Abstract
Objective. Adiponectin, an anti-inflammatory and anti-diabetogenic adipokine, has an important regulatory effect on both the innate and adaptive limbs of the immune response. The objective of this study was to determine whether adiponectin is present in amniotic fluid (AF) and if its concentration changes with gestational age, in the presence of labor, and in the presence of intra-amniotic infection (IAI) in patients with spontaneous preterm labor (PTL) and intact membranes.
Study design. This cross-sectional study included 468 patients in the following groups: (1) women in the mid-trimester of pregnancy (14–18 weeks) who underwent amniocentesis for genetic indications and delivered a normal neonate at term (n = 52); (2) normal pregnant women at term with (n = 49) and without (n = 41) spontaneous labor; (3) patients with an episode of PTL and intact membranes who were classified into: (a) PTL who delivered at term (n = 149); (b) PTL who delivered preterm (<37 weeks gestation) without IAI (n = 108); and (c) PTL with IAI (n = 69). Adiponectin concentration in AF was determined by ELISA.
Results. (1) The median AF adiponectin concentration at term was significantly higher than in the mid-trimester (35.6 ng/ml, interquartile range [IQR] 26.4–52.7 vs. 29.9 ng/ml, IQR 19.9–35.2; p = 0.01); (2) among women with PTL and intact membranes, the median AF adiponectin concentration was significantly higher in patients with IAI than in those without IAI who delivered either at term (54.3 ng/ml, 39.0–91.8 vs. 50.1 ng/ml, 33.2–72.8; p = 0.02) or preterm (47.6 ng/ml, 32.6–74.6; p = 0.01); and (3) among women at term, there was no significant difference in the median AF adiponectin concentration between those with and without labor (33.7 ng/ml, IQR 21.7–53.9 vs. 35.6 ng/ml, IQR 26.4–52.7; respectively p = 0.5).
Conclusions. (1) Adiponectin is a physiologic constituent of AF; and (2) adiponectin concentrations in AF are increased significantly with advancing gestation and in the presence of IAI. Collectively, these findings suggest that adiponectin plays a dynamic role in normal gestation and in the presence of IAI.
Introduction
Spontaneous preterm parturition is syndromic in nature [Citation1,Citation2]. Consistent with this view, several mechanisms of disease have been implicated in the pathogenesis of this condition, including intra-amniotic infection/inflammation (IAI) [Citation3–9], uteroplacental ischemia [Citation10–12], uterine overdistention [Citation13,Citation14], allergic reactions [Citation15,Citation16], cervical insufficiency [Citation2,Citation17–19], hormonal disorders [Citation20] and others. Despite the strong experimental and epidemiologic evidence suggesting an association between the aforementioned etiological factors and spontaneous preterm parturition, intra-amniotic infection/inflammation is the only pathological process for which a solid body of evidence supports a cause–effect relationship with preterm parturition [Citation9,Citation21].
The mechanism by which microbial invasion of the amniotic cavity (MIAC) and intra-amniotic inflammation induce preterm parturition involves the production and secretion of a wide range of pro-inflammatory cytokines [Citation2,Citation22–29]. These cytokines and chemokines include: interleukin (IL)- 1 [Citation30–36], IL-6 [Citation35,Citation37–41], tumor necrosis factor (TNF)-α, [Citation34,Citation35,Citation42–47], IL-18 [Citation48], 1L-16 [Citation49], IL-8 [Citation50,Citation51], colony-stimulating factors [Citation52], macrophage migration inhibitory factor [Citation53], monocyte chemotactic protein-1 (MCP-1) [Citation54], macrophage inflammatory protein-1α (MIP-1α) [Citation55], RANTES [Citation56], epithelial cell-derived neutrophil-activating peptide-78 [Citation57], CXCL6 [Citation58], CXCL13 [Citation59], and CCL20 [Citation60]. Several lines of evidence support the causal link between cytokines and prematurity: (1) exposure of human decidua to bacterial products results in increased production of IL-1, IL-6, and TNF-α [Citation47,Citation61,Citation62]; (2) TNF-α, [Citation63,Citation64], IL-1 [Citation63,Citation65], and IL-1β [Citation66,Citation67] can stimulate uterine contractility by induction of prostaglandin production [Citation65,Citation68]; (3) matrix metalloproteinases (MMPs) have been implicated in membrane rupture [Citation69–71] and cervical ripening [Citation72]. TNF-α can stimulate MMPs production [Citation72]; (4) administration of IL-1 can induce preterm labor (PTL) and preterm birth in pregnant mice [Citation36]. Moreover, treatment of these mice with the natural antagonist of IL-1 (IL-1 receptor antagonist) abrogates preterm parturition [Citation32]; (5) amniotic fluid (AF) concentrations of immunoreactive IL-1 [Citation30,Citation33], TNF-α [Citation42,Citation43,Citation45,Citation61], IL-6 [Citation37,Citation38,Citation41,Citation73,Citation74], IL-18 [Citation48], IL-16 [Citation49], IL-8 [Citation50,Citation51], MCP-1 [Citation54], MIP-1α [Citation55], RANTES [Citation56] are elevated in women with PTL in the presence of infection and/or inflammation.
Adiponectin is a member of a growing group of peptides and proteins secreted by adipose tissue, termed adipocytokines [Citation75]. Some of these active molecules are produced mainly by adipose tissue (e.g. leptin [Citation76], adiponectin [Citation77]), whereas others are shared with other systems (e.g. TNF-α [Citation78], IL-6 [Citation79]). Adiponectin, identified independently by four groups [Citation80–83] took position as an important adipocytokine with a wide range of biological actions including insulin-sensitizing [Citation84], anti-atherogenic [Citation85], and angiogenic [Citation86] properties. In addition to its well-established role in glucose metabolism and regulation of vasculature, adiponectin also has a potent anti-inflammatory effect [Citation87].
Despite its pleiotropic effects on metabolism, inflammatory, and immune responses, only one report concerning AF concentrations of this adipocytokine has been published [Citation88]. Moreover, no data exist regarding AF concentrations of adiponectin in patients at term, or in labor (either term or preterm). Thus, the objective of this study was to determine whether adiponectin is present in AF and if its concentration changes with gestational age, in the presence of labor and in the presence of intra-amniotic infection (IAI) in patients with spontaneous PTL and intact membranes.
Materials and methods
Study design and population
A cross-sectional study was conducted by searching our clinical database and bank of biological samples and included 468 patients in the following groups: (1) women in the mid-trimester of pregnancy (14–18 weeks) who underwent amniocentesis for genetic indications and delivered a normal neonate at term (n = 52); (2) normal pregnant women at term with (n = 49) and without (n = 41) spontaneous labor; (3) patients with an episode of PTL and intact membranes who were classified into: (a) PTL who delivered at term (n = 149); (b) PTL who delivered preterm (<37 weeks gestation) without IAI (n = 108); and (c) PTL with IAI (n = 69).
All participating women provided written informed consent prior to the collection of AF. The collection and utilization of AF for research purposes was approved by the Institutional Review Boards of the participant institutions and the Eunice Kennedy Shriver National Institute of Child Health and Human Development, NIH, DHHS. Many of these samples have been previously used to study the biology of inflammation, hemostasis, and growth factor concentrations in normal pregnant women and those with pregnancy complications.
