Abstract
Background and purpose — Minimizing the decrease in muscular strength after total hip arthroplasty (THA) might allow patients to recover faster. We evaluated muscular strength in patients who were operated on using 3 surgical approaches.
Patients and methods — In a prospective cohort study, 60 patients scheduled for primary THA were allocated to the direct lateral, posterior, or anterior approach. Leg press and abduction strength were evaluated 2 weeks or less preoperatively, 2 and 8 days postoperatively, and at 6-week and 3-month follow-up.
Results — Differences in maximal strength change were greatest after 2 and 8 days. The posterior and anterior approaches produced less decrease in muscular strength than the direct lateral approach. 6 weeks postoperatively, the posterior approach produced greater increase in muscular strength than the direct lateral approach, and resulted in a greater increase in abduction strength than the anterior approach. At 3-month follow-up, no statistically significant differences between the groups were found. The operated legs were 18% weaker in leg press and 15% weaker in abduction than the unoperated legs, and the results were similar between groups.
Interpretation — The posterior and anterior approaches appeared to have the least negative effect on abduction and leg press muscular strength in the first postoperative week; the posterior approach had the least negative effect, even up to 6 weeks postoperatively. THA patients have reduced muscle strength in the operated leg (compared to the unoperated leg) 3 months after surgery.
Regaining muscular strength is important for postoperative function after hip arthroplasty. Inactivity reduces muscular strength and physical function (CitationMcGuire et al. 2001, CitationSuesada et al. 2007, CitationKortebein et al. 2008), and muscular strength decreases substantially in the first week after total hip arthroplasty (THA) (CitationHolm et al. 2013). Early recovery and rehabilitation of the weakened musculature is therefore of importance (CitationSicard-Rosenbaum et al. 2002). The type of surgical approach used has a major impact on THA stability and muscle function (CitationMasonis and Bourne 2002).
The direct lateral approach (DLA) is associated with a low dislocation risk (CitationWitzleb et al. 2009), but of concern is that it traumatizes the abductor muscles, which can lead to permanent postoperative limp and weakness (CitationEdmunds and Boscainos 2011). The posterior approach (PA) has been associated with postoperative dislocations (CitationEdmunds and Boscainos 2011, CitationBrooks 2013), mainly owing to the small femoral heads used to prevent wear (CitationBystrom et al. 2003). However, the introduction of highly cross-linked polyethylene into the articulation has reduced wear independently of head diameter (CitationBragdon et al. 2007), leading to increased use of larger head diameters (CitationLombardi et al. 2011). It has also been shown that a posterior soft-tissue repair following PA reduces the dislocation rate (Citationvan Stralen et al. 2003, CitationSuh et al. 2004). The anterior approach (AA), first described by Robert Judet in 1947 as a modified Smith-Petersen approach, follows the principles of minimally invasive surgery. This approach provides intermuscular and internervous exposure to the hip (CitationWojciechowski et al. 2007), leading to reduced soft-tissue dissection and trauma (CitationBergin et al. 2011). Concerns have been related to higher complication rates owing to wound complications, intraoperative fracture, and compromised fixation after minimally invasive surgery, with increased risks of early revision surgery (CitationGraw et al. 2010).
There is no consensus on the relative functional advantages of different surgical approaches (CitationGulati et al. 2008, CitationEdmunds and Boscainos 2011), and differences in maximal strength have not been examined. To our knowledge, there have been no studies comparing the DLA, the PA, and the AA in terms of early maximal muscular strength. We compared these 3 surgical approaches with regard to regaining of maximal muscular strength by 3 months postoperatively in patients undergoing THA.
Patients and methods
Patients
Patients less than 70 years old with a BMI of less than 34 who had a diagnosis of unilateral ost eoarthritis and who were scheduled for primary THA were assessed for eligibility. Exclusion criteria were any other disease or illness entailing difficulty with testing. Patients were included between June 2011 and June 2013.
