Abstract
Background and purpose — It has been suggested that preoperative posterior tilt of the femoral head may increase the risk of fixation failure in Garden-I and -II femoral neck fractures. To investigate this association, we studied a cohort of 322 such patients.
Patients and methods — Patients treated with internal fixation between 2005 and 2012 were retrospectively identified using hospital records and the digital image bank. 2 raters measured the preoperative posterior tilt angle and categorized it into 3 groups: < 10°, 10–20°, and ≥ 20°. The inter-rater reliability (IRR) was determined. Patients were observed until September 2013 (with a minimum follow-up of 18 months) or until failure of fixation necessitating salvage arthroplasty. The risk of fixation failure was assessed using competing-risk regression analysis, adjusting for time to surgery.
Results — Patients with a posterior tilt of ≥ 20° had a higher risk of fixation failure: 19% (8/43) as compared to 11% (14/127) in the 10–20° category and 6% (9/152) in the < 10° category (p = 0.03). Posterior tilt of ≥ 20° increased the risk of fixation failure, with an adjusted hazard ratio of 3.4 (95% CI: 1.3–8.9; p = 0.01). The interclass correlation coefficient for angular measurements of posterior tilt was 0.90 (95% CI: 0.87–0.92), and the IRR for the categorization of posterior tilt into 3 groups was 0.76 (95% CI: 0.69–0.81).
Interpretation — Preoperative posterior tilt of ≥ 20° in Garden-I and -II femoral neck fractures increased the risk of fixation failure necessitating salvage arthroplasty. The reliability of the methods that we used to measure posterior tilt ranged from good to excellent.
Several authors have questioned the apparently satisfactory results after internal fixation of undisplaced femoral neck fractures (Rogmark et al. Citation2009, Gjertsen et al. Citation2011). In elderly patients with Garden-I or -II femoral neck fractures, the choice of treatment is internal fixation or primary arthroplasty (Palm et al. Citation2013). Orthopedic surgeons need a reliable predictor that can identify patients who are at risk of failure after internal fixation. Recently, Palm et al. (Citation2009) found that preoperative posterior tilt of the femoral head increased the risk of reoperation after internal fixation of Garden-I and -II fractures, and they suggested a new method for measurement of posterior tilt. Lapidus et al. (Citation2013) were, however, unable to reproduce these findings in a cohort of 382 patients.
We examined the relationship between posterior tilt, fixation failure and avascular necrosis (AVN) after internal fixation of Garden-I and -II femoral neck fractures. We hypothesized that the risk of fixation failure would increase with increasing preoperative posterior tilt.
Patients and methods
The study design was retrospective and observational. We identified internal fixations of femoral neck fractures performed at Akershus University Hospital, Norway, from June 2005 through February 2012. Throughout this period, all femoral neck fractures were treated surgically. Undisplaced fractures (Garden-I and -II) were treated with internal fixation, and an increasing number of displaced fractures were treated with arthroplasty. All patients treated with internal fixation were scheduled for follow-up 3 months after surgery. Any additional follow-up was by physician referral. Patient records for the Garden-I and -II fractures included were reviewed (dating from June 2005 until September 2013). The main outcomes were fixation failure and AVN necessitating revision hip arthroplasty. The term fixation failure was used when revision was indicated due to persistent pain and when radiographs showed loss of screw purchase or non-union. Avascular necrosis was diagnosed when revision was indicated due to persistent pain and when radiographs showed a segmental collapse of the femoral head. Data obtained from patient records were cross-referenced with data from the Norwegian Hip Fracture Register. None of the patients included had surgery at another hospital due to fixation failure or AVN. Removal of the implants because of local discomfort was not regarded as fixation failure.