Definitions
Patients were considered to have a normal pregnancy outcome if they did not have any medical, obstetrical, or surgical complication, and delivered a term neonate (≥37 weeks) of appropriate birth weight for gestational age [Citation89,Citation90] without complications. Spontaneous PTL was defined by the presence of regular uterine contractions occurring at a frequency of at least two every 10 min associated with cervical change before 37 completed weeks of gestation that required hospitalization. IAI was defined as a positive AF culture for micro-organisms. Intra-amniotic inflammation was diagnosed by an AF IL-6 concentration ≥2.6 ng/ml [Citation91].
Sample collection
AF samples were obtained by transabdominal amniocentesis performed for genetic indication, evaluation of microbial status of the amniotic cavity, and/or assessment of fetal lung maturity in patients approaching term. Women at term in labor consisted of women who were admitted for suspected PTL because of uncertain dates and had an amniocentesis for the assessment of fetal lung maturity. The criteria for considering that these patients were at term in labor was derived retrospectively if the following criteria were met: (1) spontaneous labor; (2) delivery within 24 h from amniocentesis; (3) analysis of AF consistent with maturity; (4) birthweight >2500 g; (5) absence of respiratory distress syndrome or other complications of prematurity; and (6) physical examination of the newborn by pediatricians consistent with a term neonate. Samples of AF were transported to the laboratory in a sterile capped syringe and cultured for aerobic/anaerobic bacteria and genital mycoplasmas. White blood cell (WBC) count, glucose concentration, and Gram-stain were also performed shortly after collection as previously described [Citation92–94]. The results of these tests were used for clinical management. AF IL-6 concentrations were used only for research purposes. AF not required for clinical assessment was centrifuged for 10 min at 4°C and the supernatant was aliquoted and stored at −70°C until analysis.
The correlation between AF adiponectin concentrations and maternal age, BMI, AF WBC count, AF concentrations of glucose and IL-6 as well as with birthweight was determined among patients with spontaneous PTL with intact membranes who delivered within 48 h. The 48 h interval was chosen to preserve a meaningful temporal relationship between AF adiponectin concentration and AF concentrations of glucose, IL-6 as well as with birthweight.
Determination of human adiponectin concentration in amniotic fluid
Specific and sensitive enzyme-linked immunoassays were used to determine concentrations of adiponectin in human AF. Immunoassays for human adiponectin were purchased from Linco Research (Human Adiponectin ELISA, LINCO Research, St Charles, MO). Adiponectin assays were validated for use in human AF in our laboratory prior to their use in this study. The calculated inter-assay and intra-assay coefficients of variation for resistin in our laboratory were 1.6% and 3.4%, respectively. The sensitivity was 0.47 ng/ml.
Statistical analysis
The normality of the data was tested using the Shapiro–Wilk and Kolmogorov–Smirnov tests. Because AF adiponectin concentrations were not normally distributed, non-parametric tests were used for analyses. Comparisons between proportions were performed with the Chi-square test. Kruskal–Wallis with post-hoc analysis and Mann–Whitney U tests were used for continuous variables. Adjustment for multiple comparisons was performed using the Bonferroni method. Spearman rank correlation was utilized to assess correlations between AF concentration of adiponectin, WBC count and IL-6. A p-value of 0.05 was considered statistically significant. The statistical package used was SPSS v.14.0 (SPSS, Chicago, IL).
Results
Demographic and clinical characteristics of the study population
presents the demographic and clinical characteristics of patients in the mid-trimester, term not in labor and term in labor groups. displays the demographic and clinical characteristics of patients with spontaneous PTL and intact membranes. Among patients with PTL, those with IAI had a significantly lower median gestational age at amniocentesis than those without IAI who delivered preterm and those who delivered at term ().
Table I. Demographic and clinical characteristics of patients in the mid-trimester and those at term with and without spontaneous labor.
Table II. Demographic and clinical characteristics of patients presenting with spontaneous preterm labor with intact membranes.
Amniotic fluid adiponectin concentrations in themid-trimester and at term
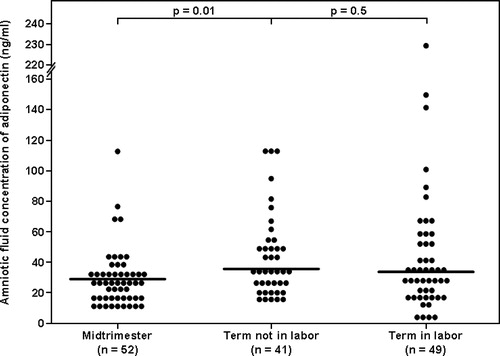
The median AF concentration of adiponectin was significantly higher in patients at term not in labor than in those in the mid-trimester of pregnancy (35.6 ng/ml, interquartile range [IQR] 26.4–52.7 vs. 29.9 ng/ml, IQR 19.9–35.2; p = 0.01, ). Among women at term, there was no significant difference in the median AF adiponectin concentration between those with and without labor (33.7 ng/ml, IQR 21.7–53.9 vs. 35.6 ng/ml, IQR 26.4–52.7; respectively p = 0.5, ).
Figure 1. Amniotic fluid adiponectin concentrations in women with a normal pregnancy in the mid-trimester and in those at term not in labor. The median amniotic fluid concentration of adiponectin was significantly lower in the mid-trimester than at term. Among women at term, there was no significant difference in the median amniotic fluid concentration of adiponectin between patient in labor and those not in labor.
Amniotic fluid adiponectin concentrations in spontaneous preterm labor and intact membranes
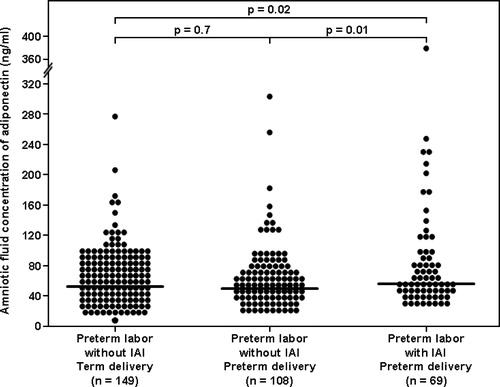
Among women with PTL and intact membranes, the median AF adiponectin concentration was significantly higher in patients with IAI than in those without IAI who delivered either at term (54.3 ng/ml, 39.0–91.8 vs. 50.1 ng/ml, 33.2–72.8; p = 0.02, ) or preterm (54.3 ng/ml, 39.0–91.8 vs. 47.6 ng/ml, 32.6–74.6; p = 0.01, ). Among women with PTL without IAI, no significant difference was found in the median AF concentration of adiponectin between women who delivered at term and those who delivered preterm (p = 0.7, ).
Figure 2. Amniotic fluid concentration of adiponectin in women with spontaneous preterm labor and intact membranes. Among women with preterm labor and intact membranes, the median amniotic fluid adiponectin concentration was significantly higher in patients with IAI than in those without IAI who delivered either at term or preterm.
Amniotic fluid adiponectin concentrations and intra-amniotic infection/inflammation
AF adiponectin concentrations correlated with AF WBC count (Spearman rho coefficient: 0.26, p = 0.01), AF concentrations of glucose concentration (r = −0.37, p = 0.002) and IL-6 (r = 0.34, p < 0.001).
Discussion
Principal findings of the study
(1) Adiponectin is a constituent of the AF; (2) the median AF concentration of adiponectin is higher at term that in the mid-trimester; (3) among women with spontaneous PTL and intact membranes, those with IAI had a significantly higher median AF adiponectin concentration than those without IAI who delivered either at term or preterm; (4) AF adiponectin concentrations were positively correlated with AF WBC count and IL-6 concentrations; and (5) AF adiponectin concentrations were negatively correlated with AF glucose concentrations.
