Abstract
Background: Bipolar I disorder is a recurrent illness that affects 1% of the US population and constitutes a large economic burden. Few studies have investigated the cost-effectiveness of maintenance treatment options. The objective of this analysis was to assess the cost-effectiveness of quetiapine (QTP) in combination with lithium (Li) or divalproex (DVP) compared with that of Li or DVP alone for maintenance treatment of bipolar disorder.
Methods: The cost-effectiveness of maintenance treatment with QTP in combination with Li or DVP was compared with placebo (PBO) in combination with Li or DVP from a US direct costs perspective using a Markov model. The model simulated a cohort of 1,000 stabilized patients with bipolar I disorder and estimated the quarterly risk in three health states: euthymia, mania, and depression. Efficacy data were derived from two randomized, double-blind, placebo-controlled trials comparing QTP + Li/DVP with PBO + Li/DVP for up to 2 years. Resource data were obtained from published literature. Direct costs included drug costs, hospitalizations, and physician visits. Outcomes and costs were discounted at 3% and the price reference year was 2007. Endpoints included the number of acute mood episodes, hospitalizations due to an acute mood event, and costs per quality-adjusted life-years. A probabilistic sensitivity analysis (PSA) was conducted to evaluate uncertainty.
Results: In the base-case analysis, QTP + Li/DVP dominated PBO + Li/DVP. The PSA showed these results to be robust. In addition, treatment with QTP + Li/DVP was associated with reductions in acute manic episodes (46%), acute depressive episodes (41%), and related hospitalizations (44%) compared with PBO + Li/DVP.
Conclusions: These analyses, based on two randomized clinical trials, suggest that QTP + Li/DVP is a cost-effective maintenance treatment option for patients with bipolar I disorder compared with Li or DVP alone.
Introduction
Conceptualized as a spectrum of mood disorders, bipolar disorder has distinct subtypes, which have been categorized by the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR) as: (1) bipolar I disorder, (2) bipolar II disorder, (3) cyclothymia, and (4) bipolar disorder not otherwise specifiedCitation1. Among these subtypes, bipolar I disorder is the most common, with a lifetime prevalence of 1%, based on a nationally representative sample in the USCitation2.
Bipolar I disorder is a serious and persistent disorder characterized by unpredictable episodes of mania, hypomania, mixed mood, major depression, and euthymia. Patients experience episodes of mania, depression, or mixed episodes with intervals of normal moodCitation1. It has a severe impact on patients, their families, and society in terms of personal and socio-occupational functioningCitation3,4. Affected patients are at increased risk of suicide – approximately 20 times more than the general populationCitation4 – as well as increased risk of other medical conditions including substance abuse, diabetes, and obesityCitation5. Misdiagnosis or delay in diagnosis of bipolar disorder is common; a recent study found that 37–40% of patients with a hospital discharge diagnosis of bipolar disorder had been considered to have unipolar depression prior to admissionCitation6. Misdiagnosed patients are treated with pharmacologic interventions that can worsen the clinical course of disease including the onset of rapid cyclingCitation6. Both misdiagnosis and delay in diagnosis contribute to the economic burden of bipolar I disorder.
In the US, the annual cost of bipolar disorder has been estimated to be $45 billion, of which $7 billion was attributed to direct medical costs including non-treatment-related expenditures and $37 billion to indirect costsCitation7. The average lifetime treatment cost per patient is thought to range from $11,720 for patients with a single manic episode to $624,785 for patients with nonresponsive/chronic episodesCitation8. Most of the costs associated with bipolar disorder are due to inpatient costs in the first year following diagnosis, followed by charges for outpatient physician visitsCitation9. This pattern highlights not only the significant overall economic burden of bipolar disorder, but also the economic importance of preventing acute mood episodes.
Treatment of bipolar I disorder can involve both psychosocial and pharmacologic interventions. Common clinical treatment goals include the control of acute mood episodes and the reduction in risk of future episodesCitation10. The latter goal, however, remains elusive for most patients. Pharmacologic therapies, which include lithium (Li), anticonvulsants, and atypical antipsychotics, have demonstrated varying efficacy in the maintenance treatment of bipolar disorderCitation11.
