Sir,
Facial fillers, injectable therapeutic materials for soft tissue augmentation, are ideal for restoring facial volume and contour. With recognition of its value, as well as the ease of office procedures, filler injection has become one of the most commonly performed cosmetic procedures. Yet, fillers are implants and essentially foreign bodies that can trigger an inflammatory response in individuals. In addition, filler injection is a blind procedure in which the physician is unable to see exactly where the material is placed. With these characteristics, injectable fillers have the potential for a myriad of complications. Moreover, in East Asian countries, injection of illegal materials by unlicensed practitioners are widespread with an increased risk of filler complications. We herein present a case of filler migration to the eyelid, a rare complication following illegal filler injection. To our knowledge, this complication has not been reported previously in the dermatologic literature.
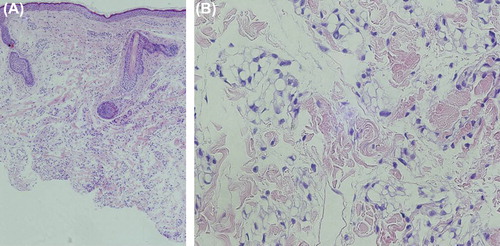
A 74-year-old female presented to the dermatologic outpatient clinic with a history of gradually enlarging swelling on the left upper eyelid. Clinical examination disclosed a yellowish, firm and non-tender mass on the left upper eyelid (). The mass was not associated with decreased visual acuity, ocular motility limitation, or proptosis. The patient stated that she received filler injection on the forehead by an illegal practitioner 3 years ago and the lesion was said to develop a month afterwards. Although our patient recalled the injected material as a liquid agent, she was not able to identify the exact nature of the substance. She denied of being injected in the periorbital region and also of a trauma history. A skin biopsy was performed from the eyelid mass. Histopathologically, there was diffuse granulomatous inflammation throughout the dermis. Under high magnification, numerous lipid vacuoles were seen surrounded by epithelioid histiocytes and multi-nucleated giant cells. The overlying epidermis was intact and unremarkable (). Although we were not able to identify the exact filler substance, the clinical and histological findings were in keeping with the diagnosis of a lipogranuloma from filler migration. The patient was asked to undergo treatment, but is currently lost for follow-up.
Figure 1. (A&B) A 74-year-old female presenting with edema and yellowish discoloration of the left upper eyelid which developed a month after an illegal filler injection to the forehead.
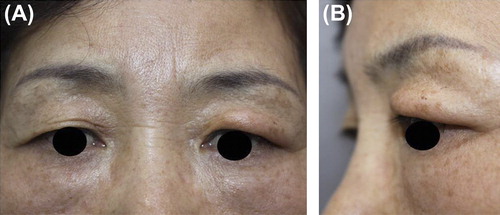
Figure 2. (A) Histopathologically, there was diffuse granulomatous inflammation throughout the dermis (hematoxylin and eosin, × 100). (B) Under high magnification, numerous lipid vacuoles were seen surrounded by epithelioid histiocytes and multi-nucleated giant cells (hematoxylin and eosin, × 400).
Clinically detectable granuloma formation following facial filler injections is a well-known complication, where complication rates vary from 0.01% to 0.1% (Citation1). This is not surprising, as all skin-implanted exogenous substances can trigger an inflammatory response in individuals. Notably, oily substances such as silicone and paraffin have commonly been reported to produce a foreign body granulomatous reaction known as “sclerosing lipogranuloma” (Citation2).
The pathogenesis of eyelid mass formation after filler injection to the forehead can be explained by the consideration of the galea as the superficial musculo-aponeurotic system (Citation1). The layers of the forehead consist of the skin, subcutaneous tissue, frontalis muscle, galea aponeurotica, loose areaolar tissue, and periosteum. The subcutaneous fat layer in the forehead is connected with the brow fat pad, while the galea is connected with the posterior orbicularis fascia. The galea is a broad sheet, and the tissue plane formed by the galea and the posterior orbicularis fascia can function as a migration pathway of the injected material from the forehead to the upper eyelid. Injected filler substances may migrate through the galea aponeurosis and the retroorbicularis fascia by gravity, facial muscle movement and postoperative massage of the injection sites for better distribution of the injected material. Moreover, filler migration can be affected by substance nature, the injection depth, the amount of filler injected and injection technique which is highly dependent on the practitioner. Cases of direct filler migration to the upper eyelid have been very rarely reported (Citation1,Citation3,Citation4). However, the complication may become more common as more dermatologists place the filler more deeply than the subcutaneous tissue plane as Coleman originally described. Needless to say, illegal filler injection by an inexperienced, non-qualified person is prone to cause filler migration and is expected to cause great problem in East Asian Countries, where such procedures are widespread.
Local steroid injection or oral steroids, as well as anti-inflammatory and anti-mitotic drugs such as minocycline and 5-FU, have been used for the treatment of foreign body granuloma. However, it is felt that an appropriate surgical excision is the treatment of choice in many cases (Citation5). In the previously mentioned cases with filler migration to the upper eyelid, surgical excision was performed on both diagnoses and treatment purposes (Citation1,Citation3,Citation4).
With the increasing use of facial fillers in the community, the migrated filler could become an important differential diagnosis for periocular swellings in future. This case highlights the importance of a detailed history on cosmetic procedures. Last but not least, dermatologists should be vigilant about the various complications associated with fillers and be equipped to treat the complications when they do arise. It is also equally important that physicians advocate patients to see reputable physicians who use FDA-approved, purified products for an injection.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Sa HK, Woo KI, Suh YL, Kim YD. Periorbital lipogranuloma: a previously unknown complication of autologous fat injections for facial augmentation. Br J Opthalmol. 2011;95: 1259–1263.
- Sinrachtanant C, Tantinikorn W, Warnnissorn M, Assanasen P. Sclerosing lipogranuloma of the nose: a new treatment using adipose tissue transplantation. Facial Plast Surg. 2003; 19:363–367.
- Malik S, Mehta P, Adesanya O, Ahluwalia HS. Migrated peiocular filler masquerading as arteriovenous malformation: a diagnostic and therapeutic dilemma. Ophthal Plast Reconstr Surg. 2013;29:18–20.
- Lee MJ, Sung MS, Kim NJ, Choung HK, Khwarg SI. Eyelid mass secondary to injection of calcium hydroxylapatite facial filler. Opthal Plast Reconstr Surg. 2008;24:421–423.
- Park TH, Seo SW, Kim JK, Chang CH. Clinical outcome in a series of 173 cases of foreign body granuloma: improved outcomes with a novel surgical technique. J Plast Reconstr Aesthet Surg. 2012;65:29–34.