Adiponectin is a potent anti-inflammatory adipocytokine
In addition to its well-established role in metabolic regulation, adiponectin has emerged as a potent anti-inflammatory adipocytokine. The evidence in support of this view includes: (1) adiponectin induces production of anti-inflammatory cytokines (IL-10, IL-1 receptor antagonist [Citation95]) by human monocytes, macrophages and dendritic cells; (2) adiponectin suppresses macrophage production of pro-inflammatory cytokines (TNF-α [Citation96], interferon-γ [Citation95], IL-6) and mitigates their phagocytic activity in response to stimulation with lipopolysaccharide (LPS) [Citation97]; (3) adiponectin abates T-cell ability to evoke an allogenic T-cell response [Citation95]; (4) adiponectin inhibits activation of the nuclear transcription factor NF-κB in endothelial cells [Citation98]; and (5) alterations in adiponectin concentrations characterize systemic inflammatory conditions such as overweight/obesity [Citation99,Citation100] insulin resistance [Citation101] and systemic lupus erythematosus [Citation102]. The importance of adiponectin in major metabolic pathways, as well as in the innate and adaptive limbs of the immune response suggests that this adipocytokine plays a role in the regulation of the intricate interface between inflammation and metabolism.
Adiponectin and human pregnancy
Congruent with studies in non-pregnant individuals, adiponectin has been implicated in the metabolic adaptations to gestation [Citation103–105], as well as in complications of pregnancy such as gestational diabetes mellitus (GDM) [Citation106,Citation107] and preeclampsia [Citation108–113]. Indeed, the importance of adiponectin in human pregnancy has been corroborated in the following reports: (1) normal pregnancy is associated with alterations in circulating adiponectin [Citation104,Citation114–118]; (2) circulating maternal adiponectin correlates with insulin resistance indices during pregnancy [Citation103,Citation119,Citation120]; (3) GDM is associated with decreased maternal concentrations of adiponectin as compared to normal pregnant women [Citation120–123]; (4) overweight pregnant women have a lower plasma concentration of adiponectin [Citation124,Citation125] than non-obese pregnant women; and (5) preeclampsia is associated with altered maternal circulating adiponectin [Citation126–130].
Adiponectin is a physiological component of the amniotic fluid
Adiponectin was detected in the AF of all patients included in this study, from the early second trimester until 42 weeks of gestation, suggesting that adiponectin is a physiologic component of human AF. This is a novel finding. AF adiponectin concentrations were determined in only one study [Citation88]. Baviera et al. [Citation88], reported the presence of adiponectin in 50 normal pregnant patients between 15 and 18 weeks of gestation. The results of the current study are in agreement with the latter study. In both studies, adiponectin was detected in all samples. Moreover, the mean and IQR of patients in mid-trimester are remarkably similar: 29.0 ng/ml, 19.9–35.2 in the present study and 26.8 ng/ml, 13.9–37.3 ng/ml in the study conducted by Baviera et al [Citation88]. The results reported herein extend our knowledge by demonstrating that adiponectin is present in AF in a wide range of gestational ages, at term and during preterm and term labor. Moreover, we were able to report higher AF adiponectin concentrations with advancing gestation and in the presence of IAI.
Our findings characterize adiponectin as a novel physiologic constituent of AF. Adiponectin is argued to be produced exclusively by adipocytes. Thus, its presence in AF deserves comment. A possible explanation could be a contamination from the maternal and fetal circulation. However, this possibility is highly unlikely from the following reasons: (1) contamination at the time of amniocentesis is rare, with maternal origin ranging from 0.3 to 10.8%, whereas fetal injury rates range between 0.6 and 2% [Citation131]. Of note, these data were obtained from a review that was published before the widespread use of ultrasound. Adiponectin was detected in all samples in the present report as well as in the study by Baviera et al [Citation88]; (2) adiponectin concentrations are higher in the presence of IAI and correlate with AF WBC count IL-6 and glucose concentrations; and (3) the mean and IQR of AF adiponectin concentration of patients in mid-trimester are remarkably similar in the present study and the one conducted by Baviera et al. [Citation88]. Collectively, these data strongly suggest that adiponectin is a genuine component of AF and its presence in that compartment cannot be attributed to contamination by maternal or fetal blood.
High amniotic fluid concentrations of adiponectin at term and in the presence of intra-amniotic infection: possible ontology and etiology
The presence of adiponectin in AF is an intriguing finding since it has been argued that this adipokine is produced exclusively by adipocytes. Nevertheless, adiponectin have been detected in other body fluids including synovial [Citation132], cerebrospinal [Citation133,Citation134], peritoneal [Citation135], saliva [Citation136], and urine [Citation102,Citation137]. Thus, although the source for AF adiponectin remains unknown, putative origins include fetal urine and fetal membranes.
Several lines of evidence support fetal urine as a source for AF adiponectin. Circulating fetal adiponectin concentrations are very high [Citation114,Citation115,Citation118,Citation138,Citation139]. Indeed, they are two-to-four fold higher than the adults population [Citation104,Citation115,Citation118]. Since adiponectin is secreted in the urine [Citation102,Citation137] (in its native conformation [Citation140]) it is conceivable that AF adiponectin originate from fetal urine. Moreover, term newborns have higher circulating adiponectin than preterm neonates [Citation141,Citation142]. Thus, the higher median AF concentrations of adiponectin at term than in mid trimester reported herein, can be explained by higher urine adiponectin in mature fetuses. Finally, fetal urine origin of adiponectin can also account for the higher AF adiponectin in the presence of IAI. Renal dysfunction is associated with increased urinary adiponectin secretion [Citation102,Citation137]. Fetal renal insult has been associated with IAI inflammation [Citation143,Citation144]. Taken together, it is possible that renal dysfunction in fetuses affected by the inflammatory process results in increased fetal urine adiponectin concentration which in turn leads to high AF adiponectin.
An additional explanation for the presence of adiponectin in the AF could be the production and secretion by the fetal membranes. Lappas et al. [Citation145] have demonstrated an ex-vivo secretion of adiponectin by human amnion. Consistent with the findings of the latter report, we have recently found mRNA expression of adiponectin in human amnion [Citation146]. In addition, adiponectin was detected in the AF as early as the 15th week of gestation, at which period the major contribution for AF is not the fetal urine. Collectively, these data strongly suggest that the amnion is a source for AF adiponectin. Secretion of adiponectin by the amnion can account for the higher concentrations at term since the surface area of the amnion is significantly larger at term than in the mid trimester. Finally, pathway analysis of human amnion gene expression identified adipocytokine signaling pathway as one of the signaling pathways associated with labor, which is an inflammatory process [Citation147]. Thus, it is tempting to suggest that the increased of AF adiponectin in the presence of IAI is regulated by the amnion. Further studies will be needed to establish the intriguing relationship between the amnion and adiponectin in the context of IAI. These putative sources of adiponectin, i.e. fetal urine and amnion and the suggested explanations for the increased adiponectin at term and in the presence of IAI are not necessarily mutually exclusive and it is possible that both are involved in the regulation of adiponectin.
In conclusion, this is the first study describing the presence of adiponectin in AF of term and preterm women and its association with IAI. These observations are in line with, and lend credence to, our previous studies that suggest an association between AF adipokines and IAI [Citation148–150]. Collectively, these novel findings suggest that adipokines play a dynamic, and hitherto unrecognized role in both normal gestation and in IAI. Concomitantly, the source of AF adiponectin is unknown. Identification of AF origin is of major importance in order to further elucidate the interaction between the IAI, adiponectin and fetal–placental compartments.