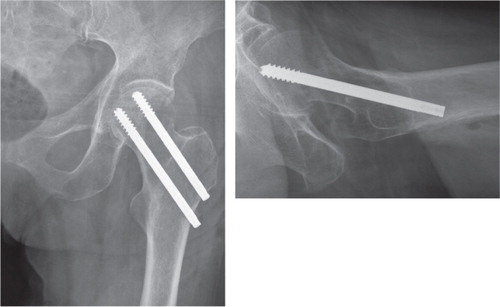
The senior orthopedic resident on call treated patients with Garden-I or -II fractures with closed reduction (if necessary) and internal fixation, inserting 2 cannulated screws parallel to the neck axis (Olmed; DePuy, Warsaw, IN; or Hip Pins; Smith and Nephew, London, UK). The inferior screw was placed so as to minimize screw-calcar distance, and both screws were inserted centrally in the lateral view just short of the subchondral bone (). The perioperative protocol remained unchanged throughout the study period. Patients underwent surgery on a traction table under spinal anesthesia. Dalteparin and cloxacillin (clindamycin where there was penicillin allergy) were given as perioperative prophylaxis. Immediate mobilization was emphasized, and weight bearing was allowed after surgery, as tolerated.
Figure 1. Internal fixation of a Garden I–II femoral neck fracture with 2 parallel cannulated screws.
2 of the authors (FD and SEH), who were blind regarding the outcome, identified 545 femoral neck fractures that were treated with internal fixation and classified the anteroposterior (AP) radiographs using the modified Garden classification (Blundell et al. Citation1998). Garden-I and -II fractures were categorized as undisplaced (383) and Garden-III and -IV fractures were characterized as displaced (162). We excluded 40 patients who lacked true cross-table lateral radiographs. 12 patients who sustained subsequent contralateral undisplaced fractures during the study period were included only once. We also excluded 4 patients who lived abroad, 3 patients with extracapsular fractures, and 2 with combined acetabular and femoral neck fractures. 322 patients were therefore included in the final analysis.
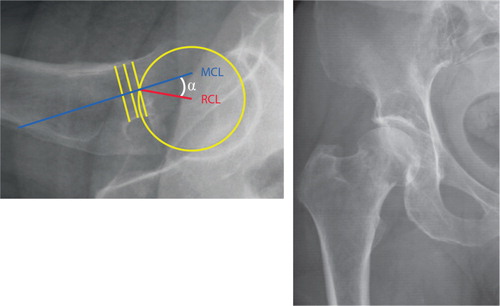
2 of the authors (FD and SEH) measured the posterior tilt angle of the femoral head using the method described by Palm et al. (Citation2009). All measurements were conducted using a software plugin developed for the software mdesk (RSA Biomedical, Umeå, Sweden) (), and both raters were blind regarding the outcome. Angular measurements were recorded with 1 decimal place and divided into 3 categories (< 10°, 10–20°, and ≥ 20°) or 2 (< 20° and ≥ 20°) to allow comparisons with previous studies evaluating the significance of posterior tilt (Lapidus et al. Citation2013, Palm et al. Citation2009). In cases of disagreement between the 2 raters, a third independent orthopedic surgeon evaluated the posterior tilt. Hypothesizing that a simple morphological classification would be as reliable as measuring the posterior tilt angle, radiographs were re-examined following a washout period of 6 weeks (Audige et al. Citation2004) and the fractures were simply described as undisplaced or displaced without measuring the posterior tilt angle. Postoperative posterior tilt was measured in 317 of 322 hips to assess the reduction of the fracture. 5 patients did not have postoperative lateral radiographs (2 in the < 10° category and 3 in the 10–20° category). Implant positioning was evaluated by measuring the minimal distance between the screws and calcar in the AP view, and screws and posterior cortex in the lateral view.
Figure 2. Garden I–II fracture of the right femoral neck. The posterior tilt angle (α) is defined by the mid-collum line (MCL) and the radius collum line (RCL) (Palm et al. Citation2009).
All 322 patient records were reviewed until the time of death or until the time of revision surgery due to fixation failure or AVN. Patients with no such events were observed until the end of the study period, for a minimum of 18 months (February 2012 to September 2013). The mean observational time for all patients was 38 months (range 0–97 months). Mean age was 78 years (SD 10, range 53–97), and 72% of the patients (232 of 322) were women. The survival rate 3 months after surgery was 91% (293 of 322) and 67% (197 of 293) attended the scheduled follow-up. The survival rate after 1 year was 79% (254 of 322).