Study design
This was a prospective cohort study with 3 parallel groups. 60 consecutive patients were scheduled for 1of 3 surgical approaches: the direct lateral approach (DLA), the posterior approach (PA), or the anterior approach (AA). Patients were allocated to the groups by the order in which they were included in the study; the first 20 patients were allocated to the DLA group, the next 20 patients to the PA group, and the last 20 patients to the AA group. 1 patient was re-scheduled from PA surgery to DLA surgery because of acute illness on the day of surgery. As surgery was postponed, the surgeon with expertise in PA surgery was not available. Thus, the DLA group had 21 patients and the PA group had 19 patients (Figure 1, see Supplementary data). A team of 3 experienced surgeons was in charge of the surgeries, each with expertise in one of the approaches. Therefore, none of the surgeons had a learning curve. The patients followed the standardized fast-track clinical pathway at Trondheim University Hospital (CitationWinther et al. 2015), including mobilization in the recovery unit as soon as the block from the spinal anesthesia had disappeared. After discharge, the patients were tested at 2 days, 8 days, 6 weeks, and 3 months postoperatively.
Implants
All operations used an uncemented, double-tapered, fully hydroxyapatite-coated stem (Profemur Gladiator, Wright Medical Technology Inc., Memphis, TN, USA). All implants had a modular neck and a ceramic head with a 28-mm or 32-mm articulation. All the patients in the DLA group received a head with a 28-mm articulation. The third patient in the PA group had a hip dislocation, and the remaining patients were given heads with a 32-mm articulation. All the patients in the AA group received 32-mm articulations. The acetabular component was an uncemented, porous cup with a highly cross-linked polyethylene insert (Reflection; Smith and Nephew, London, UK).
Surgical procedures
The direct lateral approach (DLA): Following a posterior curved lateral incision, the hip was exposed through a direct lateral approach, as described by Frndak and modified by CitationHardinge (1982). The deep fascia was split proximally in the direction of the anterior fibers of the gluteus maximus, and the common muscle plate of the anterior third of the vastus lateralis and the gluteus medius was dissected subperiosteally from the greater trochanter. During reconstruction of the abductor muscles, the common muscle plate was reinserted into the greater trochanter using 2 non-resorbable osteosutures. This fixation was reinforced with a continuously sewn, slowly resorbable, looped monofilament suture.
The posterior approach (PA): This approach was first described by Kocher and Langenbeck, and later modified by CitationGibson (1950). Following a curved skin incision with the top point slightly posterior to the greater trochanter, the incision in the fascia lata was begun in the distal wound. Proximally, the deep fascia was incised in the direction of the anterior fibers of the gluteus maximus. The external rotators (piriformis muscle and gemelli muscles) were divided close to the greater trochanter. From their insertion on the greater trochanter (marked with a suture), they were folded posteriorly, to protect the sciatic nerve. The capsule was incised in the same direction. For closure, the capsule was sutured and the external rotators were reinserted with a non-resorbable osteosuture.
The anterior approach (AA): The approach used was the modified Smith-Peterson approach as described by CitationBerend et al. (2009). This approach uses the internervous plane between the tensor fascia lata and the sartorius muscles, and moves laterally to the rectus femoris for deep dissection. For closure, a continuously resorbable suture was used in the fascia.
Outcome measures
Strength tests: 2 experienced physiologists and 2 physiotherapists administered the physical performance tests. 2 weeks preoperatively, all patients performed strength tests, expressed as 1 repetition maximum (1RM) in a standardized order. In all strength tests, the initial weight load was decided individually based on the examiner’s subjective estimation of the patient’s physical fitness. The 1RM strength test is a valid test to assess muscular strength in the lower extremities (CitationVerdijk et al. 2009).