Acknowledgement
This work was supported by the Intramural Research Program of the Eunice Kennedy Shriver National Institute of Child Health and Human Development, NIH, DHHS.
References
- Romero R, Mazor M. Infection and preterm labor. Clin Obstet Gynecol 1988;31:553–584.
- Romero R, Espinoza J, Kusanovic JP, Gotsch F, Hassan S, Erez O, Chaiworapongsa T, Mazor M. The preterm parturition syndrome. BJOG 2006;113(Suppl 3):17–42.
- Romero R, Mazor M. Infection and preterm labor. Clin Obstet Gynecol 1988;31:553–584.
- Gibbs RS, Romero R, Hillier SL, Eschenbach DA, Sweet RL. A review of premature birth and subclinical infection. Am J Obstet Gynecol 1992;166:1515–1528.
- Goldenberg RL, Hauth JC, Andrews WW. Intrauterine infection and preterm delivery. N Engl J Med 2000;342:1500–1507.
- Ledger WJ. Infection and premature labor. Am J Perinatol 1989;6:234–236.
- Romero R, Mazor M, Wu YK, Sirtori M, Oyarzun E, Mitchell MD, Hobbins JC. Infection in the pathogenesis of preterm labor. Semin Perinatol 1988;12:262–279.
- Goncalves LF, Chaiworapongsa T, Romero R. Intrauterine infection and prematurity. Ment Retard Dev Disabil Res Rev 2002;8:3–13.
- Hirsch E, Wang H. The molecular pathophysiology of bacterially induced preterm labor: insights from the murine model. J Soc Gynecol Investig 2005;12:145–155.
- Arias F, Rodriquez L, Rayne SC, Kraus FT. Maternal placental vasculopathy and infection: two distinct subgroups among patients with preterm labor and preterm ruptured membranes. Am J Obstet Gynecol 1993;168:585–591.
- Kim YM, Chaiworapongsa T, Gomez R, Bujold E, Yoon BH, Rotmensch S, Thaler HT, Romero R. Failure of physiologic transformation of the spiral arteries in the placental bed in preterm premature rupture of membranes. Am J Obstet Gynecol 2002;187:1137–1142.
- Kim YM, Bujold E, Chaiworapongsa T, Gomez R, Yoon BH, Thaler HT, Rotmensch S, Romero R. Failure of physiologic transformation of the spiral arteries in patients with preterm labor and intact membranes. Am J Obstet Gynecol 2003;189:1063–1069.
- Hill LM, Breckle R, Thomas ML, Fries JK. Polyhydramnios: ultrasonically detected prevalence and neonatal outcome. Obstet Gynecol 1987;69:21–25.
- Ludmir J, Samuels P, Brooks S, Mennuti MT. Pregnancy outcome of patients with uncorrected uterine anomalies managed in a high-risk obstetric setting. Obstet Gynecol 1990;75:906–910.
- Bytautiene E, Romero R, Vedernikov YP, El-Zeky F, Saade GR, Garfield RE. Induction of premature labor and delivery by allergic reaction and prevention by histamine H1 receptor antagonist. Am J Obstet Gynecol 2004;191:1356–1361.
- Romero R, Mazor M, Avila C, et al Uterine “allergy”: a novel mechanism for preterm labor. Am J Obstet Gynecol 1991;164:375.
- Romero R, Espinoza J, Erez O, Hassan S. The role of cervical cerclage in obstetric practice: can the patient who could benefit from this procedure be identified? Am J Obstet Gynecol 2006;194:1–9.
- Mazaki-Tovi S, Romero R, Kusanovic JP, Erez O, Pineles BL, Gotsch F, Mittal P, Than NG, Espinoza J, Hassan SS. Recurrent preterm birth. Semin Perinatol 2007;31:142–158.
- Lee SE, Romero R, Park CW, Jun JK, Yoon BH. The frequency and significance of intraamniotic inflammation in patients with cervical insufficiency. Am J Obstet Gynecol 2008;198:633–638.
- Check JH, Lee G, Epstein R, Vetter B. Increased rate of preterm deliveries in untreated women with luteal phase deficiencies. Preliminary report. Gynecol Obstet Invest 1992;33:183–184.
- Romero R, Gomez R, Mazor M, Ghezzi F, Yoon BH. The preterm labor syndrome. 1997;29–49.
- Gotsch F, Romero R, Kusanovic JP, Mazaki-Tovi S, Pineles BL, Erez O, Espinoza J, Hassan SS. The fetal inflammatory response syndrome. Clin Obstet Gynecol 2007;50:652–683.
- Challis JR, Lye SJ, Gibb W, Whittle W, Patel F, Alfaidy N. Understanding preterm labor. Ann N Y Acad Sci 2001;943:225–234.
- Gibbs RS, Romero R, Hillier SL, Eschenbach DA, Sweet RL. A review of premature birth and subclinical infection. Am J Obstet Gynecol 1992;166:1515–1528.
- Goldenberg RL, Andrews WW, Hauth JC. Choriodecidual infection and preterm birth. Nutr Rev 2002;60:S19–S25.
- Gomez R, Ghezzi F, Romero R, Munoz H, Tolosa JE, Rojas I. Premature labor and intra-amniotic infection. Clinical aspects and role of the cytokines in diagnosis and pathophysiology. Clin Perinatol 1995;22:281–342.
- Romero R, Espinoza J, Mazor M, Chaiworapongsa T. The preterm parturition syndrome. 2004;28–60.
- Romero R, Mazor M, Wu YK, Sirtori M, Oyarzun E, Mitchell MD, Hobbins JC. Infection in the pathogenesis of preterm labor. Semin Perinatol 1988;12:262–279.
- Romero R, Espinoza J, Mazor M. Can endometrial infection/inflammation explain implantation failure, spontaneous abortion, and preterm birth after in vitro fertilization? Fertil Steril 2004;82:799–804.
- Romero R, Brody DT, Oyarzun E, Mazor M, Wu YK, Hobbins JC, Durum SK. Infection and labor. III. Interleukin-1: a signal for the onset of parturition. Am J Obstet Gynecol 1989;160:1117–1123.
- Romero R, Sepulveda W, Mazor M, Brandt F, Cotton DB, Dinarello CA, Mitchell MD. The natural interleukin-1 receptor antagonist in term and preterm parturition. Am J Obstet Gynecol 1992;167:863–872.
- Romero R, Tartakovsky B. The natural interleukin-1 receptor antagonist prevents interleukin-1-induced preterm delivery in mice. Am J Obstet Gynecol 1992;167:1041–1045.
- Romero R, Mazor M, Brandt F, Sepulveda W, Avila C, Cotton DB, Dinarello CA. Interleukin-1 alpha and interleukin-1 beta in preterm and term human parturition. Am J Reprod Immunol 1992;27:117–123.
- Bry K, Hallman M. Transforming growth factor-beta 2 prevents preterm delivery induced by interleukin-1 alpha and tumor necrosis factor-alpha in the rabbit. Am J Obstet Gynecol 1993;168:1318–1322.
- Fidel PL, Jr., Romero R, Wolf N, Cutright J, Ramirez M, Araneda H, Cotton DB. Systemic and local cytokine profiles in endotoxin-induced preterm parturition in mice. Am J Obstet Gynecol 1994;170:1467–1475.
- Romero R, Mazor M, Tartakovsky B. Systemic administration of interleukin-1 induces preterm parturition in mice. Am J Obstet Gynecol 1991;165:969–971.