The atypical antipsychotic quetiapine (QTP) has demonstrated long-term efficacy in the maintenance treatment of bipolar I disorderCitation12–14. Two double-blind, placebo-controlled clinical trials with a 2-year follow-up period, found that QTP in combination with Li or divalproex (DVP) for maintenance treatment demonstrated superior efficacy (measured as the increased time to recurrence of acute episodes) than treatment with placebo (PBO) and Li or DVP in recently stabilized patients with bipolar I disorderCitation13,14. These findings were significant irrespective of the polarity of the index episode (mania, mixed, or depression).
Amid increasing healthcare expenditures and limited resources, assessing the value of new therapies – in terms of costs and consequences – is important to clinicians and healthcare decision makers. The cost-effectiveness of QTP for maintenance treatment of bipolar I disorder has not yet been reported. We therefore conducted a cost-effectiveness analysis of QTP or PBO in combination with Li/DVP from the two maintenance clinical trials.
Methods
Model overview
A Markov model of bipolar I disorder maintenance treatment was developed to estimate the clinical and economic outcomes associated with the disease and its treatment. Efficacy data were derived from two randomized clinical trials that compared QTP + Li/DVP to PBO + Li/DVP for maintenance treatment of bipolar I disorderCitation13,14. Data for other model inputs were obtained from the published literature. A cost-utility analysis was conducted to simulate the impact of treatment on clinical outcomes and costs over a 2-year time horizon. Only direct costs were considered. A discount rate of 3% was applied to all costs and outcomesCitation15. The model was developed in MS Excel 2003 (Microsoft, Redmond, WA, USA).
Quetiapine clinical trials
The pivotal QTP trials were randomized, multicenter, parallel-group, flexible dose, double-blind, placebo-controlled phase III studiesCitation13,14. A total of 3,414 patients were enrolled for up to 104 weeks’ duration. Patients were eligible if they had experienced an acute mood event within 26 weeks of study enrolment. Patients first entered an open-label, pre-randomization, stabilization treatment phase and were given QTP and Li or DVP for a period of 12–36 weeks. Eligibility criteria for study randomization required patients to: (1) have been prescribed QTP (dose range 400–800 mg/day) and either Li or DVP for at least 12 weeks during the pre-randomization phase; and (2) have reached clinical stability, defined as Young Mania Rating Scale (YMRS) total score ≤12 and Montgomery-Åsberg Depression Rating Scale (MADRS) total score ≤12, assessed at a minimum of four consecutive visits spanning at least 12 weeks in the pre-randomization phase. Patients were then randomized to QTP (flexible dosing between 400 and 800 mg/day, at the discretion of the investigator) or placebo plus Li (trough serum concentration of 0.5–1.2 mEq/L) or DVP (50–125 μg/mL). Patients were excluded from randomization if they had: (1) been hospitalized due to a mood event (mania, depression, or mixed), (2) been administered electroconvulsive therapy, (3) attempted suicide, or (4) abused alcohol or substances during the pre-randomization phase.
The primary study endpoint for both trials was time to recurrence of any mood event, defined as: (1) initiation of an antipsychotic, antidepressant, or mood stabilizer other than the assigned regimen to treat mixed, manic, or depression symptoms; (2) psychiatric hospitalization; (3) YMRS or MADRS scores ≥20; or (4) study discontinuation due to a mood event. Safety was monitored during the trials by clinical observations and laboratory testing of blood and urine samples.
Baseline and clinical efficacy results of the pivotal QTP trials are presented in and . Approximately 46% of the pooled study populations were assigned Li and 54% were assigned DVP. For the economic model, patient data were grouped into three categories: (1) patients who experienced an acute mania event, (2) patients who experienced an acute depression event, and (3) patients who discontinued (not due to a mood event). Across both studies, 646 patients were randomized to QTP + Li/DVP and 680 patients to PBO + Li/DVP (). The number of observed acute manic episodes was 58 and 157, and the number of observed acute depressive episodes was 67 and 186 in the pooled QTP and the pooled PBO treatment groups, respectively ().
