Abstract
Objective: The main objective of the study was to assess the cost and quality of life (QoL) effects of elective dialysis patients during the first year of end-stage renal disease (ESRD) treatment in one Finnish treatment centre.
Methods: A prospective case-series study was performed involving all elective dialysis patients (n=29) in a Finnish dialysis unit during 2003–2004. Direct costs of ESRD treatment were obtained from the hospital database and the Social Insurance Institution. The QoL effects were measured at the initiation of treatment, at 6 and at 12 months using 15D, a generic QoL instrument.
Results: The average cost of ESRD treatment was €69,085. The improvement in the patients' QoL score was statistically and clinically significant during the first treatment year. The most significant changes were seen in the dimensions of breathing and vitality. The condition of patients commencing haemodialysis (HD) was more severe than that of patients commencing peritoneal dialysis (PD) as indicated by worse residual kidney function and poorer quality of life at the initiation.
Conclusions: In this small patient population, treatment of ESRD during the first year seemed to improve or maintain the QoL of the patients.
Introduction
The incidence and prevalence of end-stage renal disease (ESRD) are increasing in the developed countries. This is largely due to the increasing number of patients with diabetes and hypertension, since these diseases are the most common causes of chronic kidney failure progressing to ESRDCitation1. The prevalence of ESRD in the Finnish population was 725/million inhabitants in 2007 and the incidence was 92/million inhabitants. The mortality related to ESRD was 94/1000 patient years in 2007Citation2.
The treatment of ESRD in Finland is organised in dialysis units that are mostly located in central or university hospitals. In addition, there are self-care and institution satellite haemodialysis units. The dialysis modality is selected for each patient during the individual predialysis programme in co-operation with the nephrologist, predialysis nurse and the patient. Those patients starting acute dialysis (not previously known by the nephrological unit) come to the ESRD programme from outside the predialysis programme. The percentage of these patients varies from centre-to-centre and over time. Accurate data for these patients are not available in Finland.
Of the ESRD patients receiving treatment in Finland during 2007, approximately 32% received haemodialysis (HD), 8% peritoneal dialysis (PD) and 60% received treatments related to functioning renal transplants. The first treatment for new patients was HD in approximately 76%, and PD in approximately 24%, of the patientsCitation2. In Finland the proportion of patients on home haemodialysis was 4% at the end of 2006Citation3.
The yearly treatment costs for ESRD are known to be high and they have been studied in many countriesCitation4–10. In this study, the objective was to evaluate the cost and the quality of life effects of ESRD treatment during the first treatment year in elective dialysis patients at one Finnish treatment centre.
Patients and methods
The study was a prospective observational case-series study in Kuopio University Hospital, Finland. The dialysis treatment centre consists of the main dialysis unit in the Kuopio University Hospital and two satellite haemodialysis units. These dialysis units treat all ESRD patients in the population of the surrounding district of 249,000 inhabitants. Ethical approval for this study was obtained through the Kuopio University Hospital Ethics Board (decision number 48/2003) and the study was carried out in compliance with the Declaration of Helsinki.
All incident renal patients (n=32) starting their dialysis treatment at the department during the study period (from May 2003 until September 2004) were invited to participate in the study. Informed consent was obtained from 29 patients, of whom two withdrew from the study before the end of the follow-up period of 1 year. Three patients, all initiating on HD, refused to participate in the study.
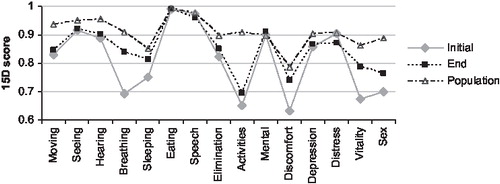
Patients' quality of life (QoL) was assessed using 15DCitation11 at the treatment initiation, at 6 months and at 12 months. The 15D instrument measures health status with 15 dimensional domains (mobility, vision, hearing, breathing, sleeping, eating, speech, elimination, usual activities, mental wellbeing, discomfort, depression, distress, vitality and sexuality) that are further divided into 5 items. 15D is a composite tool which yields a 15-dimension health profile and an overall QoL index score. 15D has been used previously in dialysis assessmentsCitation10,12.
The included cost estimates in this study were chosen from a healthcare payer perspective. All use of healthcare resources and their costs during the study period were collected from the hospital databases using micro-costing approach (see, for example, Swindle et al Citation13). Pharmaceutical expenditures and travelling costs were obtained from the Social Insurance Institution (SII), which is the authority responsible for the reimbursement of medical and travelling expenditures in Finland. All costs were estimated in euros using the year 2004 price level. Discounting was not considered, since the follow-up time was only 1 year.
Due to the small size of the study population the possible differences between treatment groups were not analysed. The differences in the quality of life at the base-line and at the end of first treatment year were evaluated using the Wilcoxon signed-rank test. All statistical analyses were performed using Intercooled Stata version 9.2.