- Romero R, Sepulveda W, Kenney JS, Archer LE, Allison AC, Sehgal PB. Interleukin 6 determination in the detection of microbial invasion of the amniotic cavity. Ciba Found Symp 1992;167:205–220.
- Romero R, Yoon BH, Kenney JS, Gomez R, Allison AC, Sehgal PB. Amniotic fluid interleukin-6 determinations are of diagnostic and prognostic value in preterm labor. Am J Reprod Immunol 1993;30:167–183.
- Hillier SL, Witkin SS, Krohn MA, Watts DH, Kiviat NB, Eschenbach DA. The relationship of amniotic fluid cytokines and preterm delivery amniotic fluid infection, histologic chorioamnionitis, and chorioamnion infection. Obstet Gynecol 1993;81:941–948.
- Gomez R, Romero R, Galasso M, Behnke E, Insunza A, Cotton DB. The value of amniotic fluid interleukin-6, white blood cell count, and gram stain in the diagnosis of microbial invasion of the amniotic cavity in patients at term. Am J Reprod Immunol 1994;32:200–210.
- Romero R, Avila C, Santhanam U, Sehgal PB. Amniotic fluid interleukin 6 in preterm labor. Association with infection. J Clin Invest 1990;85:1392–1400.
- Romero R, Manogue KR, Mitchell MD, Wu YK, Oyarzun E, Hobbins JC, Cerami A. Infection and labor. IV. Cachectin-tumor necrosis factor in the amniotic fluid of women with intraamniotic infection and preterm labor. Am J Obstet Gynecol 1989;161:336–341.
- Romero R, Mazor M, Sepulveda W, Avila C, Copeland D, Williams J. Tumor necrosis factor in preterm and term labor. Am J Obstet Gynecol 1992;166:1576–1587.
- Baumann P, Romero R, Berry S, Gomez R, McFarlin B, Araneda H, Cotton DB, Fidel P. Evidence of participation of the soluble tumor necrosis factor receptor I in the host response to intrauterine infection in preterm labor. Am J Reprod Immunol 1993;30:184–193.
- Maymon E, Ghezzi F, Edwin SS, Mazor M, Yoon BH, Gomez R, Romero R. The tumor necrosis factor alpha and its soluble receptor profile in term and preterm parturition. Am J Obstet Gynecol 1999;181:1142–1148.
- Romero R, Mazor M, Wu YK, Sirtori M, Oyarzun E, Mitchell MD, Hobbins JC. Infection in the pathogenesis of preterm labor. Semin Perinatol 1988;12:262–279.
- Romero R, Mazor M, Manogue K, Oyarzun E, Cerami A. Human decidua: a source of cachectin-tumor necrosis factor. Eur J Obstet Gynecol Reprod Biol 1991;41:123–127.
- Pacora P, Romero R, Maymon E, Gervasi MT, Gomez R, Edwin SS, Yoon BH. Participation of the novel cytokine interleukin 18 in the host response to intra-amniotic infection. Am J Obstet Gynecol 2000;183:1138–1143.
- Athayde N, Romero R, Maymon E, Gomez R, Pacora P, Yoon BH, Edwin SS. Interleukin 16 in pregnancy, parturition, rupture of fetal membranes, and microbial invasion of the amniotic cavity. Am J Obstet Gynecol 2000;182:135–141.
- Cherouny PH, Pankuch GA, Romero R, Botti JJ, Kuhn DC, Demers LM, Appelbaum PC. Neutrophil attractant/activating peptide-1/interleukin-8: association with histologic chorioamnionitis, preterm delivery, and bioactive amniotic fluid leukoattractants. Am J Obstet Gynecol 1993;169:1299–1303.
- Romero R, Ceska M, Avila C, Mazor M, Behnke E, Lindley I. Neutrophil attractant/activating peptide-1/interleukin-8 in term and preterm parturition. Am J Obstet Gynecol 1991;165:813–820.
- Saito S, Kato Y, Ishihara Y, Ichijo M. Amniotic fluid granulocyte colony-stimulating factor in preterm and term labor. Clin Chim Acta 1992;208:105–109.
- Chaiworapongsa T, Romero R, Espinoza J, Kim YM, Edwin S, Bujold E, Gomez R, Kuivaniemi H. Macrophage migration inhibitory factor in patients with preterm parturition and microbial invasion of the amniotic cavity. J Matern Fetal Neonatal Med 2005;18:405–416.
- Esplin MS, Romero R, Chaiworapongsa T, Kim YM, Edwin S, Gomez R, Mazor M, Adashi EY. Monocyte chemotactic protein-1 is increased in the amniotic fluid of women who deliver preterm in the presence or absence of intra-amniotic infection. J Matern Fetal Neonatal Med 2005;17:365–373.
- Romero R, Gomez R, Galasso M, Munoz H, Acosta L, Yoon BH, Svinarich D, Cotton DB. Macrophage inflammatory protein-1 alpha in term and preterm parturition: effect of microbial invasion of the amniotic cavity. Am J Reprod Immunol 1994;32:108–113.
- Athayde N, Romero R, Maymon E, Gomez R, Pacora P, Araneda H, Yoon BH. A role for the novel cytokine RANTES in pregnancy and parturition. Am J Obstet Gynecol 1999;181:989–994.
- Keelan JA, Yang J, Romero RJ, Chaiworapongsa T, Marvin KW, Sato TA, Mitchell MD. Epithelial cell-derived neutrophil-activating peptide-78 is present in fetal membranes and amniotic fluid at increased concentrations with intra-amniotic infection and preterm delivery. Biol Reprod 2004;70:253–259.
- Mittal P, Romero R, Kusanovic JP, Edwin SS, Gotsch F, Mazaki-Tovi S, Espinoza J, Erez O, Nhan-Chang CL, Than NG, et al CXCL6 (granulocyte chemotactic protein-2): a novel chemokine involved in the innate immune response of the amniotic cavity. Am J Reprod Immunol 2008;60:246–257.
- Nhan-Chang CL, Romero R, Kusanovic JP, Gotsch F, Edwin SS, Erez O, Mittal P, Kim CJ, Kim MJ, Espinoza J, et al A role for CXCL13 (BCA-1) in pregnancy and intra-amniotic infection/inflammation. J Matern Fetal Neonatal Med 2008;21:763–775.
- Hamill N, Romero R, Gotsch F, Pedro KJ, Edwin S, Erez O, Than NG, Mittal P, Espinoza J, Friel LA, et al Exodus-1 (CCL20): evidence for the participation of this chemokine in spontaneous labor at term, preterm labor, and intrauterine infection. J Perinat Med 2008;36:217–227.
- Casey ML, Cox SM, Beutler B, Milewich L, MacDonald PC. Cachectin/tumor necrosis factor-alpha formation in human decidua. Potential role of cytokines in infection-induced preterm labor. J Clin Invest 1989;83:430–436.
- Romero R, Wu YK, Brody DT, Oyarzun E, Duff GW, Durum SK. Human decidua: a source of interleukin-1. Obstet Gynecol 1989;73:31–34.
- Molnar M, Romero R, Hertelendy F. Interleukin-1 and tumor-necrosis-factor stimulate arachidonic-acid release and phospholipid-metabolism in human myometrial cells. Am J Obstet Gynecol 1993;169:825–829.
- Romero R, Mazor M, Wu YK, Avila C, Oyarzun E, Mitchell MD. Bacterial endotoxin and tumor necrosis factor stimulate prostaglandin production by human decidua. Prostaglandins Leukot Essent Fatty Acids 1989;37:183–186.