1RM leg press: This was tested in a leg-press ergometer with the patient in supine position, using both legs simultaneously (Steens Physical; Ring Mekanikk AS, Moelv, Norway) (Figure 2, see Supplementary data). Each leg was tested individually: first the operated leg and then the non-operated leg. The test was approved when the patient was able to perform the leg-press movement from an extended position to flexion with a knee joint angle of 90° and a hip joint angle of 90°, and stretch into the extended position again. The weight was increased by 10 kg at each repetition, and the test was terminated when the patient could no longer manage to perform the leg-press movement.
1RM abduction strength: This was tested with the patient in supine position. An examination bench was customized to fix the patient in a stable position. An adjustable clamp arch against the iliac crest stabilized the pelvis (Figure 3, see Supplementary data). Both the operated leg and the non-operated leg were tested, with the leg not currently being tested inactivated in a vertical sling. Another sling was placed simultaneously on the leg being tested with its lower edge at the caput fibulae, and mounted on a pulling apparatus. Patients were instructed to place their arms on their chest, to extend the tested leg with toes pointing upwards, and to move the leg in horizontal abduction. The weight load was increased by 2.5 kg at each repetition, and the test was terminated when the patient could no longer perform the abduction movement.
Pain and disease-specific scores: Pain was assessed using a numeric rating scale (NRS) for pain, both during mobilization and at rest (CitationBreivik et al. 2008). The scores on the NRS were obtained preoperatively, and at 2 days, 8 days, 6 weeks, and 3 months postoperatively. The patients were asked a standardized question at rest before the maximal strength test, and during mobilization as the test was being performed: “On a scale from 0 to 10, where 0 is no pain and 10 is the worst pain imaginable, can you define the pain you have right now?”.
Statistics
Statistical calculations were performed using IBM SPSS Statistics version 21 and IBM SPSS SamplePower 3. A leg press strength difference of 20 kg or more was previously regarded as clinically relevant (CitationHusby et al. 2009), and this was used as a reference when calculating the number of patients needed. In all, 20 patients were to be included in each group, selecting a significance level of 5% and a power level of 80%. Analysis of variance (ANOVA) and Fisher’s exact test were used to compare the patients’ baseline data. Kolmogorov-Smirnov tests were used to determine whether data were normally distributed. Mixed linear models were used to analyze muscular strength data. Preoperative strength measurements were logarithmically transformed and included as covariates. The strength results were calculated as percentage changes from preoperative values and logarithmically transformed. Logarithmic data transformation was necessary to fulfill the assumption of normally distributed residuals in the linear models.
Bonferroni corrections were used to account for multiple comparisons between groups at the different follow-ups. The level of statistical significance was set at p < 0.05. The underlying test assumptions for all tests were fulfilled. The statistician was blinded to the group allocation.
Ethics
The study was approved by the regional ethics committee (entry no. 2011/450) and conducted in accordance with the Declaration of Helsinki. Each subject gave informed consent before participation in the study. The regional ethics committee had approved the consent form. The study was registered at ClinicalTrials.gov (identifier NCT01506024).
Results
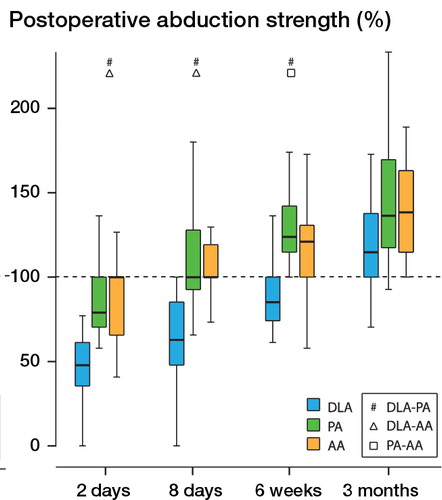
Of the 60 patients included in the study, 2 were excluded owing to complications, and 3 patients were lost to follow-up (Figure 1, see Supplementary data). There were no statistically significant differences in the patient baseline data, except for the leg-press test, where patients in the PA group were significantly stronger (). There were no statistically significant postoperative differences in pain scores between the groups at any of the follow-up assessments (p = 0.9) ().