Results
Patient characteristics
The median age of the study patients was 55 years with about equal numbers of women and men (52% men). The most common aetiologies of ESRD in the study population were type 1 diabetic nephropathy and polycystic renal disease (21% each) followed by chronic glomerulonephritis and nephrosclerosis (17% each). Almost all patients suffered from hypertension (97%) and the majority also had hyperlipidaemia (62%). None of the patients participating in the study died during the study period. However, one of the refusing patients died shortly after being invited to participate.
The treatment modalities of the patients in this study were haemodialysis (HD), peritoneal dialysis (PD) and kidney transplant. The majority of the study patients were initially treated with HD (66%). During the study period there were switches to other treatment modalities in 38% of the patients. Nevertheless, the proportion of patients receiving HD remained at 66% at the end of the study period.
The clinical characteristics of the study patients are presented in . The dialysis modality was selected during the individual predialysis programme in co-operation with the nephrologist, predialysis nurse and the patient. The patients starting PD treatment had better residual kidney function and higher haemoglobin and serum albumin levels and had diabetes more often than the patients starting HD treatment. During the follow-up period, 14 of the 19 HD patients continued the whole follow-up period with that treatment, while two of them received a kidney transplant (Tx). One patient switched to PD treatment for a short time and one patient restored his own kidney function. Among the ten PD patients, four continued with PD for the whole period, four switched to HD (of whom one had an unsuccessful Tx) and three had a Tx. Altogether, five patients received a transplant during the follow-up period. The treatment periods for HD, PD and Tx were 201, 95 and 20 months, respectively.
Use of healthcare resources and related costs
The mean total cost of ESRD-treatment in this study was €69,085 (SE 3,366; 95% CI: 62,178–75,992). This cost was calculated on the basis of the resources used, which are shown in , along with the mean total cost and average cost of each resource type.
There are differences in the use of resources in patients receiving PD and HD. HD patients have naturally more outpatient treatment visits (on average nearly 3 per week) and therefore incur more travel expenses than the patients receiving PD. However, the opposite is true for the use of pharmaceuticals purchased from pharmacies. In the study, the yearly travelling expenses (paid partly by the SII and partly by the patient) were €3,135 (SE 942; 95% CI: 908–5 363) for PD and €11,214 (SE 2,184; 95% CI: 6,560–15,869) for HD. With respect to pharmaceuticals (including PD solutions), the yearly costs were 23,076 (SE 1,482; 95% CI: 19,571–26,580) and €8,062 (SE 1,222; 95% CI: 5,457–10,668) in the PD and HD groups, respectively. The mean total costs were €55,743 (SE 6,379; 95% CI: 40,661–70,826) for patients receiving PD and 77,126 (SE 3 099; 95% CI: 70,480–83,773) for patients receiving HD as the initial treatment modality (excluding the transplant patients and the one patient with restored kidney function).
Quality of life
The 15D questionnaire was returned by all of the 29 patients at the beginning of the study period and by 27 of the patients at 6 and 12 months (two patients did not return the follow-up questionnaires at 6 and 12 months).
The QoL of ESRD-patients improved during the dialysis treatment. The mean 15D score was 0.797 (95% CI: 0.752–0.842) at the time of first dialysis visit. At the end of the year, the corresponding score was 0.828 (95% CI: 0.780–0.875). The end-of-year 15D score was slightly lower compared to the mid-year value of 0.832 (95% CI: 0.787–0.876). According to the Wilcoxon signed-rank test, the QoL distributions at the treatment initiation and at the end of the year were different (p=0.0396). The effect of treatment was clinically significant since the difference between the initial 15D score and end-of-year 15D score was greater than the minimum important difference (MID) of |0.030|Citation11.
The 15D profile at the treatment initiation and at the end of the first treatment year compared to the Finnish population in the year 2000Citation14 is shown in . When comparing the initial and the end values of 15D items, the greatest effects are seen in the breathing, sleeping, discomfort, vitality and sexual dimensions of QoL. According to the Wilcoxon signed-rank test, the changes in the breathing (p=0.0049) and vitality (p=0.0312) dimensions were significant at 0.05 level.
The differences in the QoL between treatment modalities could not be analysed from the data due to the small study size and the treatment modality switches. The QoL of patients at the treatment initiation was lower in the HD group (mean 0.775, 95% CI: 0.706–0.844) than PD group (mean 0.846, 95% CI: 0.799–0.893). When the QoL at the end of the study period was assessed according to the actual treatment modality at the time, the QoL was again lower in the HD group (0.779, 95% CI: 0.715–0.843, n=16) followed by the PD group (mean 0.912, 95% CI: 0.888–0.935, n=5) and patients who had a functioning renal transplant (mean 0.913, 95% CI: 0.858–0.967, n=4).
Discussion
ESRD is a heavy burden to both patients and society, because the treatment is expensive and entails a major life change for the patients. This study assesses the changes in the QoL of the patients and the costs associated with ESRD treatment of elective dialysis patients in one Finnish treatment centre during the first treatment year.