- Romero R, Durum S, Dinarello CA, Oyarzun E, Hobbins JC, Mitchell MD. Interleukin-1 stimulates prostaglandin biosynthesis by human amnion. Prostaglandins 1989;37:13–22.
- Hertelendy F, Rastogi P, Molnar M, Romero R. Interleukin-1beta-induced prostaglandin E2 production in human myometrial cells: role of a pertussis toxin-sensitive component. Am J Reprod Immunol 2001;45:142–147.
- Hertelendy F, Molnar M, Romero R. Interferon gamma antagonizes interleukin-1beta-induced cyclooxygenase-2 expression and prostaglandin E(2) production in human myometrial cells. J Soc Gynecol Investig 2002;9:215–219.
- Romero R, Mazor M, Wu YK, Sirtori M, Oyarzun E, Mitchell MD, Hobbins JC. Infection in the pathogenesis of preterm labor. Semin Perinatol 1988;12:262–279.
- Athayde N, Edwin SS, Romero R, Gomez R, Maymon E, Pacora P, Menon R. A role for matrix metalloproteinase-9 in spontaneous rupture of the fetal membranes. Am J Obstet Gynecol 1998;179:1248–1253.
- Maymon E, Romero R, Pacora P, Gervasi MT, Gomez R, Edwin SS, Yoon BH. Evidence of in vivo differential bioavailability of the active forms of matrix metalloproteinases 9 and 2 in parturition, spontaneous rupture of membranes, and intra-amniotic infection. Am J Obstet Gynecol 2000;183:887–894.
- Romero R, Chaiworapongsa T, Espinoza J, Gomez R, Yoon BH, Edwin S, Mazor M, Maymon E, Berry S. Fetal plasma MMP-9 concentrations are elevated in preterm premature rupture of the membranes. Am J Obstet Gynecol 2002;187:1125–1130.
- Watari M, Watari H, DiSanto ME, Chacko S, Shi GP, Strauss JF, III. Pro-inflammatory cytokines induce expression of matrix-metabolizing enzymes in human cervical smooth muscle cells. Am J Pathol 1999;154:1755–1762.
- Romero R, Yoon BH, Mazor M, Gomez R, Diamond MP, Kenney JS, Ramirez M, Fidel PL, Sorokin Y, Cotton D, et al The diagnostic and prognostic value of amniotic fluid white blood cell count, glucose, interleukin-6, and gram stain in patients with preterm labor and intact membranes. Am J Obstet Gynecol 1993;169:805–816.
- Yoon BH, Romero R, Kim CJ, Jun JK, Gomez R, Choi JH, Syn HC. Amniotic fluid interleukin-6: a sensitive test for antenatal diagnosis of acute inflammatory lesions of preterm placenta and prediction of perinatal morbidity. Am J Obstet Gynecol 1995;172:960–970.
- Montague CT, O'Rahilly S. The perils of portliness: causes and consequences of visceral adiposity. Diabetes 2000;49:883–888.
- Friedman JM, Halaas JL. Leptin and the regulation of body weight in mammals. Nature 1998;395:763–770.
- Berg AH, Combs TP, Scherer PE. ACRP30/adiponectin: an adipokine regulating glucose and lipid metabolism. Trends Endocrinol Metab 2002;13:84–89.
- Hotamisligil GS, Shargill NS, Spiegelman BM. Adipose expression of tumor necrosis factor-alpha: direct role in obesity-linked insulin resistance. Science 1993;259:87–91.
- Vidal H. Gene expression in visceral and subcutaneous adipose tissues. Ann Med 2001;33:547–555.
- Hu E, Liang P, Spiegelman BM. AdipoQ is a novel adipose-specific gene dysregulated in obesity. J Biol Chem 1996;271:10697–10703.
- Maeda K, Okubo K, Shimomura I, Funahashi T, Matsuzawa Y, Matsubara K. cDNA cloning and expression of a novel adipose specific collagen-like factor apM1 (AdiPose Most abundant Gene transcript 1). Biochem Biophys Res Commun 1996;221:286–289.
- Nakano Y, Tobe T, Choi-Miura NH, Mazda T, Tomita M. Isolation and characterization of GBP28, a novel gelatin-binding protein purified from human plasma. J Biochem.(Tokyo) 1996;120:803–812.
- Scherer PE, Williams S, Fogliano M, Baldini G, Lodish HF. A novel serum protein similar to C1q, produced exclusively in adipocytes. J Biol Chem 1995;270:26746–26749.
- Berg AH, Combs TP, Du X, Brownlee M, Scherer PE. The adipocyte-secreted protein Acrp30 enhances hepatic insulin action. Nat Med 2001;7:947–953.
- Ouchi N, Kihara S, Arita Y, Nishida M, Matsuyama A, Okamoto Y, Ishigami M, Kuriyama H, Kishida K, Nishizawa H, et al Adipocyte-derived plasma protein, adiponectin, suppresses lipid accumulation and class A scavenger receptor expression in human monocyte-derived macrophages. Circulation 2001;103:1057–1063.
- Shibata R, Ouchi N, Kihara S, Sato K, Funahashi T, Walsh K. Adiponectin stimulates angiogenesis in response to tissue ischemia through stimulation of amp-activated protein kinase signaling. J Biol Chem 2004;279:28670–28674.
- Shimabukuro M, Higa N, Asahi T, Oshiro Y, Takasu N, Tagawa T, Ueda S, Shimomura I, Funahashi T, Matsuzawa Y. Hypoadiponectinemia is closely linked to endothelial dysfunction in man. J Clin Endocrinol Metab 2003;88:3236–3240.
- Baviera G, Corrado F, Dugo C, Cannata ML, Russo S, Rosario D. Midtrimester amniotic fluid adiponectin in normal pregnancy. Clin Chem 2007;53:1723–1724.
- Alexander GR, Himes JH, Kaufman RB, Mor J, Kogan M. A United States national reference for fetal growth. Obstet Gynecol 1996;87:163–168.
- Gonzalez RP, Gomez RM, Castro RS, Nien JK, Merino PO, Etchegaray AB, Carstens MR, Medina LH, Viviani PG, Rojas IT. [A national birth weight distribution curve according to gestational age in Chile from 1993 to 2000]. Rev Med Chil 2004;132:1155–1165.
- Yoon BH, Romero R, Moon JB, Shim SS, Kim M, Kim G, Jun JK. Clinical significance of intra-amniotic inflammation in patients with preterm labor and intact membranes. Am J Obstet Gynecol 2001;185:1130–1136.
- Romero R, Emamian M, Quintero R, Wan M, Hobbins JC, Mazor M, Edberg S. The value and limitations of the Gram stain examination in the diagnosis of intraamniotic infection. Am J Obstet Gynecol 1988;159:114–119.
- Romero R, Jimenez C, Lohda AK, Nores J, Hanaoka S, Avila C, Callahan R, Mazor M, Hobbins JC, Diamond MP. Amniotic fluid glucose concentration: a rapid and simple method for the detection of intraamniotic infection in preterm labor. Am J Obstet Gynecol 1990;163:968–974.
- Romero R, Quintero R, Nores J, Avila C, Mazor M, Hanaoka S, Hagay Z, Merchant L, Hobbins JC. Amniotic fluid white blood cell count: a rapid and simple test to diagnose microbial invasion of the amniotic cavity and predict preterm delivery. Am J Obstet Gynecol 1991;165:821–830.