Table 1. Preoperative characteristics of patients in the direct lateral approach (DLA), posterior approach (PA), and anterior approach (AA) groups. Values are mean (SD) or mean (range)
Figure 4. Pain scores (numeric rating scale) in the direct lateral approach (DLA) group, the posterior approach (PA) group, and the anterior approach (AA) group pre- and postoperatively. The circles are outliers. These are defined as values that do not fall within the inner fences. The asterisks are extreme outliers. These represent cases or rows that have values more than 3 times the height of the boxes.
1RM leg press
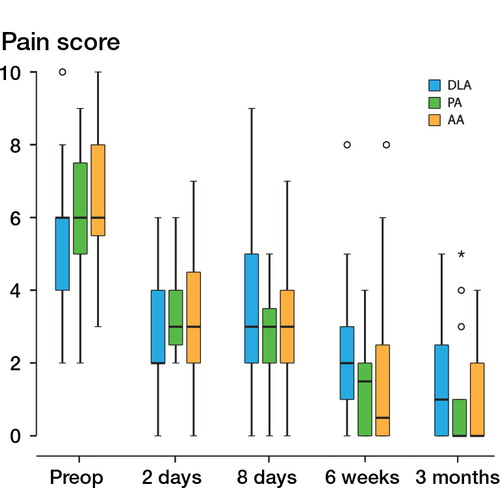
At 2 and 8 days postoperatively, patients in the DLA group had a statistically significantly larger reduction in muscular strength relative to the preoperative level than did the patients in the PA and AA groups, with no statistically significant difference between the PA and AA groups at 2 and 8 days postoperatively (). At 6 weeks postoperatively, there was still a statistically significant difference in percentage muscle strength change compared to preoperative values between the DLA group and the PA group, in favor of patients in the PA group. No statistically significant differences were found between patients in the AA group and patients in the PA group at 6 weeks, or between patients in the DLA and AA groups at 6 weeks. At 3-month follow-up, no statistically significant changes in muscle strength were found between any of the groups (). 3 months postoperatively, the leg-press muscular strength was 18% less in the operated leg than in the unoperated leg (p < 0.001), with no differences between the groups.
Table 2. Results from the leg-press test. Leg press (% compared with preoperative value)
Figure 5. Postoperative leg-press strength compared with preoperative values (100%) in the direct lateral approach (DLA) group, the posterior approach (PA) group, and the anterior approach (AA) group. #, Δ , and □ show statistically significant differences in percent change relative to preoperative values between groups.
1RM abduction
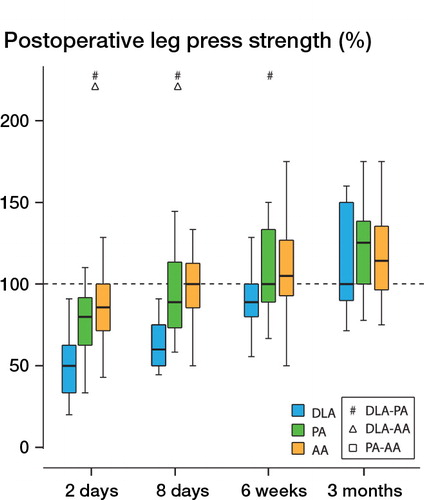
At 2 and 8 days postoperatively, patients in the DLA group had a statistically significantly larger reduction in muscular strength relative to the preoperative level than did the patients in the PA and AA groups, with no significant difference between the latter 2 groups (). 6 weeks postoperatively, there were statistically significant differences in percentage muscle strength change compared to preoperative values between patients in the DLA and PA groups and between patients in the PA and AA groups, in favor of patients in the PA group. No statistically significant differences in muscle strength changes were found between the AA group and the DLA group at 6 weeks. At 3-month follow-up, there were no statistically significant muscle strength changes between any of the groups (). At 3 months postoperatively, the abduction muscular strength was 15% less in the operated leg than in the unoperated leg (p < 0.001), with no statistically significant differences between groups.