Table 1. Baseline characteristics of randomized quetiapine clinical trials (Studies 126 and 127)Citation13,14.
Table 2. Outcomes of randomized quetiapine clinical trials (Studies 126 and 127)Citation13,14.
Model structure
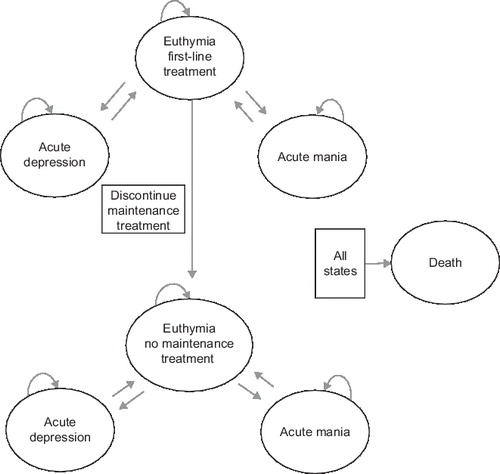
An overview of the model structure is presented in . The model health states are stratified by treatment status (i.e., patients who were ‘on maintenance treatment’ or who ‘discontinued maintenance treatment’). Within each treatment status, there are three health states in the model: (1) euthymia, (2) acute mania, and (3) acute depression. Costs and outcomes associated with discontinuing maintenance treatment have been simulated by allowing patients to switch from the ‘maintenance’ to the ‘no maintenance’ treatment arm.
Based on the characteristics of patients in the randomized clinical trials, the base-case model is populated with a hypothetical cohort of 1,000 stabilized patients with bipolar I disorder. The model does not apply to patients who have not been stabilized on QTP and Li/DVP since patients enter the model only after they have achieved successful stabilization of mood events and are assigned to the euthymic state upon entry.
In subsequent cycles, patients may remain in the euthymia state or experience an acute depression or acute mania event, either on or off maintenance treatment. Once off maintenance treatment, discontinued patients remain off maintenance treatment. However discontinued patients, who experience an acute mood event, are treated for the acute mood event. Treatment for acute mood episodes was dependent on the treatment (Li or DVP) originally assigned. For example, patients initially assigned to Li were switched to treatment with DVP for acute manic episodes, and vice versa. In addition, patients assigned to PBO and Li/DVP were treated with 600 mg/day of QTP in the event of an acute mania event. Treatment for an acute depression episode consisted of 200 mg of lamotrigine, irrespective of treatment assignment at randomization.
Patients were followed for eight quarterly cycles (total of 2 years), corresponding to the follow-up period in the QTP clinical trials. All-cause mortality and suicide were also included in the model to account for the risk of suicide in the bipolar I disorder patient population. Mortality was determined by averaging the annual age- and sex-specific mortality rates in the US population from 2004 US death tables and then adjusting for the suicide rate observed in the bipolar disorder patient populationCitation16,17. However, these rates were not adjusted based on the acute manic and depressive episodes observed in QTP + Li/DVP and PBO + Li/DVP. We assumed mortality rates were equivalent in both treatment arms.
Model assumptions
A number of key assumptions were made in constructing the model. First, patients who experience an acute mood event transition to the euthymic state, prior to experiencing another acute mood event. Second, patients who discontinue treatment have the same risk for acute mood events as patients on the ‘no maintenance’ treatment option. Third, patients who discontinue treatment remain off treatment unless they relapse, at which time they are treated for an acute mood event. Finally, each cycle lasts 3 months to account for the average duration of acute mania and depression episodes.