- Wolf AM, Wolf D, Rumpold H, Enrich B, Tilg H. Adiponectin induces the anti-inflammatory cytokines IL-10 and IL-1RA in human leukocytes. Biochem Biophys Res Commun 2004;323:630–635.
- Wulster-Radcliffe MC, Ajuwon KM, Wang J, Christian JA, Spurlock ME. Adiponectin differentially regulates cytokines in porcine macrophages. Biochem Biophys Res Commun 2004;316:924–929.
- Yokota T, Oritani K, Takahashi I, Ishikawa J, Matsuyama A, Ouchi N, Kihara S, Funahashi T, Tenner AJ, Tomiyama Y, et al Adiponectin, a new member of the family of soluble defense collagens, negatively regulates the growth of myelomonocytic progenitors and the functions of macrophages. Blood 2000;96:1723–1732.
- Ouchi N, Kihara S, Arita Y, Okamoto Y, Maeda K, Kuriyama H, Hotta K, Nishida M, Takahashi M, Muraguchi M, et al Adiponectin, an adipocyte-derived plasma protein, inhibits endothelial NF-kappaB signaling through a cAMP-dependent pathway. Circulation 2000;102:1296–1301.
- Arita Y, Kihara S, Ouchi N, Takahashi M, Maeda K, Miyagawa J, Hotta K, Shimomura I, Nakamura T, Miyaoka K, et al Paradoxical decrease of an adipose-specific protein, adiponectin, in obesity. Biochem Biophys Res Commun 1999;257:79–83.
- Nien JK, Mazaki-Tovi S, Romero R, Erez O, Kusanovic JP, Gotsch F, Pineles BL, Gomez R, Edwin S, Mazor M, et al Plasma adiponectin concentrations in non-pregnant, normal and overweight pregnant women. J Perinat Med 2007;35:522–531.
- Yamauchi T, Kamon J, Waki H, Terauchi Y, Kubota N, Hara K, Mori Y, Ide T, Murakami K, Tsuboyama-Kasaoka N, et al The fat-derived hormone adiponectin reverses insulin resistance associated with both lipoatrophy and obesity. Nat Med 2001;7:941–946.
- Rovin BH, Song H, Hebert LA, Nadasdy T, Nadasdy G, Birmingham DJ, Yung YC, Nagaraja HN. Plasma, urine, and renal expression of adiponectin in human systemic lupus erythematosus. Kidney Int 2005;68:1825–1833.
- Catalano PM, Hoegh M, Minium J, Huston-Presley L, Bernard S, Kalhan S, Hauguel-De MS. Adiponectin in human pregnancy: implications for regulation of glucose and lipid metabolism. Diabetologia 2006;49:1677–1685.
- Mazaki-Tovi S, Kanety H, Pariente C, Hemi R, Wiser A, Schiff E, Sivan E. Maternal serum adiponectin levels during human pregnancy. J Perinatol 2007;27:77–81.
- McLachlan KA, O'Neal D, Jenkins A, Alford FP. Do adiponectin, TNFalpha, leptin and CRP relate to insulin resistance in pregnancy? Studies in women with and without gestational diabetes during and after pregnancy. Diabetes Metab Res Rev 2006;22:131–138.
- Ranheim T, Haugen F, Staff AC, Braekke K, Harsem NK, Drevon CA. Adiponectin is reduced in gestational diabetes mellitus in normal weight women. Acta Obstet Gynecol Scand 2004;83:341–347.
- Worda C, Leipold H, Gruber C, Kautzky-Willer A, Knofler M, Bancher-Todesca D. Decreased plasma adiponectin concentrations in women with gestational diabetes mellitus. Am J Obstet Gynecol 2004;191:2120–2124.
- D'Anna R, Baviera G, Corrado F, Giordano D, De VA, Nicocia G, Di BA. Adiponectin and insulin resistance in early- and late-onset pre-eclampsia. BJOG 2006;113:1264–1269.
- Haugen F, Ranheim T, Harsem NK, Lips E, Staff AC, Drevon CA. Increased plasma levels of adipokines in preeclampsia: relationship to placenta and adipose tissue gene expression. Am J Physiol Endocrinol Metab 2006;290:E326–E333.
- Kajantie E, Kaaja R, Ylikorkala O, Andersson S, Laivuori H. Adiponectin concentrations in maternal serum: elevated in preeclampsia but unrelated to insulin sensitivity. J Soc Gynecol Investig 2005;12:433–439.
- Mazaki-Tovi S, Romero R, Vaisbuch E, Kusanovic JP, Erez O, Gotsch F, Chaiworapongsa T, Than NG, Kim SK, Nhan-Chang CL, et al Maternal serum adiponectin multimers in preeclampsia. J Perinat Med 2009;37:349–363.
- Naruse K, Yamasaki M, Umekage H, Sado T, Sakamoto Y, Morikawa H. Peripheral blood concentrations of adiponectin, an adipocyte-specific plasma protein, in normal pregnancy and preeclampsia. J Reprod Immunol 2005;65:65–75.
- Ramsay JE, Jamieson N, Greer IA, Sattar N. Paradoxical elevation in adiponectin concentrations in women with preeclampsia. Hypertension 2003;42:891–894.
- Mazaki-Tovi S, Kanety H, Sivan E. Adiponectin and human pregnancy. Curr Diab Rep 2005;5:278–281.
- Mazaki-Tovi S, Kanety H, Pariente C, Hemi R, Efraty Y, Schiff E, Shoham A, Sivan E. Determining the source of fetal adiponectin. J Reprod Med 2007;52:774–778.
- Mazaki-Tovi S, Romero R, Kusanovic JP, Erez O, Vaisbuch E, Gotsch F, Mittal P, Than GN, Nhan-Chang C, Chaiworapongsa T, et al Adiponectin multimers in maternal plasma. J Matern Fetal Neonatal Med 2008;21:796–815.
- Nien JK, Mazaki-Tovi S, Romero R, Erez O, Kusanovic JP, Gotsch F, Pineles BL, Gomez R, Edwin S, Mazor M, et al Plasma adiponectin concentrations in non-pregnant, normal and overweight pregnant women. J Perinat Med 2007;35:522–531.
- Sivan E, Mazaki-Tovi S, Pariente C, Efraty Y, Schiff E, Hemi R, Kanety H. Adiponectin in human cord blood: relation to fetal birth weight and gender. J Clin Endocrinol Metab 2003;88:5656–5660.
- Lopez-Bermejo A, Fernandez-Real JM, Garrido E, Rovira R, Brichs R, Genaro P, Bach C, Cabrero D, Kihara S, Funahashi T, et al Maternal soluble tumour necrosis factor receptor type 2 (sTNFR2) and adiponectin are both related to blood pressure during gestation and infant's birthweight. Clin Endocrinol.(Oxf) 2004;61:544–552.
- Retnakaran R, Hanley AJ, Raif N, Connelly PW, Sermer M, Zinman B. Reduced adiponectin concentration in women with gestational diabetes: a potential factor in progression to type 2 diabetes. Diabetes Care 2004;27:799–800.
- Ranheim T, Haugen F, Staff AC, Braekke K, Harsem NK, Drevon CA. Adiponectin is reduced in gestational diabetes mellitus in normal weight women. Acta Obstet Gynecol Scand 2004;83:341–347.
- Thyfault JP, Hedberg EM, Anchan RM, Thorne OP, Isler CM, Newton ER, Dohm GL, deVente JE. Gestational diabetes is associated with depressed adiponectin levels. J Soc Gynecol Investig 2005;12:41–45.