In the study, the mean total cost of ESRD-treatment was €69,085. The obtained estimate is in line with previous Finnish studies that reported the cost of HD and PD to be in the range of €38,932–64,566 and €28,069–62,279, respectivelyCitation7,8. As expected, this figure is notably higher than the estimates of €38,477 and €39,781 reported by Malmström et al Citation10 for home haemodialysis and self-care satellite dialysis, respectively. Due to the small number of patients in the current study, the cost of different treatment modalities could not be analysed statistically. An intention-to-treat analysis indicated that differences in costs might exist.
On average, the QoL of ESRD patients in the current study improved during the first year of dialysis treatment. The improvements in breathing and vitality dimensions of the 15D instrument were statistically significant. Unfortunately, reliable comparisons between treatment modalities could not be made. According to the study results, patients initiating on HD had a poorer QoL than PD patients at the treatment initiation which is in accordance with their clinically more severe condition (i.e., lower Hb and albumin levels and lower residual kidney function at the start of dialysis treatment). The QoL of those patients who had a renal transplant or PD as their treatment modality at the end of the first year was surprisingly good, as they had achieved the same level as the average QoL in the Finnish population (0.91 in year 2000).
To place the obtained QoL figures into perspective, the scores of HD patients during the study period were similar to those of Finnish patients with Parkinson's disease (0.748), heart failure (0.773) or stroke (0.801) whereas the QoL figures for patients on PD at the treatment initiation were similar to patients with chronic obstructive pulmonary disease (0.843), arthrosis of hip or knee (0.844) or asthma (0.864)Citation15. In the study by Saarni et al Citation15 reporting the QoL of Finnish patients with 25 specified diseases and conditions, Parkinson's disease had the largest negative impact on the health-related QoL at the individual level. Thus, our study results suggest that the impact of ESRD on the QoL of some of the affected patients is likely to be one of the highest of all diseases and conditions.
Conclusions
The ESRD treatment improves or maintains the QoL of the patients compared to the QoL at the initiation of treatment. There may be cost preferences for PD over HD, but due to the very limited number of patients in our study, this could not be reliably analysed. Perhaps a larger, well controlled clinical trial in more than one Finnish treatment centre could resolve this problem.
Table 1. Clinical characteristics of the 29 incident dialysis patients at baseline.
Table 2. The average use of resources and related costs for the first year of renal replacement therapy, in euros (excl. VAT).
Acknowledgements
Declaration of interest: None disclosed. We would like to thank Minna Hyvärinen, the head nurse of the dialysis unit at the Kuopio University Hospital, for her efforts in data gathering and retrieval from the hospital databases. A research grant from Kuopio University Hospital was received, grant 5102506.
References
- Bommer J. Prevalence and socio-economic aspects of chronic kidney disease. Nephrol Dial Transplant 2002;17(Suppl 11):8-12.
- Suomen munuaistautirekisteri, Finnish Registry for Kidney Diseases: Vuosiraportti 2007, Annual Report 2007. Helsinki, 2008.
- Honkanen EO, Rauta VM. What happened in Finland to increase home hemodialysis? Hemodial Int 2008;12(Suppl 1.:S11-15.
- Shih Y, Guo A, Just P, et al. Impact of initial dialysis modality and modality switches on Medicare expenditures of end-stage renal disease patients. Kidney Int 2005;68:319-329.
- Joyce A, Iacoviello J, Nag S, et al. End-stage renal disease-associated managed care costs among patients with and without diabetes. Diabetes Care 2004;27:2829-2835.
- Sandoz M, Ess S, Keusch G, et al. Prevalence and direct medical costs of end-stage renal disease in patients with type 2 diabetes mellitus in Switzerland for 2001. Swiss Med Wkly 2004;134:448-458.
- Salonen T, Reina T, Oksa H, et al. Cost analysis of renal replacement therapies in Finland. Am J Kidney Dis 2003;42:1228-1238.
- Salonen T, Reina T, Oksa H, et al. Alternative strategies to evaluate the cost-effectiveness of peritoneal dialysis and hemodialysis. Int Urol Nephrol 2007;39:289-298.
- Kontodimopoulos N, Niakas D. An estimate of lifelong costs and QALYs in renal replacement therapy based on patients' life expectancy. Health Policy 2008;26:85-96.
- Malmström RK, Roine RP, Heikkilä A, et al. Cost analysis and health-related quality of life of home and self-care satellite haemodialysis. Nephrol Dial Transplant 2008;23: 1990-1996.
- Sintonen H. The 15D instrument of health-related quality of life: properties and applications. Ann Med 2001;33:328-336.
- Yildirim A. The importance of patient satisfaction and health-related quality of life after renal transplantation. Transplant Proc 2006;38:2831-2834.
- Swindle R, VanDensen Lukas C, Meyer DA, et al. Cost analysis in the Department of Veteran Affairs, consensus and future directions. Med Care 1999;37(Suppl):3-8.
- National Public, Health Institute. The Finnish Health 2000 Survey data. Helsinki, 2006.
- Saarni SI, Härkänen T, Sintonen H, et al. The impact of 29 chronic conditions on health-related quality of life: a general population survey in Finland using 15D and EQ 5D. Qual Life Res 2006;15:1403-1414.