Transitional probabilities
Transitional probabilities were derived from the QTP clinical trials and the literature (). For QTP + Li/DVP and PBO + Li/DVP, we estimated the rates of (1) acute mania episodes, (2) acute depression episodes, and (3) discontinuations (not due to mood events), using the pooled data and the pooled number of person-days from the QTP clinical trials. The rates of these acute mood events were converted to quarterly transitional probabilities using published methodologyCitation18. The transitional probabilities of the ‘no maintenance’ treatment option, which accounts for patients who have discontinued treatment, were abstracted from Calabrese et al, 2003 (a placebo-controlled, double-blind, randomized trial which evaluated the efficacy of lamotrigine and lithium maintenance treatment for recently depressed bipolar I disorder patients) and adjusted based on input from clinical expertsCitation19.
Table 3. Quarterly transitional probability estimations.
Health state utilities
Health state utilities were derived from Calvert et al, 2006Citation20. The authors determined utility values using Medical Outcomes Study 36-Item Short Form (SF-36) data from the lamotrigine pivotal trialsCitation20,21 and multivariate model-based algorithms that estimate a preference-based measure of health from the SF-36, as reported by Brazier et al Citation1. Specific utility values were derived for acute depression (0.4), acute mania (0.7), and euthymia (0.8).
Resource-use estimate
The resource-use data for different health states were obtained from Calvert et al, 2006 ()Citation20. The model included: (1) drug costs for maintenance treatment, (2) drug and hospitalization costs for acute mania and depression episodes, (3) costs of physician monitoring, and (4) diagnostic testing costs. Cost data for drugs were updated using the Red Book 2007 Citation22. The average whole price (AWP) was adjusted by 30% to account for potential rebates and discounts which are often negotiated between payers and drug manufacturers. All cost data were inflated to 2007 cost values using the US consumer price indexCitation23.
Table 4. Model inputs and sources.
Sensitivity analysis
Sensitivity analyses identified parameters with the greatest influence on model results. Sensitivity analyses independently alter the value of each parameter across the range of plausible values for that parameter. For the one-way sensitivity analysis, the following model parameters were varied (by + 50%) one at a time: (1) all components of costs, (2) utilities, (3) percentage of patient hospitalizations for acute mood events, (4) number of hospitalization days for acute mood events, and (5) physician monitoring time costs for acute manic and acute depressive episodes.
A scenario analysis was also conducted to evaluate the transition probabilities for QTP + Li/DVP and PBO + Li/DVP treatment groups. The transition probability of euthymia was varied from 0.997 (best-case scenario) to 0.001 (worst-case scenario) for both comparators; transition probabilities for mania, depression, and discontinuation were varied from 0.001 (best-case scenario) to 0.333 (worst-case scenario), to ensure that the sum of transition probabilities for a given scenario summed to 1.
A probabilistic sensitivity analysis (PSA) using Monte Carlo simulation was performed to evaluate the impact of uncertainty around clinical and resource utilization parameters on the model results. PSA involves specifying distributions for model parameters to represent uncertainty in their estimation. A random sample is then taken from each of the parameter distributions and used to calculate the expected costs and clinical outcomes for that combination of parameter values. All model parameters, except drug costs, were included in the analysis. Ranges for the PSA were calculated from the means and the standard deviations of the parameters. The final model was further verified for internal validity by a modeler external to the study team and for external validity by a clinical expert in bipolar disorder.
Results
Base-case treatment analysis
For the hypothetical cohort of 1,000 patients aged 40 years and treated over 2 years (eight cycles), the model estimated that patients treated with QTP + Li/DVP experienced a 46% decrease in acute manic mood episodes and a 41% decrease in acute depressive episodes compared with PBO + Li/DVP (). Treatment with QTP + Li/DVP was also associated with a 44% decrease in hospitalizations for an acute mood event. Numbers of acute mood events, hospitalizations, and euthymic days are summarized in .
Table 5. Clinical outcomes over 2-year period (eight cycles) of the model for a cohort of 1,000 simulated patients.
The model estimated that the direct costs of treatment with QTP + Li/DVP were $9,604 and resulted in an increase of 1.491 quality-adjusted life-years (QALYs) per patient over 2 years compared with $10,731 and 1.440 QALYs per patient for treatment with placebo + Li/DVP over the same time period (). The incremental cost-utility ratio indicated that QTP + Li/DVP dominated PBO + Li/DVP.