- Worda C, Leipold H, Gruber C, Kautzky-Willer A, Knofler M, Bancher-Todesca D. Decreased plasma adiponectin concentrations in women with gestational diabetes mellitus. Am J Obstet Gynecol 2004;191:2120–2124.
- Nien JK, Mazaki-Tovi S, Romero R, Erez O, Kusanovic JP, Gotsch F, Pineles BL, Gomez R, Edwin S, Mazor M, et al Plasma adiponectin concentrations in non-pregnant, normal and overweight pregnant women. J Perinat Med 2007;35:522–531.
- Hendler I, Blackwell SC, Mehta SH, Whitty JE, Russell E, Sorokin Y, Cotton DB. The levels of leptin, adiponectin, and resistin in normal weight, overweight, and obese pregnant women with and without preeclampsia. Am J Obstet Gynecol 2005;193:979–983.
- Haugen F, Ranheim T, Harsem NK, Lips E, Staff AC, Drevon CA. Increased plasma levels of adipokines in preeclampsia: relationship to placenta and adipose tissue gene expression. Am J Physiol Endocrinol Metab 2006;290:E326–E333.
- Kajantie E, Kaaja R, Ylikorkala O, Andersson S, Laivuori H. Adiponectin concentrations in maternal serum: elevated in preeclampsia but unrelated to insulin sensitivity. J Soc Gynecol Investig 2005;12:433–439.
- Naruse K, Yamasaki M, Umekage H, Sado T, Sakamoto Y, Morikawa H. Peripheral blood concentrations of adiponectin, an adipocyte-specific plasma protein, in normal pregnancy and preeclampsia. J Reprod Immunol 2005;65:65–75.
- Nien JK, Mazaki-Tovi S, Romero R, Erez O, Kusanovic JP, Gotsch F, Pineles BL, Gomez R, Edwin S, Mazor M, et al Adiponectin in severe preeclampsia. J Perinat Med 2007;35:503–512.
- Ramsay JE, Jamieson N, Greer IA, Sattar N. Paradoxical elevation in adiponectin concentrations in women with preeclampsia. Hypertension 2003;42:891–894.
- Galle PC, Meis PJ. Complications of amniocentesis: a review. J Reprod Med 1982;27:149–155.
- Schaffler A, Ehling A, Neumann E, Herfarth H, Tarner I, Scholmerich J, Muller-Ladner U, Gay S. Adipocytokines in synovial fluid. JAMA 2003;290:1709–1710.
- Kos K, Harte AL, da Silva NF, Tonchev A, Chaldakov G, James S, Snead DR, Hoggart B, O'Hare JP, McTernan PG, et al Adiponectin and resistin in human cerebrospinal fluid and expression of adiponectin receptors in the human hypothalamus. J Clin Endocrinol Metab 2007;92:1129–1136.
- Neumeier M, Weigert J, Buettner R, Wanninger J, Schaffler A, Muller AM, Killian S, Sauerbruch S, Schlachetzki F, Steinbrecher A, et al Detection of adiponectin in cerebrospinal fluid in humans. Am J Physiol Endocrinol Metab 2007;293:E965–E969.
- Takemura Y, Osuga Y, Harada M, Hirata T, Koga K, Yoshino O, Hirota Y, Morimoto C, Yano T, Taketani Y. Concentration of adiponectin in peritoneal fluid is decreased in women with endometriosis. Am J Reprod Immunol 2005;54:217–221.
- Toda M, Tsukinoki R, Morimoto K. Measurement of salivary adiponectin levels. Acta Diabetol 2007;44:20–22.
- Koshimura J, Fujita H, Narita T, Shimotomai T, Hosoba M, Yoshioka N, Kakei M, Fujishima H, Ito S. Urinary adiponectin excretion is increased in patients with overt diabetic nephropathy. Biochem Biophys Res Commun 2004;316:165–169.
- Mazaki-Tovi S, Kanety H, Pariente C, Hemi R, Schiff E, Sivan E. Cord blood adiponectin in large-for-gestational age newborns. Am J Obstet Gynecol 2005;193:1238–1242.
- Mazaki-Tovi S, Kanety H, Pariente C, Hemi R, Yinon Y, Wiser A, Schiff E, Sivan E. Adiponectin and leptin concentrations in dichorionic twins with discordant and concordant growth. J Clin Endocrinol Metab 2009;94:892–898.
- Shen YY, Hughes JT, Charlesworth JA, Kelly JJ, Peake PW. Adiponectin is present in the urine in its native conformation and specifically reduces the secretion of MCP-1 by proximal tubular cells. Nephrology.(Carlton.) 2008;13:405–410.
- Kajantie E, Hytinantti T, Hovi P, Andersson S. Cord plasma adiponectin: a 20-fold rise between 24 weeks gestation and term. J Clin Endocrinol Metab 2004;89:4031–4036.
- Siahanidou T, Mandyla H, Papassotiriou GP, Papassotiriou I, Chrousos G. Circulating levels of adiponectin in preterm infants. Arch Dis Child Fetal Neonatal Ed 2007;92:F286–F290.
- Romero R, Gotsch F, Pineles B, Kusanovic JP. Inflammation in pregnancy: its roles in reproductive physiology obstetrical complications and fetal injury. Nutr Rev 2007;65:S194–S202.
- Yoon BH, Kim YA, Romero R, Kim JC, Park KH, Kim MH, Park JS. Association of oligohydramnios in women with preterm premature rupture of membranes with an inflammatory response in fetal, amniotic, and maternal compartments. Am J Obstet Gynecol 1999;181:784–788.
- Lappas M, Yee K, Permezel M, Rice GE. Release and regulation of leptin, resistin and adiponectin from human placenta, fetal membranes, and maternal adipose tissue and skeletal muscle from normal and gestational diabetes mellitus-complicated pregnancies. J Endocrinol 2005;186:457–465.
- Han YM, Romero R, Kim JS, Tarca AL, Kim SK, Draghici S, Kusanovic JP, Gotsch F, Mittal P, Hassan SS, et al Region-specific gene expression profiling: novel evidence for biological heterogeneity of the human amnion. Biol Reprod 2008;79:954–961.
- Haddad R, Tromp G, Kuivaniemi H, Chaiworapongsa T, Kim YM, Romero R. Spontaneous labor at term is characterized by a genomic signature of acute inflammation in the chorioamniotic membranes but not in the systemic circulation. Am J Obstet Gynecol 2004;191:S138.
- Kusanovic JP, Romero R. Mazaki-Tovi S, Chaiworapongsa T, Mittal P, Gotsch F, Erez O, Vaisbuch E, Edwin S, Than NG, et al Resistin in amniotic fluid and its association with intra-amniotic infection and inflammation. J Matern Fetal Neonatal Med 2008;21:902–916.
- Mazaki-Tovi S, Romero R, Kusanovic JP, Erez O, Gotsch F, Mittal P, Than NG, Nhan-Chang CL, Hamill N, Vaisbuch E, et al Visfatin/Pre-B cell colony-enhancing factor in amniotic fluid in normal pregnancy, spontaneous labor at term, preterm labor and prelabor rupture of membranes: an association with subclinical intrauterine infection in preterm parturition. J Perinat Med 2008;36:485–496.
- Vaisbuch E, Mazaki-Tovi S, Kusanovic JP, Erez O, Than GN, Kim SK, Dong M, Gotsch F, Mittal P, Chaiworapongsa T, et al Retinol Binding Protein 4: an adipokine associated with intra-amniotic infection/inflammation. J Matern Fetal Neonatal Med 2009; In Press.