Statistics
Normal distribution of variables was evaluated using the Shapiro-Wilk test. Groups were compared using ANOVA test for age, and the remaining continuous variables were compared with the Kruskal-Wallis test. Equality of variances was evaluated with Levene’s parametric and non-parametric tests. The chi-square test was used to compare categorical variables between the 3 groups. Inter-rater reliability (IRR) for measurements of posterior tilt are presented as an intraclass correlation coefficient (ICC) using a two-way random effects model with absolute agreement (ICC 2.1) (Weir Citation2005). ICC was interpreted as follows (Cicchetti Citation1994): excellent (> 0.75), fair to good (0.40–0.75), and poor (< 0.40). The inter-rater agreement was evaluated using Cohen’s kappa for 2 categories and weighted kappa, with quadratic weights, for 3 categories. Kappa values were interpreted as suggested by Landis and Koch (Citation1977) and as adapted slightly by Altman (Citation1991): poor (0.00–0.20), weak (0.21–0.40), moderate (0.41–0.60), good (0.61–0.80), and very good (0.81–1.0).
To account for participants dying during the study period, competing-risk regression (CRR) analyses were performed to determine whether there was any association between posterior tilt and fixation failure. Events were defined as time to revision arthroplasty or death. Based on the previous literature, we conducted CRR analyses with the following independent variables: age, sex, ASA classification (Dripps et al. Citation1961), cognitive impairment (as noted in the patient records), time to surgery (from hospital admission to start of surgery), and postoperative posterior tilt. The assumption of proportional hazards was assessed by inspection of log-minus-log and Schoenfeld residuals plots. Multicollinearity was evaluated by examining the variance inflation factor. Competing-risk analysis could not be used to analyze the association between posterior tilt and revision due to AVN. The assumption of proportional hazards was not met, and the sample size was too small to ensure stable statistical models. A minimal adjustment set of covariates was selected using directed acyclic graphs (DAGs) by closing all biasing paths, leaving all causal paths open (Shrier and Platt Citation2008). The DAG diagram was drawn with DAGitty version 2.3 (http://www.dagitty.net; Textor et al. Citation2011). Statistical analyses were performed with R version 3.1.3 for Mac OS X using the R software package cmprsk to run the CRR analysis (Fine Citation1999).
Ethics
The study was reviewed by the Regional Committee for Medical and Health Research Ethics of Norway (reference no. 2013/488). Granting of consent was deemed unnecessary, as the data were to be collected from existing medical records.
Results
31 cases of fixation failure and 13 cases of AVN were identified. All fixation failures occurred during the first year, and all AVNs occurred during the second year or later. 3 patients with fixation failure and 3 patients with AVN declined salvage arthroplasty because of deteriorating health, but they were still included in the final analyses. The frequency of fixation failure was significantly higher in the ≥ 20° category than in the other 2 categories (). Of the 43 patients with a preoperative posterior tilt of ≥ 20°, 22 had their postoperative posterior tilt reduced to 0–10°, 20 had their postoperative posterior tilt reduced to 10–20°, and 1 patient remained in the ≥ 20° group. The frequency of fixation failure in this group of patients (n = 43) was not statistically significantly higher for fractures with a residual postoperative posterior tilt of more than 10° (data not shown). Implant positioning was not significantly different between the 3 groups. The intraclass correlation coefficient for angular measurements of posterior tilt was excellent, and the inter-rater agreement was good for all classification systems ().
Table 1. Patient characteristics, avascular necrosis cases, and fixation failures listed according to preoperative posterior tilt angle (n = 322, with 5 missing cases for postoperative posterior tilt). Values are number of patients (%) unless otherwise stated
Table 2. Inter-rater reliability (IRR) of classification systems for posterior tilt of the femoral head
In univariable competing-risk regression analysis, a preoperative posterior tilt of ≥ 20° significantly increased the risk of fixation failure, with a hazard ratio (HR) of 3.4 (95% CI: 1.3–8.6; p = 0.01) (). Similarly, posterior tilt of ≥ 20° increased the risk of fixation failure using the dichotomous classification. When posterior tilt was classified as undisplaced or displaced without measuring the angle, there tended to be an increased risk of fixation failure for patients with posterior displacement.