Table 6. Results – QTP + Li/DVP vs. placebo + Li/DVP*.
Sensitivity analysis
The sensitivity analysis determined parameters with the greatest influence on model results (). The most sensitive parameters, in order of influence, were: cost of QTP; percentage of patients hospitalized for acute manic mood events, average days of hospitalization for manic episodes, average cost of inpatient treatment per day for a manic episode, cost of DVP, and percentage of patients hospitalized for acute depressive episodes. In the best-case scenario analysis in which the transition probability of euthymia for QTP + Li/DVP was assumed as a certainty, QTP dominated PBO + Li/DVP; likewise, identical results were observed in the best-case scenario analysis for PBO + Li/DVP (). As expected, in the worst-case scenario analysis which assumed the transition probability of euthymia for QTP + Li/DVP was 0.001, QTP was dominated by PBO + Li/DVP.
Table 7. One-way sensitivity analyses results: six most influential parameters in the model.
Table 8. Scenario analyses results.
The PSA demonstrated that in light of uncertainty around model variables, QTP + Li/DVP is cost effective. The results of the PSA, presented in , indicated that approximately 50% of the scenarios are located in the lower right quadrant (i.e., costs of maintenance treatment with QTP + Li/DVP are lower and benefits are higher) where PBO + Li/DVP is dominated by QTP + Li/DVP. The other 50% of scenarios are located in the upper right quadrant, in which costs of maintenance treatment with QTP + Li/DVP are higher and benefits are higher as compared to PBO + Li/DVP. The most extreme point in this quadrant still remained within the threshold of cost-effectiveness. This is below the widely cited benchmark of $50,000/QALY or the recently suggested $100,000/QALY to determine the cost-effectiveness of treatmentsCitation24,25.
Discussion
Bipolar disorder poses a significant economic burden on patients, their families, and society. Few studies, however, have investigated the cost-effectiveness of maintenance treatmentsCitation20,26,27. This study is the first to evaluate the cost-effectiveness of QTP in combination with Li or DVP for the maintenance treatment of bipolar I disorder. Based on the results of two, 2-year randomized clinical trials, our model indicates that continuation of maintenance treatment with QTP + Li/DVP results in significant decreases in the number of acute mood episodes and subsequent hospitalizations, and is a cost effective treatment option compared with PBO + Li/DVP.
The sensitivity analyses identified the most influential drivers of the model; among them were transitional probabilities for both treatment comparators, cost of quetiapine, average days of hospitalization for manic episodes, percentage of patients hospitalized for acute manic mood events, and average cost of inpatient bed per day for manic episode. PSA of the model showed that, despite uncertainty around parameter values, QTP + Li/DVP is cost effective.
There is substantial variability in the literature regarding the length of hospitalization associated with acute mood episodes, the percentage of patients hospitalized for acute mood episodes, and the duration of acute mood episodes. Estimates of the duration of acute mood episodes vary from 30 days to 69.3 days for acute manic episodes and 75 days to 149.1 days for acute depressive episodesCitation20. Hospitalization rates due to acute mood episodes ranged from 18% to 44%Citation24,28. We assumed that the average hospital stay for mania was 11.3 days and 8.3 days for depressionCitation20; however, the 2005 National Hospital Discharge Survey reports that a mean length of inpatient stay is 7.7 days in short-stay hospitals for adults aged 45–64 years with a first-listed discharge diagnosis of major depressive disorderCitation29. The implication of the variability of these factors was evaluated in the sensitivity analysis. Hospitalization due to acute mood episodes and average days of hospitalization for manic episodes were among the most influential parameters in the model, while changing the duration of acute mood episodes did not significantly affect the results.
Additional variability was present for health state utilities of bipolar I disorder patients experiencing acute mood episodes. Estimates are stratified by the severity of the episode and range from 0.53 to 0.70 for acute mania and 0.4 to 0.63 for acute depressionCitation20,30,31. The sensitivity analyses, however, determined the impact of health state utility variability to be non-influential. Conversely, we assumed that all patients, irrespective of treatment group, experienced the same risk of suicide in the general bipolar patient population. We believe that this is a conservative approach because patients in the PBO + Li/DVP treatment group would likely experience a higher risk of suicide than QTP + Li/DVP.