Table 3. Results from the abduction test. Abduction (% compared with preoperative value)
Loss to follow-up, exclusions, and adverse events
3 patients were lost to follow-up, for personal reasons: 2 in the DLA group before the 3-month test and one in the PA group before the 6-week test (Figure 1, see Supplementary data). 2 patients were excluded, 1 in the PA group, owing to posterior dislocation before the 3-month test, and 1 in the AA group, in whom the liner had dislocated perioperatively. 2 patients experienced adverse events that did not compromise participation in the study: 1 in the PA group had an accidental dural puncture and 1 in the AA group had a cardiac arrest during surgery, but was successfully resuscitated with no sequelae.
Discussion
It is reasonable to assume that the differences in muscular strength between the groups were caused by differences in the surgical approaches. In the PA, the gluteus maximus, piriformis muscle, and gemelli muscles are the muscles affected. In the DLA, the vastus lateralis, gluteus maximus, and gluteus medius are affected. In the AA, the muscles are mainly spared, but the tensor fascia latae and the rectus femoris, sartorius, and gluteus medius are extensively stretched, owing to the small incision in the skin.
The leg-press exercise is performed using the quadriceps, hamstrings, and gluteal muscles. In the DLA, the vastus lateralis muscle is traumatized, owing to the continuation of the incision of the anterior part of the gluteus medius into the anterior part of the vastus lateralis. Leg-press strength is therefore reduced, which may explain the inferior leg-press strength in the patients in the DLA group. Furthermore, the incision in the gluteus maximus in the PA is positioned slightly posteriorly to that in the DLA, which might have fewer implications for leg-press muscular strength.
The abduction exercise mainly involves the gluteus medius and the gluteus minimus. The piriformis muscle, the tensor fascia latae, and the upper fibers of the gluteus maximus also contribute, but to a lesser degree. The inferior results in the abduction exercise in the DLA group are therefore not unexpected. By performing the surgery intermuscularly, with no detachment or dissection of muscles and tendons, the abductors are thought to be completely spared in the AA. The AA has previously been found to reduce pain and result in a better clinical outcome (CitationWojciechowski et al. 2007). The benefit of sparing of the abductors can, however, be insignificant if the AA leads to muscle damage to the tensor fascia latae and rectus femoris, as described in a cadaveric study by CitationMeneghini et al. (2006). This might have been the case in our study, as patients in the PA group did not show less reduction in muscle strength than did patients in the AA group within the first postoperative week. The results indicate that the traumatization of the gluteus maximus in the PA group during surgery had a minor effect on leg-press and abduction muscular strength. The gluteus medius muscle is not affected by the PA (CitationBaker and Bitounis 1989), which might explain the superior outcome for abduction strength in the patients in the PA group.
As expected, all patient groups improved in muscular strength in maximal leg press and abduction with longer follow-up time, from 2 days up to 3 months postoperatively. However, the amount of improvement differed. Patients in the PA and AA groups had less reduction in muscular strength than the DLA group from preoperatively until 2 and 8 days postoperatively following THA surgery. At 6 weeks, the PA group still had less reduction in muscle strength than the DLA group in both leg press and abduction, and less reduction in muscle strength than the AA group in abduction strength only. At 3-month follow-up, muscular strength was similar between the groups. This is in line with the findings of CitationDowning et al. (2001), who reported no difference in abductor strength between their DLA and PA groups 3 and 12 months postoperatively. The abductor muscles are important for a normal gait pattern without limping (CitationJohnston et al. 2007). Thus, our findings are important for the everyday function of the patients, particularly in the early postoperative phase. Another relevant clinical finding of our study is that even though muscular strength was increased above preoperative levels at 3 months, the patients did not have equal muscular strength levels in the operated and unoperated legs, either in the leg press test or in the abduction test. Muscular strength was similar between the groups, indicating that irrespective of the approach used, the traumatization of muscles during surgery results in clinically relevant reduction in muscle strength, even 3 months after surgery. Regaining of equal bilateral muscle strength postoperatively is important in achieving a normal gait pattern without limping (CitationSuter et al. 1998, CitationJohnston et al. 2007, CitationTalis et al. 2008, CitationTsai et al. 2015). Overloading of the unoperated hip might also increase the risk of developing osteoarthritis in the healthy leg (CitationSuter et al. 1998, CitationTalis et al. 2008).