Table 3. Risk factors for fixation failure in patients with undisplaced femoral neck fractures. Competing-risk regression analysis with time to fixation failure as outcome (31 failures, n = 322)
Posterior tilt was the only statistically significant predictor of fixation failure in the univariable competing-risk regression analyses ().
Time to surgery was selected for multivariable competing-risk regression based on analysis of directed acyclic graphs (DAGs). Preoperative posterior tilt of ≥ 20° increased the risk of fixation failure, with an HR of 3.4 (95% CI: 1.3–8.9; p = 0.01) adjusted for time to surgery (). Posterior tilt of ≥ 20° was also associated with fixation failure when 2 categories (< 20° and ≥ 20°) rather than 3 were used. In contrast, posterior tilt was not significantly associated with fixation failure when the lateral radiograph was classified as displaced without measuring the angle.
Table 4. Competing-risk regression analyses adjusted for time to surgery, with time to fixation failure as outcome (31 failures, n = 322)
Discussion
We found that the risk of fixation failure was higher for patients with a preoperative posterior tilt of ≥ 20°. When posterior tilt was evaluated without measuring the angle, posterior displacement increased the risk of fixation failure, but the association was not statistically significant. The reliability of the methods used to evaluate posterior tilt was good to excellent.
The importance of posterior tilt is debated, and differences in study design, categorization of posterior tilt, definition of the outcome measure, and length of follow-up make it difficult to compare our results with those from previous studies (Clement et al. Citation2013, Lapidus et al. Citation2013, Palm et al. Citation2009). Differences in study design could explain the diverging reoperation rates for patients with posterior tilt ≥ 20° reported by Palm et al. (Citation2009) (56%) and those reported by Lapidus et al. (Citation2013) (10%). The former was a prospective cohort with 1-year follow-up and the threshold for reoperations may have been lower than in the latter retrospective cohort study with a minimum follow-up of 5 years. In our study, 19% of the patients with posterior tilt ≥ 20° had fixation failure. The 2 above-mentioned studies defined the main outcome as “reoperations due to healing disturbances”. Nevertheless, the first study included 3 peri-implant fractures as fixation failures (Palm et al. Citation2009), whereas Lapidus et al. (Citation2013) excluded 5 patients for whom revision surgery was indicated—but not performed due to medical comorbidity. A third recent trial found that posterior tilt predicted implant failure, but the main outcome measure included removal of screws because of local discomfort (Clement et al. Citation2013).
Greater posterior tilt could possibly cause more posterior comminution, compromising the stability of the fixation. This could explain why a reduction in posterior tilt did not protect against fixation failure. In contrast to fixation failures, AVNs occur later—after the fracture has united. Consequently, Lapidus et al. (Citation2013) detected fixation failures and late-occurring AVNs whereas Palm et al. (Citation2009) mainly included fixation failures. In the present study, the number of patients with AVN was too small to ensure stable statistical models.
We used the simplified dichotomous Garden classification, which is more reliable than the original classification based on 4 categories (Blundell et al. Citation1998, Van Embden et al. Citation2012). Thus, we did not differentiate between Garden-I and -II fractures. Moreover, Lapidus et al. (Citation2013) suggested that Palm et al. (Citation2009) may inadvertently have included displaced fractures by using the less reliable 4-category classification.
The retrospective data collection and the lack of regular follow-up after 3 months were the most important limitations of our study. Consequently, some fixation failures and AVNs may not have been identified. The finding that cognitive impairment tended to reduce the risk of fixation failure could also support the assumption that some failures were not recognized. Pain and discomfort are more difficult to convey for these patients and more difficult to interpret for caregivers. Nevertheless, patients were referred to the hospital depending on symptoms, and the Norwegian Hip Fracture Register was cross-referenced for revision surgeries performed at other hospitals.
Internal fixation and arthroplasty are the 2 main treatment options for elderly patients with femoral neck fractures. Fixation failure is potentially devastating for the patient, and the results after salvage arthroplasty are worse than after primary arthroplasty (Blomfeldt et al. Citation2006, Frihagen et al. Citation2007). Our findings support the idea that preoperative posterior tilt of ≥ 20° increases the risk of fixation failure in elderly patients with Garden-I or -II femoral neck fractures treated with internal fixation. Arthroplasty should be considered in these patients.