One strength of this economic evaluation was that it was based on randomized clinical trials. Access to clinical trial data allowed us to model patient characteristics and estimate transitional probabilities explicitly. A second strength of this study was its simple design, which increased the model's transparency.
Limitations
The analysis has several limitations, the first of which is the generalizability of the results to the bipolar I patient population outside a clinical trial setting. The patients enrolled in the clinical trials had been stabilized on a combination of QTP + Li/DVP during a 12-week pre-randomization phase. While this is a standard approach in the clinical research design of maintenance studies, such an approach may have increased the internal validity at the expense of external validity. Similarly, patient adherence to treatment may vary between the controlled clinical trial setting and clinical practice, thus efficacy observed during a clinical trial may not translate to clinical practice.
Secondly, potential limitations arise from the assumptions made in the model. The model did not account for patients who may have switched maintenance treatments. Patients were assumed to remain on their assigned maintenance treatment for the duration of the model unless they discontinued (not due to a mood event). Although the probability of discontinuation, which captures the impact of adverse events on treatment discontinuation, was modeled, adverse events and their associated costs were not explicitly taken into account.
Third, for patients who discontinue maintenance treatment, the present model employed the relapse rates observed in the patients who discontinued maintenance treatment from the PBO group of the lamotrigine and lithium maintenance studyCitation19. The population in that study was recently depressed patients and the study inclusion criteria were less stringent than those employed in the QTP clinical trials. These differences in study populations may falsely increase the rate of relapse in patients who discontinue PBO + Li/QTP or QTP + Li/QTP treatment in the model. However, as the transition probability of maintenance treatment discontinuation from QTP + Li/DVP treatment is higher than with PBO + Li/DVP, the application of the relapse rates of the PBO group from the lamotrigine/lithium study is probably a conservative assumption.
Fourth, we employed average resource-use estimates abstracted from the literature. This approach has been employed in previous economic evaluations. However, it should be noted that a bottom-up costing method may have facilitated a more detailed assessment of resource use and consequently, varied the results of this economic evaluation. A final assumption was that patients who experienced an acute mood episode transitioned into the euthymia state before experiencing another acute mood event. We acknowledge that the clinical course for bipolar I disorder patients may be varied; many, if not most, patients transition directly into hypomania and then mania or mixed states. It should be noted that patients with mixed episodes were reclassified primarily as manic or depressed based upon the predominant nature of the mood symptoms as judged by the investigators. Lastly, this study does not account for the indirect costs incurred as a result of bipolar I disorder. Indirect costs, such as productivity loss due to absenteeism or mortality, pose a substantial economic burden upon society. Because the accrual of indirect costs is associated with productivity loss (due to acute mood episodes or hospitalization), a treatment such as QTP that is able to reduce the number of episodes and days of hospitalization is likely to decrease the incremental cost-effectiveness ratio (ICER) and exaggerate cost savings.
While no study to date has assessed the cost- effectiveness of QTP in combination with Li/DVP in the maintenance treatment for bipolar I disorder in the US healthcare setting, three other economic evaluations of bipolar I disorder maintenance treatments have been published. Two of the three studies considered multiple comparators, and all three studies included olanzapine. McKendrick et al conducted a cost-effectiveness analysis from the perspective of the UK National Health Service of olanzapine compared with Li in the prevention of acute mood episodes in bipolar disorderCitation32. Their model estimated that in contrast to Li monotherapy, olanzapine significantly reduced the annual number of acute mood episodes per patient (difference of –0.23; 95% CI:–0.34 to –0.12) but did not significantly reduce costs (–£799; 95% CI: – £1,824 to £59) over a period of 1 year.