There have been studies demonstrating that the surgical approach has an effect on pain, health-related quality of life, and hip function after THA (CitationEdmunds and Boscainos 2011, CitationSmith et al. 2011, CitationLindgren et al. 2012), even up to 6 years postoperatively (CitationLindgren et al. 2012). In the present study, we did not find any significant difference in pain scores between the groups. Accordingly, the results from muscular strength measurements did not appear to be influenced by pain.
The strength of our study is that highly skilled surgeons performed all the surgical procedures, thereby minimizing the effect of possible learning curves. Another strength is that the standardized fast-track patient course minimized the risk of possible confounding factors, such as different pain management, rehabilitation, or patient education (CitationPoehling-Monaghan et al. 2015). The age limit (< 70 years) was set to make it possible to use the same type of uncemented component in all patients. The age of the study population in is in accordance with the majority of THA patients who were operated on in Norway in 2013 (The Norwegian Arthroplasty Register, Report June 2014). The restriction on body mass index in this study is consistent with that in other studies (CitationRestrepo et al. 2010, CitationChristensen et al. 2014).
The main limitation of the present study is its non-randomized design. A statistically significant difference in leg-press test results between the groups was present preoperatively and may have been caused by an imbalance seen in the distribution between sexes. However, as the groups were analyzed as ratios based on changes in muscular strength and with preoperative strength included as a covariate, the results should not have been affected by these differences. The patients had different scars and, because of the study design, the examiners were aware of the approach that had been used for each patient.
In conclusion, our findings have shown that patients operated on using the PA and the AA had less reduction in muscular strength following THA surgery than did the patients in the DLA group in the first postoperative week. Although the group differences were most prominent in the first postoperative week, the PA appears to be the surgical approach that has the least negative impact on muscular strength up to 6 weeks postoperatively. Patients operated on using THA had less muscle strength in the operated leg than in the unoperated leg at the 3-month follow-up. Surgical approaches affect postoperative muscular strength differently and could influence early postoperative mobilization and recovery.
Supplementary data
Figures 1–3 are available on the Acta Orthopaedica website, www.actaorthop.org, identification number 8623.
IORT_A_1068032_SM4812.pdf
Download PDF (240.6 KB)All the authors contributed to the study design and contributed substantially to interpreting the results, to drafting the article, and to revising it for important intellectual content. SBW, ME, and VSH performed all data collection. OAF conducted the statistical analysis. OSH and TSW recruited the patients.
No competing interests declared.
- Baker AS, Bitounis VC. Abductor function after total hip replacement. An electromyographic and clinical review. J Bone Joint Surg Br 1989; 71 (1): 47–50.
- Berend KR, Lombardi AVJr, Seng BE, Adams JB, Enhanced early outcomes with the anterior supine intermuscular approach in primary total hip arthroplasty. J Bone Joint Surg Am 2009; 91 Suppl 6: 107–20.
- Bergin PF, Doppelt JD, Kephart CJ, Benke MT, Graeter JH, Holmes AS, Haleem-Smith H, Tuan RS, Unger AS. Comparison of minimally invasive direct anterior versus posterior total hip arthroplasty based on inflammation and muscle damage markers. J Bone Joint Surg Am 2011; 93 (15): 1392–8.
- Bragdon CR, Kwon YM, Geller JA, Greene ME, Freiberg AA, Harris WH, Malchau H. Minimum 6-year followup of highly cross-linked polyethylene in THA. Clin Orthop Relat Res 2007; 465: 122–7.