FCD and SEH: study design, data collection, data analysis, and preparation of manuscript. MA: data collection, data analysis, and preparation of manuscript. FF, KS, and SEU: data analysis and preparation of manuscript.
No competing interests declared.
We thank Christian Owesen for measuring posterior tilt in cases of disagreement and Peter Mark Jourdan for proofreading and commenting on the manuscript. There was no external funding.
- Altman D. Practical Statistics for Medical Research. Chapman & Hall: London; 1991; 404.
- Audige L, Bhandari M, Kellam J. How reliable are reliability studies of fracture classifications? A systematic review of their methodologies. Acta Orthop Scand 2004; 75 (2): 184–94.
- Blomfeldt R, Tornkvist H, Ponzer S, Soderqvist A, Tidermark J. Displaced femoral neck fracture: comparison of primary total hip replacement with secondary replacement after failed internal fixation: a 2-year follow-up of 84 patients. Acta Orthop 2006; 77 (4): 638–43.
- Blundell C M, Parker M J, Pryor G A, Hopkinson-Woolley J, Bhonsle S S. Assessment of the AO classification of intracapsular fractures of the proximal femur. J Bone Joint Surg Br 1998; 80 (4): 679–83.
- Cicchetti D. Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychol Assessment 1994; 6 (4): 286.
- Clement N D, Green K, Murray N, Duckworth A D, McQueen M M, Court-Brown C M. Undisplaced intracapsular hip fractures in the elderly: predicting fixation failure and mortality. A prospective study of 162 patients. J Orthop Sci 2013; 18 (4): 578–85.
- Dripps R D, Lamont A, Eckenhoff J E. The role of anesthesia in surgical mortality. Jama 1961; 178: 261–6.
- Fine G R. A Proportional hazards model for the subdistribution of a competing risk. J Amer Statist Assoc 1999; 94 (446): 496–509.
- Frihagen F, Madsen J E, Aksnes E, Bakken H N, Maehlum T, Walloe A, et al. Comparison of re-operation rates following primary and secondary hemiarthroplasty of the hip. Injury 2007; 38 (7): 815–9.
- Gjertsen J E, Fevang J M, Matre K, Vinje T, Engesaeter L B. Clinical outcome after undisplaced femoral neck fractures. Acta Orthop 2011; 82 (3): 268–74.
- Landis J R, Koch G G. The measurement of observer agreement for categorical data. Biometrics 1977; 33 (1): 159–74.
- Lapidus L J, Charalampidis A, Rundgren J, Enocson A. Internal fixation of garden I and II femoral neck fractures: posterior tilt did not influence the reoperation rate in 382 consecutive hips followed for a minimum of 5 years. J Orthop Trauma 2013; 27 (7): 386–90; discussion 90-1.
- Palm H, Gosvig K, Krasheninnikoff M, Jacobsen S, Gebuhr P. A new measurement for posterior tilt predicts reoperation in undisplaced femoral neck fractures: 113 consecutive patients treated by internal fixation and followed for 1 year. Acta Orthop 2009; 80 (3): 303-7.
- Palm H, Posner E, Ahler-Toftehoj H U, Siesing P, Gylvin S, Aasvang T, et al. High reliability of an algorithm for choice of implants in hip fracture patients. Int Orthop 2013; 37 (6): 1121–6.
- Rogmark C, Flensburg L, Fredin H. Undisplaced femoral neck fractures–no problems? A consecutive study of 224 patients treated with internal fixation. Injury 2009; 40 (3): 274–6.
- Shrier I, Platt R W. Reducing bias through directed acyclic graphs. BMC Med Res Methodol 2008; 8: 70.
- Textor J, Hardt J, Knuppel S. DAGitty: a graphical tool for analyzing causal diagrams. Epidemiology 2011; 22 (5): 745.
- Van Embden D, Rhemrev S J, Genelin F, Meylaerts S A, Roukema G R. The reliability of a simplified Garden classification for intracapsular hip fractures. Orthop Traumatol Surg Res 2012; 98 (4): 405–8.
- Weir J P. Quantifying test-retest reliability using the intraclass correlation coefficient and the SEM. J Strength Cond Res 2005; 19 (1): 231–40.