A second cost-effectiveness analysis evaluated Li monotherapy, valproate, olanzapine, and no maintenance treatment for bipolar I disorder in stabilized patients over a 5-year time horizonCitation26. Soares-Weiser et al reported that valproate dominated olanzapine, and that both valproate and Li dominated the no maintenance treatment option. The incremental cost-effectiveness analysis comparing valproate with Li resulted in an ICER of £260 and £341 per additional episode averted for men and women (without child bearing potential), respectively.
Lastly, Calvert et al conducted a cost-effectiveness analysis of Li monotherapy, lamotrigine, olanzapine, and no maintenance treatment for bipolar I disorder in stabilized patients over an 18-month time horizonCitation20. The authors reported that lamotrigine was the most effective treatment for avoiding all types of acute episodes and acute depression episodes. Olanzapine was found to be the most effective in preventing acute manic episodes. All maintenance treatments considered in the model were cost-effective compared with the ‘no maintenance treatment’ option. The base-case analysis showed that lamotrigine dominated olanzapine. Compared with Li, lamotrigine's incremental cost per episode avoided was $2,400, and the incremental cost per QALY was $26,000.
Together, these studies demonstrate wide variability in the efficacy of currently available maintenance treatments for bipolar I disorder. However, the use of different comparators, as well as differences in model time horizons, perspectives, and effectiveness measures, hinders the comparison of results across these studies.
Conclusion
The results of this economic evaluation suggest that maintenance treatment with QTP in combination with Li/DVP is a cost-effective alternative to treatment with Li/DVP alone. Specifically, the model indicates that treatment with QTP + Li/DVP, as compared with Li/DVP alone, results in lowers costs, higher QALYs, and a decrease in acute mood events and associated hospital admissions. These outcomes would reduce direct medical costs. Because bipolar I disorder is a chronic, episodic illness, the validity of this model must be confirmed as new evidence comes to light. Further research is needed to assess treatment patterns and clinical guidelines, as well as the long-term effects of maintenance treatment of bipolar I disorder.
Acknowledgments
Declaration of interest: This analysis of studies was supported by a research grant from AstraZeneca Pharmaceuticals LP, Wilmington, DE, USA.
The authors acknowledge the editorial assistance of Aruna Seth, PhD, PAREXEL MMS, supported by AstraZeneca.
References
- Brazier J, Roberts J, Deverill M. The estimation of a preference-based measure of health from the SF 36. J Health Econ 2002;21:271–292.
- Merikangas KR, Akiskal HS, Angst J, Lifetime and 12-month prevalence of bipolar spectrum disorder in the National Comorbidity Survey replication. Arch Gen Psychiatry 2007;64:543–552.
- Kleinman L, Lowin A, Flood E, Costs of bipolar disorder. Pharmacoeconomics 2003;21:601–622.
- Sharma R, Markar HR. Mortality in affective disorder. J Affect Disord 1994;31:91–96.
- Fiedorowicz JG, Palagummi NM, Forman-Hoffman VL, Elevated prevalence of obesity, metabolic syndrome, and cardiovascular risk factors in bipolar disorder. Ann Clin Psychiatry 2008;20:131–137.
- Ghaemi SN, Boiman EE, Goodwin FK. Diagnosing bipolar disorder and the effect of antidepressants: a naturalistic study. J Clin Psychiatry 2000;61:804–808; quiz 809.
- Wyatt RJ, Henter I. An economic evaluation of manic-depressive illness – 1991. Soc Psychiatry Psychiatr Epidemiol 1995;30:213–219.
- Begley CE, Annegers JF, Swann AC, The lifetime cost of bipolar disorder in the US: an estimate for new cases in 1998. Pharmacoeconomics 2001;19:483–495.
- Knoth RL, Chen K, Tafesse E. Datapoints: costs associated with the treatment of patients with bipolar disorder in a managed care organization. Psychiatr Serv 2004;55:1353.
- Practice guideline for the treatment of patients with bipolar disorder (revision). Am J Psychiatry 2002;159(4 Suppl):1–50.
- McIntyre RS, Woldeyohannes HO, Yasgur BS, Maintenance treatment in bipolar disorder: a focus on aripiprazole. Expert Rev Neurother 2007;7:919–925.