- Breivik H, Borchgrevink PC, Allen SM, Rosseland LA, Romundstad L, Hals EK, Kvarstein G, Stubhaug A. Assessment of pain. Br J Anaesth 2008; 101 (1): 17–24.
- Brooks PJ. Dislocation following total hip replacement: causes and cures. Bone Joint J 2013; 95-B (11 Suppl A): 67–9.
- Bystrom S, Espehaug B, Furnes O, Havelin LI. Femoral head size is a risk factor for total hip luxation: a study of 42,987 primary hip arthroplasties from the Norwegian Arthroplasty Register. Acta Orthop Scand 2003; 74 (5): 514–24.
- Christensen CP, Karthikeyan T, Jacobs CA. Greater prevalence of wound complications requiring reoperation with direct anterior approach total hip arthroplasty. J Arthroplasty 2014; 29 (9): 1839–41.
- Department of Orthopaedic Surgery Haukeland University Hospital. http://nrlweb.ihelse.net/Rapporter/Rapport2014.pdf.
- Downing ND, Clark DI, Hutchinson JW, Colclough K, Howard PW. Hip abductor strength following total hip arthroplasty: a prospective comparison of the posterior and lateral approach in 100 patients. Acta Orthop Scand 2001; 72 (3): 215–20.
- Edmunds CT, Boscainos PJ. Effect of surgical approach for total hip replacement on hip function using Harris Hip scores and Trendelenburg’s test. A retrospective analysis. Surgeon 2011; 9 (3): 124–9.
- Gibson A. Posterior exposure of the hip joint. J Bone Joint Surg Br 1950; 32-b (2): 183–6.
- Graw BP, Woolson ST, Huddleston HG, Goodman SB, Huddleston JI. Minimal incision surgery as a risk factor for early failure of total hip arthroplasty. Clin Orthop Relat Res 2010; 468 (9): 2372–6.
- Gulati A, Dwyer AJ, Shardlow DL. The impact of posterior approach for total hip arthroplasty on early complications. Acta Orthop Belg 2008; 74 (2): 200–5.
- Hardinge K. The direct lateral approach to the hip. J Bone Joint Surg Br 1982; 64 (1): 17–9.
- Holm B, Thorborg K, Husted H, Kehlet H, Bandholm T. Surgery-induced changes and early recovery of hip-muscle strength, leg-press power, and functional performance after fast-track total hip arthroplasty: a prospective cohort study. PLoS ONE [Electronic Resource] 2013; 8 (4): e62109.
- Husby VS, Helgerud J, Bjørgen S, Husby OS, Hoff J. Early maximal strength training is an efficienet treatment for patients undergoing total hip arthroplasty. Arch Phys Med Rehabil 2009; 90 (10): 1658–67.
- Johnston JJ, Noble PC, Hurwitz DE, Andriacchi TP. Biomechanics of the Hip. In: The Adult Hip, Vol. 1. Callaghan JJ, Rosenberg AG, Rubash HE ( eds). Lippincott, Williams & Wilkins, Philadelphia, USA 2007.
- Kortebein P, Symons TB, Ferrando A, Paddon-Jones D, Ronsen O, Protas E, Conger S, Lombeida J, Wolfe R, Evans WJ. Functional impact of 10 days of bed rest in healthy older adults. J Gerontol A Biol Sci Med Sci 2008; 63 (10): 1076–81.
- Lindgren V, Garellick G, Karrholm J, Wretenberg P. The type of surgical approach influences the risk of revision in total hip arthroplasty: a study from the Swedish Hip Arthroplasty Register of 90,662 total hipreplacements with 3 different cemented prostheses. Acta Orthop 2012; 83 (6): 559–65.
- Lombardi AVJr, Skeels MD, Berend KR, Adams JB, Franchi OJ, Do large heads enhance stability and restore native anatomy in primary total hip arthroplasty? Clin Orthop Relat Res 2011; 469 (6): 1547–53.
