium chloride loading in gentamicin nephrotoxicity. Am J Kidney Dis 15:583–91
- Tulkens PM. (1989). Nephrotoxicity of aminoglycoside antibiotics. Toxicol Lett 46:107–23
- Yeung HC. (1985). Handbook of Chinese Herbs and Formula. Los Angeles: Institute of Chinese Medicine, 320–4
- Zager RA. (1992). Gentamicin effect on renal ischaemia/reperfusion injury. Circ Res 70:20–8
- Zhishen J, Mengcheng T, Jianming W. (1999). The determination of flavonoid contents in mulberry and their scavenging effect on superoxide radicals. Food Chem 64:555–9