- Astrazeneca. Seroquel – Prescribing Information, 2007.
- Vieta E, Suppes T, Eggens I, Efficacy and safety of quetiapine in combination with lithium or divalproex for maintenance of patients with bipolar I disorder (international trial 126). J Affect Disord 2008;109:251–263.
- Suppes T, Liu S, Brecher M, Paulsson B, on behalf of the Trial 127 Investigators. Maintenance treatment in bipolar I disorder with quetiapine with lithium or divalproex: a placebo-controlled, randomized multicenter trial (trial D1447C00127). Bipolar Disord 2008;10(Suppl 1):40.
- Lipscomb J, Weinstein M, Torrance GW. Time preference. In: Gold MR, Siegel J, Russell LB, Weinstein MC, eds. Cost-effectiveness in Health and Medicine. New York, NY: Oxford University Press, 1996;214–246.
- Simon GE, Hunkeler E, Fireman B, Risk of suicide attempt and suicide death in patients treated for bipolar disorder. Bipolar Disord 2007;9:526–530.
- NCHS. National Vital Statistics Report. Deaths: Final Data for 2004.
- Fleurence RL, Hollenbeak CS. Rates and probabilities in economic modelling: transformation, translation and appropriate application. Pharmacoeconomics 2007;25:3–6.
- Calabrese JR, Bowden CL, Sachs G, A placebo-controlled 18-month trial of lamotrigine and lithium maintenance treatment in recently depressed patients with bipolar I disorder. J Clin Psychiatry 2003;64:1013–1024.
- Calvert NW, Burch SP, Fu AZ, The cost-effectiveness of lamotrigine in the maintenance treatment of adults with bipolar I disorder. J Manag Care Pharm 2006;12:322–330.
- Bowden CL, Calabrese JR, Sachs G, A placebo-controlled 18-month trial of lamotrigine and lithium maintenance treatment in recently manic or hypomanic patients with bipolar I disorder. Arch Gen Psychiatry 2003;60:392–400.
- Thomson P. Red Book [TM] for Windows (2007) Vol 43.
- US Department of Labor BoLS. Consumer price indexes: US Depart. of Labor, Bureau of Labor Statistics [on-line]. Available at: http://www.bls.gov/cpi/ [Last accessed 10 Oct 2007].
- Laupacis A, Feeny D, Detsky AS, Tugwell PX. How attractive does a new technology have to be to warrant adoption and utilization? Tentative guidelines for using clinical and economic evaluations CMAJ 1992;146:473–481.
- Briggs A, Gray A. Using cost-effectiveness information. BMJ 2000;320:246.
- Soares-Weiser K, Bravo Vergel Y, Beynon S, A systematic review and economic model of the clinical effectiveness and cost-effectiveness of interventions for preventing relapse in people with bipolar disorder. Health Technol Assess 2007;11: iii–iv, ix–206.
- Fleurence RL, Chatterton ML, Dixon JM, Rajagopalan K. Economic outcomes associated with atypical antipsychotics in bipolar disorder: a systematic review. Prim Care Companion J Clin Psychiatry 2007;9:419–428.
- Kessing LV, Munk-Jorgensen P. Does type of first contact in depressive and bipolar disorders predict subsequent hospitalisation and risk of suicide? J Affect Disord 2004;83:65–71.
- DeFrances CJ, Cullen KA, Kozak LJ. National hospital discharge survey: 2005 annual summary with detailed diagnosis and procedure data. Vital Health Stat 13, 2007 :Table 13.
- Revicki DA, Matza LS, Flood E, Lloyd A. Bipolar disorder and health-related quality of life: review of burden of disease and clinical trials. Pharmacoeconomics 2005;23:583–594.
- Revicki DA, Wood M. Patient-assigned health state utilities for depression-related outcomes: differences by depression severity and antidepressant medications. J Affect Disord 1998;48:25–36.
- McKendrick J, Cerri KH, Lloyd A, Cost-effectiveness of olanzapine in prevention of affective episodes in bipolar disorder in the United Kingdom. J Psychopharmacol 2007;21:588–596