- Masonis JL, Bourne RB. Surgical approach, abductor function, and total hip arthroplasty dislocation. Clin Orthop Relat Res 2002; (405): 46-53.
- McGuire DK, Levine BD, Williamson JW, Snell PG, Blomqvist CG, Saltin B, Mitchell JH. A 30-year follow-up of the Dallas Bedrest and Training Study: I. Effect of age on the cardiovascular response to exercise. Circulation 2001; 104 (12): 1350–7.
- Meneghini RM, Pagnano MW, Trousdale RT, Hozack WJ. Muscle damage during MIS total hip arthroplasty: Smith-Petersen versus posterior approach. Clin Orthop Relat Res 2006; 453: 293-8.
- Poehling-Monaghan KL, Kamath AF, Taunton MJ, Pagnano MW. Direct anterior versus miniposterior THA with the same advanced perioperative protocols: surprising early clinical results. Clin Orthop Relat Res 2015; 473 (2): 623–31.
- Restrepo C, Parvizi J, Pour AE, Hozack WJ. Prospective randomized study of two surgical approaches for total hip arthroplasty. J Arthroplasty 2010; 25 (5): 671–9. e1.
- Sicard-Rosenbaum L, Light KE, Behrman AL. Gait, lower extremity strength, and self-assessed mobility after hip arthroplasty. J Gerontol A Biol Sci Med Sci 2002; 57 (1): M47–51.
- Smith TO, Blake V, Hing CB. Minimally invasive versus conventional exposure for total hip arthroplasty: a systematic review and meta-analysis of clinical and radiological outcomes. Int Orthop 2011; 35 (2): 173–84.
- Suesada MM, Martins MA, Carvalho CR. Effect of short-term hospitalization on functional capacity in patients not restricted to bed. Am J Phys Med Rehabil 2007; 86 (6): 455–62.
- Suh KT, Park BG, Choi YJ. A posterior approach to primary total hip arthroplasty with soft tissue repair. Clin Orthop Relat Res 2004; (418): 162–7.
- Suter E, Herzog W, Leonard TR, Nguyen H. One-year changes in hind limb kinematics, ground reaction forces and knee stability in an experimental model of osteoarthritis. J Biomech 1998; 31 (6): 511–7.
- Talis VL, Grishin AA, Solopova IA, Oskanyan TL, Belenky VE, Ivanenko YP. Asymmetric leg loading during sit-to-stand, walking and quiet standing in patients after unilateral total hip replacement surgery. Clin Biomech (Bristol. Avon) 2008; 23 (4): 424–33.
- Tsai TY, Dimitriou D, Li JS, Woo Nam K, Li G, Kwon YM. Asymmetric hip kinematics during gait in patients with unilateral total hip arthroplasty: in vivo 3-dimensional motion analysis. J Biomech 2015; 48 (4): 555–9.
- van Stralen GM, Struben PJ, van Loon CJ. The incidence of dislocation after primary total hip arthroplasty using posterior approach with posterior soft-tissue repair. Arch Orthop Trauma Surg 2003; 123 (5): 219–22.
- Verdijk LB, van Loon L, Meijer K, Savelberg HH. One-repetition maximum strength test represents a valid means to assess leg strength in vivo in humans. J Sports Sci 2009; 27 (1): 59–68.
- Winther SB, Foss OA, Wik TS, Davis SP, Engdal M, Jessen V, Husby OS. 1-year follow-up of 920 hip and knee arthroplasty patients after implementing fast-track. Acta Orthop 2015; 86(1): 78–85.
- Witzleb WC, Stephan L, Krummenauer F, Neuke A, Gunther KP. Short-term outcome after posterior versus lateral surgical approach for total hip arthroplasty - A randomized clinical trial. Eur J Med Res 2009; 14 (6): 256–63.
- Wojciechowski P, Kusz D, Kopec K, Borowski M. Minimally invasive approaches in total hip arthroplasty. Ortop Traumatol Rehabil 2007; 9 (1): 1–7.